2020 National ART Summary
Introduction
Data from clinics in the United States that use ART to treat infertility are a rich source of information about the factors that contribute to a successful ART treatment, which is the delivery of a healthy infant. Pooling the data from all reporting clinics provides a national picture that could not be obtained by examining data from an individual clinic.
This section includes data from the 449 US fertility clinics in operation in 2020 that provided and verified data on the outcomes of all ART cycles started in their clinics. ART cycles include any process in which (1) an ART procedure is performed, (2) a woman has undergone ovarian stimulation or monitoring with the intent of having an ART procedure, or (3) frozen embryos have been thawed with the intent of transferring them to a woman. For example, an ART cycle could include an embryo transfer from a previously frozen embryo. Another cycle could include stimulation, egg retrieval, and embryo transfer.
Of the 326,468 new ART cycles reported in 2020, a total of 203,164 (62%) were started with the intent to transfer at least one embryo. Among these 203,164 cycles, there were 165,041 embryo transfers. These embryo transfers resulted in 91,453 pregnancies, 75,023 live-birth deliveries (delivery of one or more living infants), and 79,942 infants. The other 123,304 cycles (38%) were banking cycles, where eggs or embryos were cryopreserved (frozen) and stored for potential future use. The 326,468 new ART cycles started in 2020 do not include 7 research cycles that were designed to evaluate a new treatment procedure.
A patient’s chances of having a pregnancy and live-birth delivery when using ART are influenced by many factors. Some of these factors are patient-related, such as the patient’s age or the cause of infertility. Others are clinic-related, such as a clinic’s patient selection practices.
Average chances, however, do not necessarily apply to a particular individual or couple. To help patients estimate their chance of having a baby through in vitro fertilization (IVF), the most common type of ART, CDC developed the IVF Success Estimator tool. This tool uses information about the experiences of women and couples with similar characteristics to estimate a person’s chance of having a baby. These estimates are based on the available data and may not be representative of an individual patient’s specific experience. In addition, the IVF Success Estimator does not provide medical advice, diagnosis, or treatment. Couples should talk with their doctor about their specific treatment plan and potential for success.
The National Summary Table in this section provides a full snapshot of clinic services, clinic profiles, patient characteristics, and ART success rates. It combines information from all individual clinic data summaries presented on CDC’s ART Fertility Clinic Success Rates website.
The National Summary Figures in this section include ART cycles started in 2020 as described above and provide information about patients who use ART, their reasons, and the types of procedures performed. They also provide data on pregnancy and infant outcomes and 10-year trends of the types of procedures performed and pregnancy outcomes. The figures include ART cycles that used fresh or frozen embryos from a female patient’s own eggs or eggs from another woman (donor eggs). The National Summary Figures are noncumulative and based only on ART cycles performed in 2020. They cannot be used to calculate cumulative success rates. For ART cycles performed in 2020, pregnancy outcomes may have occurred in 2020 or 2021.
National Summary Table: An accessible version of this table is available on the Assisted Reproductive Technology (ART) Data website under the Clinic Data Summary tab.
DISCLAIMER: Patient medical characteristics, such as age, diagnosis, and ovarian reserve, affect the success of ART treatment. Comparison of success rates across clinics may not be meaningful due to differences in patient populations and ART treatment methods. The success rates displayed here do not reflect any one patient’s chance of success. Patients should consult with a doctor to understand their chance of success based on their own characteristics.
Cumulative ART Success Rates for Intended Retrievals Among Patients Using Their Own Eggsa,b,c | Number of reporting clinics: 449
| Patient Age | ||||
|---|---|---|---|---|
| <35 | 35–37 | 38– 40 | >40 | |
| All patients (with or without prior ART cycles) | ||||
| Number of intended retrievals | 53,163 | 32,979 | 32,490 | 29,703 |
| Percentage of intended retrievals resulting in live-birth deliveries | 51.1% | 37.1% | 23.7% | 7.6% |
| Percentage of intended retrievals resulting in singleton live-birth deliveries | 47.2% | 34.6% | 22.1% | 7.2% |
| Number of retrievals | 50,222 | 30,120 | 28,609 | 24,313 |
| Percentage of retrievals resulting in live-birth deliveries | 54.1% | 40.6% | 26.9% | 9.3% |
| Percentage of retrievals resulting in singleton live-birth deliveries | 50.0% | 37.9% | 25.1% | 8.8% |
| Number of transfers | 54,572 | 26,895 | 19,075 | 9,482 |
| Percentage of transfers resulting in live-birth deliveries | 49.8% | 45.5% | 40.4% | 23.9% |
| Percentage of transfers resulting in singleton live-birth deliveries | 46.0% | 42.4% | 37.7% | 22.6% |
| Average number of intended retrievals per live-birth delivery | 2.0 | 2.7 | 4.2 | 13.1 |
| New patients (with no prior ART cycles) | ||||
| Percentage of new patients having live-birth deliveries after 1 intended retrieval | 55.1% | 40.5% | 26.4% | 8.2% |
| Percentage of new patients having live-birth deliveries after 1 or 2 intended retrievals | 60.8% | 47.4% | 33.1% | 11.2% |
| Percentage of new patients having live-birth deliveries after all intended retrievals | 61.8% | 48.8% | 35.3% | 12.5% |
| Average number of intended retrievals per new patient | 1.2 | 1.3 | 1.4 | 1.5 |
| Average number of transfers per intended retrieval | 1.1 | 0.8 | 0.6 | 0.3 |
Noncumulative ART Success Rates for Transfers Among Patients Using Eggs or Embryos from a Donor or Donated Embryoa,b,c,d
| Fresh Embryos Fresh Eggs |
Fresh Embryos Frozen Eggs |
Frozen Embryos |
Donated Embryos |
|
|---|---|---|---|---|
| Number of transfers | 1,104 | 2,391 | 14,951 | 2,705 |
| Percentage of transfers resulting in live-birth deliveries | 54.7% | 47.4% | 47.7% | 40.9% |
| Percentage of transfers resulting in singleton live-birth deliveries | 49.5% | 44.1% | 44.5% | 36.0% |
Characteristics of ART Cyclesa,b
| Patient Age | |||||
|---|---|---|---|---|---|
| <35 | 35–37 | 38– 40 | >40 | Total | |
| Total number of cycles | 121,539 | 76,129 | 65,365 | 63,435 | 326,468 |
| Percentage of intended egg retrieval cycles without any eggs retrievede | 5.0% | 7.2% | 10.1% | 14.2% | 8.4% |
| Percentage of cycles discontinued after retrieval and before transfer or bankingf | 9.9% | 10.4% | 13.2% | 19.4% | 12.5% |
| Percentage of cycles for fertility preservation | 7.4% | 9.5% | 7.8% | 4.3% | 7.4% |
| Percentage of transfers using a gestational carrier | 2.9% | 3.7% | 4.6% | 10.3% | 4.7% |
| Percentage of transfers using frozen embryos | 81.4% | 83.6% | 82.4% | 78.3% | 81.6% |
| Percentage of transfers of at least 1 embryo with ICSI | 80.5% | 79.2% | 77.2% | 68.4% | 77.4% |
| Percentage of transfers of at least 1 embryo with PGT | 43.0% | 52.9% | 54.6% | 46.0% | 48.0% |
Current Services and Profile (percentage of clinics)
| Donor eggs? | 89% |
| Donated embryos? | 63% |
| Embryo cryopreservation? | 100% |
| Egg cryopreservation? | 99% |
| Gestational carriers? | 90% |
| SART member? | 80% |
| Verified lab accreditation | Yes | No | Pending |
| 88% | 10% | 2% |
Reason for Using ARTa,b,g
| Male factor | 28% |
| Endometriosis | 7% |
| Tubal factor | 11% |
| Ovulatory dysfunction | 14% |
| Uterine factor | 6% |
| PGT | 16% |
| Gestational carrier | 2% |
| Diminished ovarian reserve | 28% |
| Egg or embryo banking | 38% |
| Recurrent pregnancy loss | 6% |
| Other factor, infertility | 28% |
| Other factor, non-infertility | 5% |
| Unexplained factor | 10% |
ART = assisted reproductive technology; ICSI = intracytoplasmic sperm injection; PGT = preimplantation genetic testing (diagnosis or screening); SART = Society for Assisted Reproductive Technology.
a Numbers and percentages exclude 7 research cycles that were evaluating new procedures.
b Fractions are used when the denominator is less than 20. Reported sample sizes of 1 through 4 were suppressed due to small sample size.
c A live birth is defined as the delivery of one or more infants with at least one born alive. Multiple-birth deliveries (such as twins) with at least one live-born infant are counted as one live birth. Success rates for cycles using a patient’s own eggs are calculated by using all cycles started in 2019 with the intent to retrieve a patient’s eggs and all transfers of embryos created from these eggs started within 12 months of the start of the retrieval cycle. Success rates for cycles using a donor’s eggs or donated embryos are calculated by using all transfers started in 2020.
d Patients of all ages are combined because previous data show that a patient’s age does not substantially affect success when using a donor’s eggs or donated embryos.
e Includes cycles in which no eggs were retrieved among all cycles in which egg retrieval was intended.
f Includes cycles in which no eggs or embryos were transferred or frozen among all cycles in which eggs were retrieved and all frozen cycles.
g Reasons may add to more than 100% because more than one diagnosis can be reported for each ART cycle.
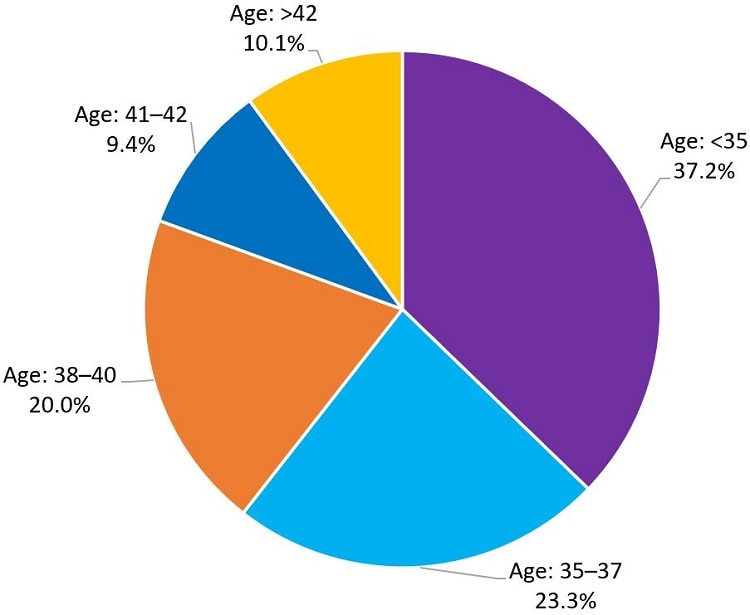
Figure 1 shows the distribution of the 326,468 ART cycles started in 2020 in the United States, by patient age group. The largest percentage of ART cycles performed was among patients younger than age 35. This age group represented 37.2% of all cycles, compared to 23.3% among patients aged 35–37, 20.0% among those aged 38–40, 9.4% among those aged 41–42, and 10.1% among those older than age 42. The average age of patients using ART services in 2020 was 36.2 years.
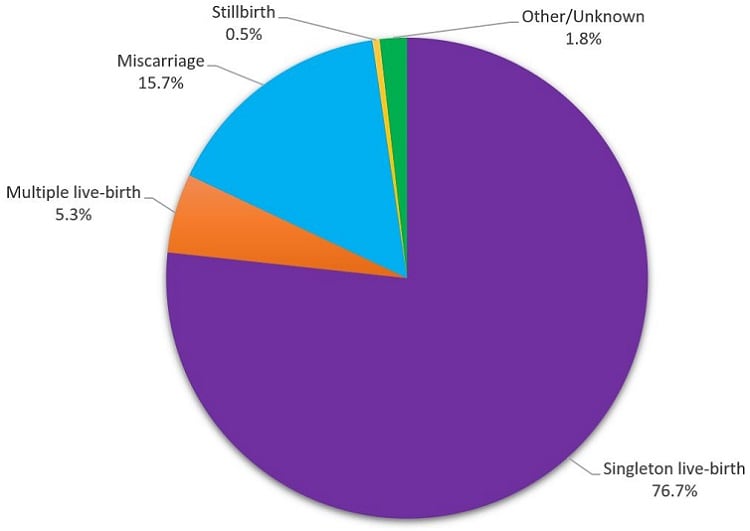
Figure 2 shows the outcomes of the 91,453 clinical pregnancies from ART cycles started in 2020. A clinical pregnancy is a pregnancy that is confirmed by ultrasound. About 82% of clinical pregnancies from ART cycles started in 2020 resulted in a live-birth delivery. Of clinical pregnancies, 76.7% resulted in the birth of a single infant, while 5.3% resulted in the birth of multiple infants. Clinical pregnancies that did not result in a live-birth delivery included miscarriage (15.7%) and stillbirth (0.5%). For 1.8% of pregnancies, the outcome was reported as other or unknown.
Fresh and frozen eggs or embryos from patients and donors are included. Banking cycles are excluded.
Both miscarriage and stillbirth describe pregnancy loss, but they are categorized according to when the loss occurs. Miscarriage (also called spontaneous abortion) is a pregnancy ending in the spontaneous loss of the embryo or fetus before 20 weeks of gestation. Stillbirth, or fetal death, is pregnancy loss at 20 weeks or more of gestation.
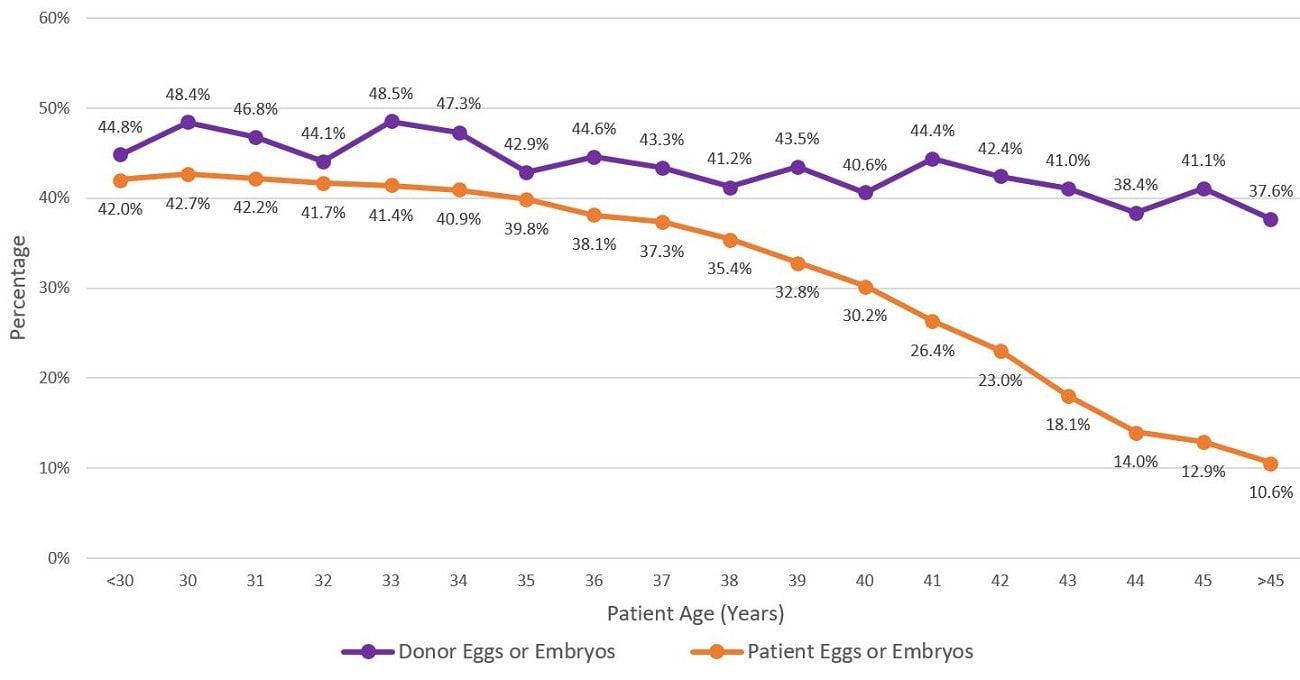
Figure 3 shows the percentage of embryo transfer cycles started in 2020 that resulted in live-birth delivery of one or more live infants, by patient age and egg or embryo source.
Fresh and frozen eggs or embryos from patients and donors are included. Banking cycles are excluded.
The percentage of embryo transfer cycles that used patient eggs or embryos and resulted in live-birth delivery generally decreased as the age of the woman increased (range: 10.6%–42.7%) because the likelihood of a fertilized egg implanting is related to the age of the woman who produced the egg. In contrast, 41.4% of embryo transfer cycles using donor eggs or embryos resulted in live-birth delivery for women of all ages (range: 37.6%–48.5%) because egg donors are typically in their 20s or early 30s and do not have infertility.
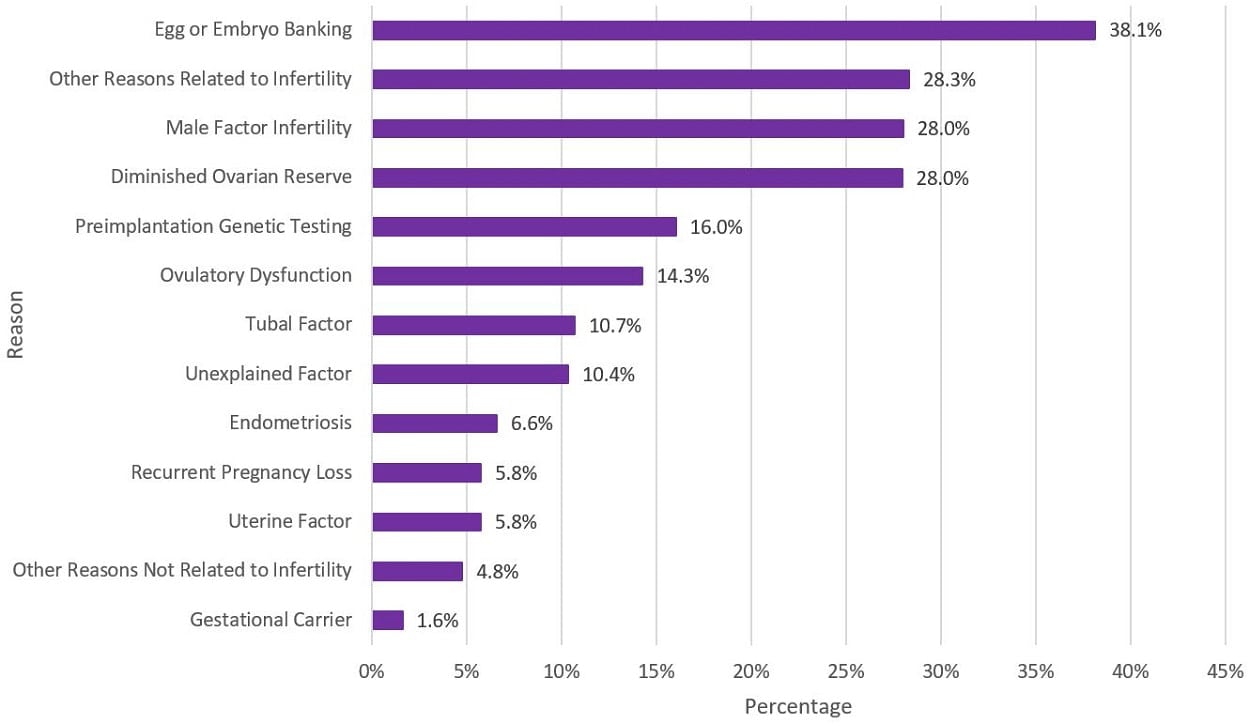
Figure 4 shows the distribution of reported reasons for ART cycles started in 2020. Percentages for each reason were as follows: 38.1% for egg or embryo banking, 28.3% for other reasons related to infertility, 28.0% for male factor infertility, 28.0% for diminished ovarian reserve, 16.0% for preimplantation genetic testing, 14.3% for ovulatory dysfunction, 10.7% for tubal factor, 10.4% for unexplained factor, 6.6% for endometriosis, 5.8% for recurrent pregnancy loss, 5.8% for uterine factor, 4.8% for other reasons not related to infertility, and 1.6% for gestational carrier. Because more than one reason can be reported per cycle, the total percentage adds to more than 100%.
Fresh and frozen eggs or embryos from patients and donors are included. Banking cycles are included.
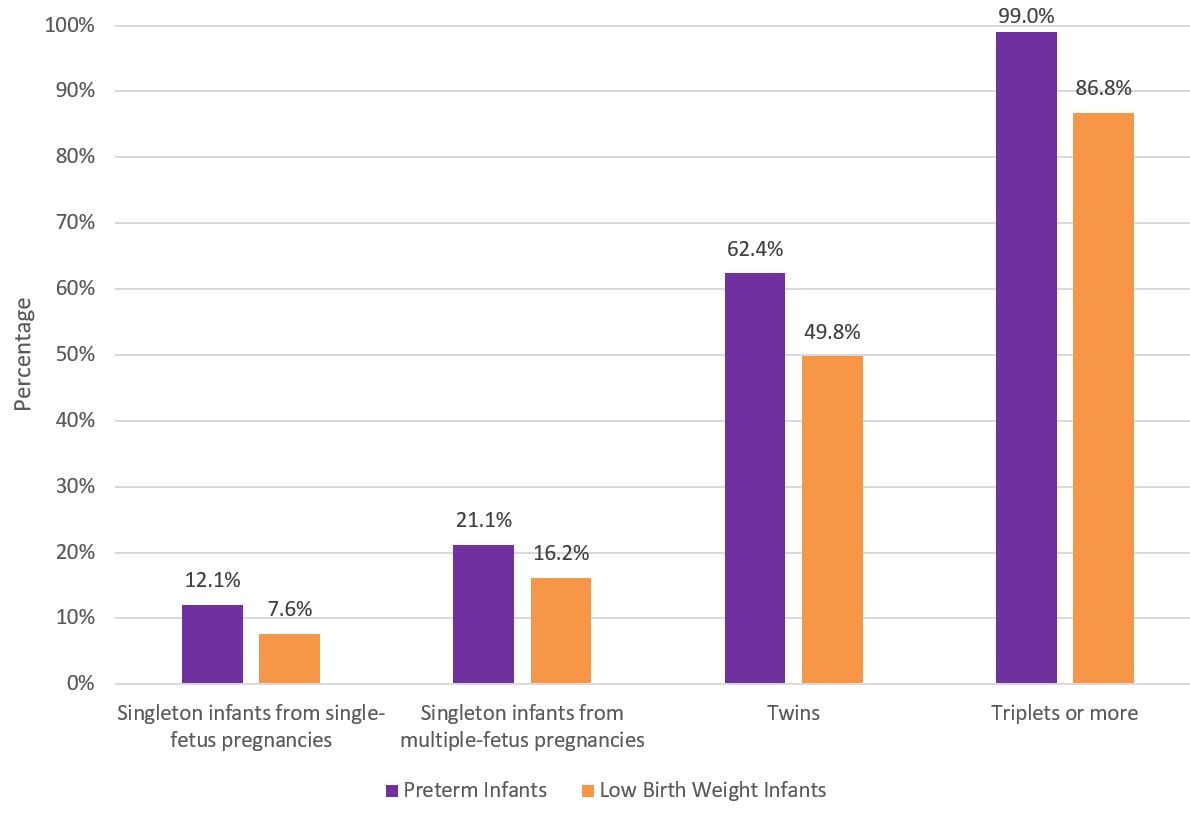
Figure 5 shows the percentage of infants born from ART procedures started in 2020 who were born preterm or with low birth weight. This figure presents percentages for deliveries that resulted in a single live-born infant (separately for single-fetus and multiple-fetus pregnancies), twin live-born infants, and triplet or more live-born infants. Multiple-fetus pregnancies were more likely to result in infants being born preterm or with low birth weight. For example, 12.1% of single infants from single-fetus pregnancies were preterm, compared to 21.1% of single infants from multiple-fetus pregnancies. Percentages of preterm and low birth weight infants increased as the number of infants born (live or still) in one delivery increased. Among triplets or more, 99.0% were preterm and 86.8% had low birth weight.
Fresh and frozen eggs or embryos from patients and donors are included. Banking cycles are excluded.
Preterm infants are born before 37 full weeks of pregnancy. Low birth weight infants are born weighing less than 2,500 grams (about 5 pounds, 8 ounces). Infants born preterm or with low birth weight are at higher risk of death in the first year of life. They also have a higher risk of other poor health outcomes, including visual and hearing problems, intellectual and learning disabilities, and behavioral and emotional problems throughout life.
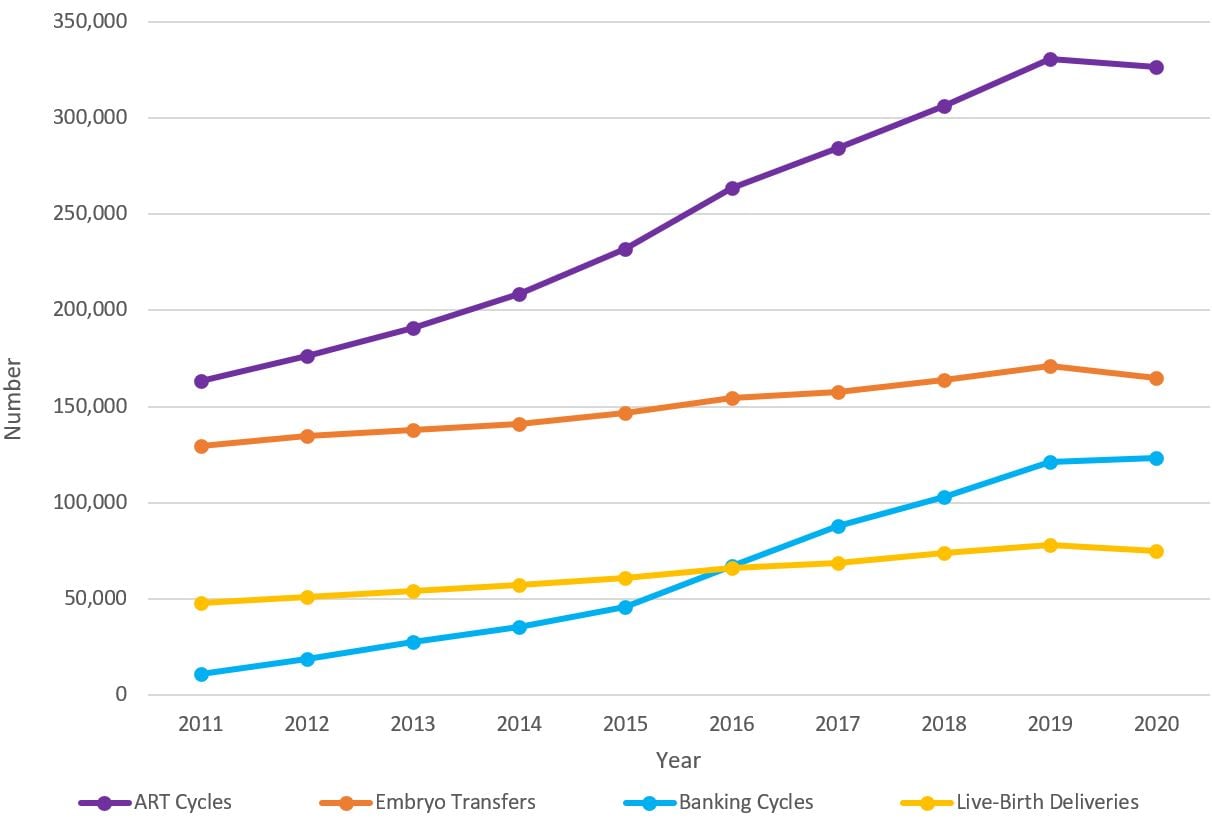
Figure 6 shows the number of ART cycles, embryo transfer cycles, and banking cycles performed and the number of live-birth deliveries that resulted from ART cycles started from 2011 through 2020. Over the last decade, the number of ART cycles started has doubled, from 163,045 cycles in 2011 to 326,468 in 2020. Banking cycles also increased, from 11,116 in 2011 to 123,304 in 2020. The number of embryo transfer cycles in 2020 (165,041) was about 1.3 times higher than in 2011 (129,360). The number of live-birth deliveries in 2020 (75,023) was about 1.6 times higher than in 2011 (47,850).
Fresh and frozen eggs or embryos from patients and donors are included.
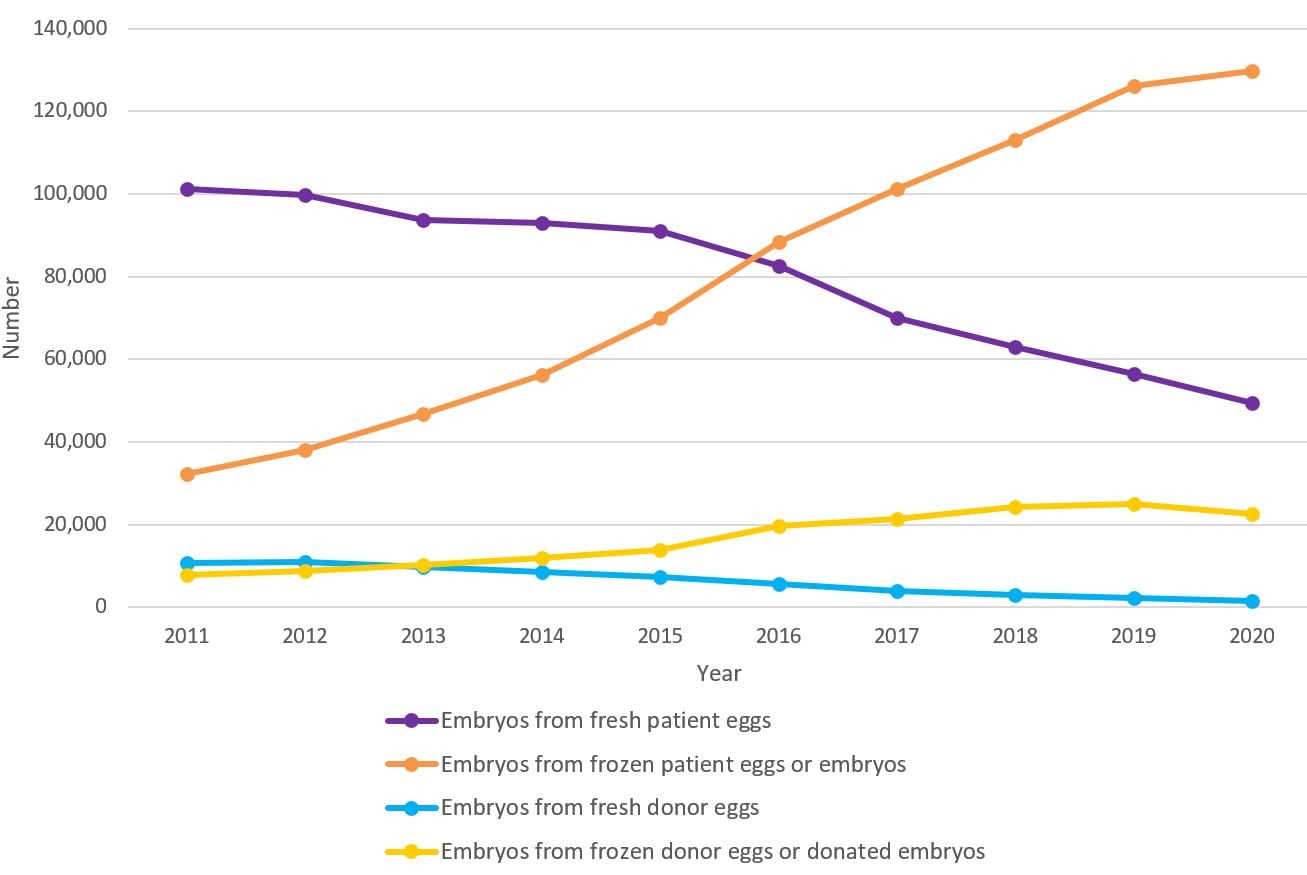
Figure 7 shows the number of ART cycles started by egg or embryo source and type, from 2011 through 2020. The number of cycles performed using embryos from fresh patient eggs decreased from 101,213 in 2011 to 49,432 in 2020. The number of cycles performed using embryos from frozen patient eggs or embryos increased from 32,180 in 2011 to 129,692 in 2020.
The number of cycles performed using embryos from fresh donor eggs decreased from 10,797 in 2011 to 1,477 in 2020. The number of cycles performed using embryos from frozen donor eggs or donated embryos increased from 7,733 in 2011 to 22,563 in 2020.
Fresh and frozen eggs or embryos from patients and donors are included. Banking cycles are excluded.
Embryos from fresh patient eggs are patient embryos from fresh eggs that were transferred without being frozen. Embryos from fresh donor eggs are donor embryos from fresh donor eggs that were transferred without being frozen. Embryos from frozen patient eggs or embryos are patient embryos that involved freezing at some point after retrieval of the egg. They include fresh embryos from frozen eggs or frozen embryos. Embryos from frozen donor eggs or donated embryos are donor embryos that involved freezing at some point after retrieval of the egg. They include fresh embryos from frozen donor eggs, frozen embryos, or donated embryos.
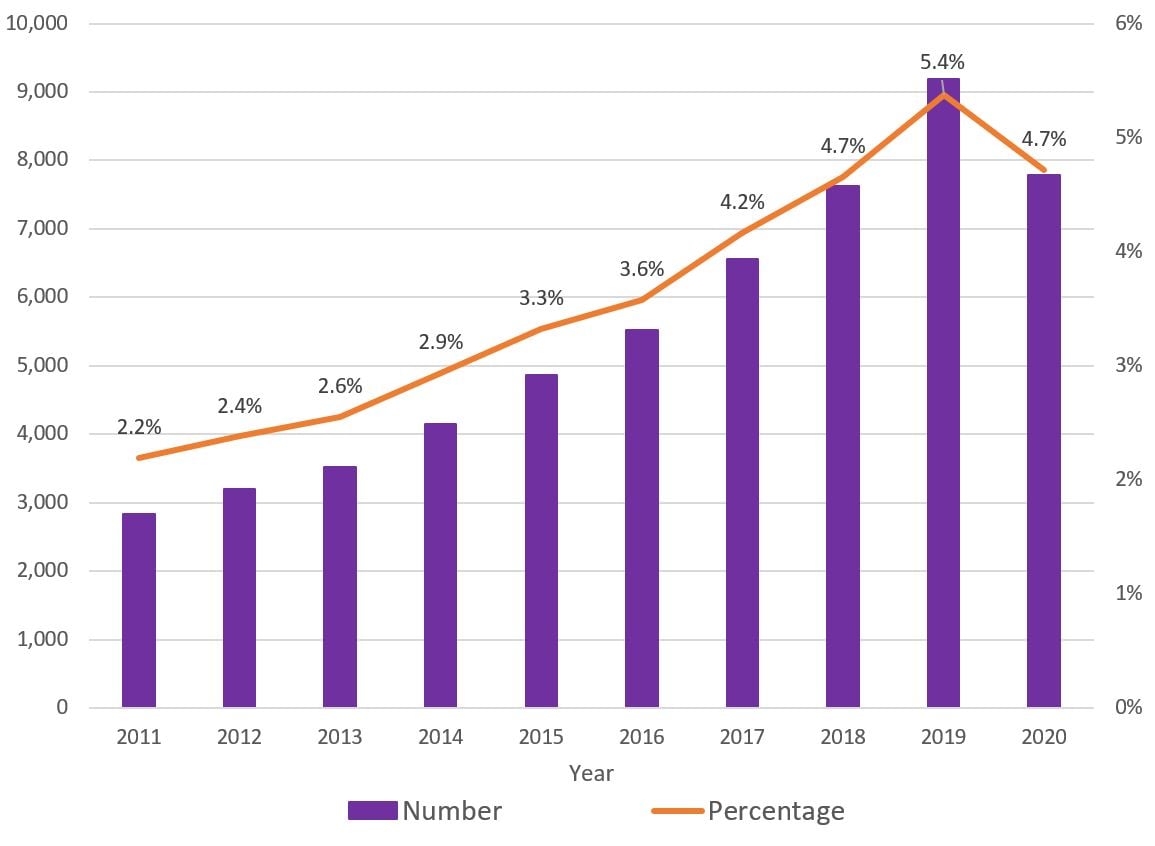
Figure 8 shows the number and percentage of embryo transfer cycles that used a gestational carrier, from 2011 through 2020. Over the last decade, the number of embryo transfer cycles that used a gestational carrier increased, from 2,841 in 2011 to 9,195 in 2019, with a decrease in 2020 (7,786). The percentage of transfers using a gestational carrier among all ART cycles also increased, from 2.2% of all ART cycles in 2011 to 5.4% in 2019, with a decrease in 2020 (4.7%).
Fresh and frozen eggs or embryos from patients and donors are included. Banking cycles are excluded.
A gestational carrier (also called a gestational surrogate) is a woman who agrees to carry a developing embryo created from another woman’s egg.
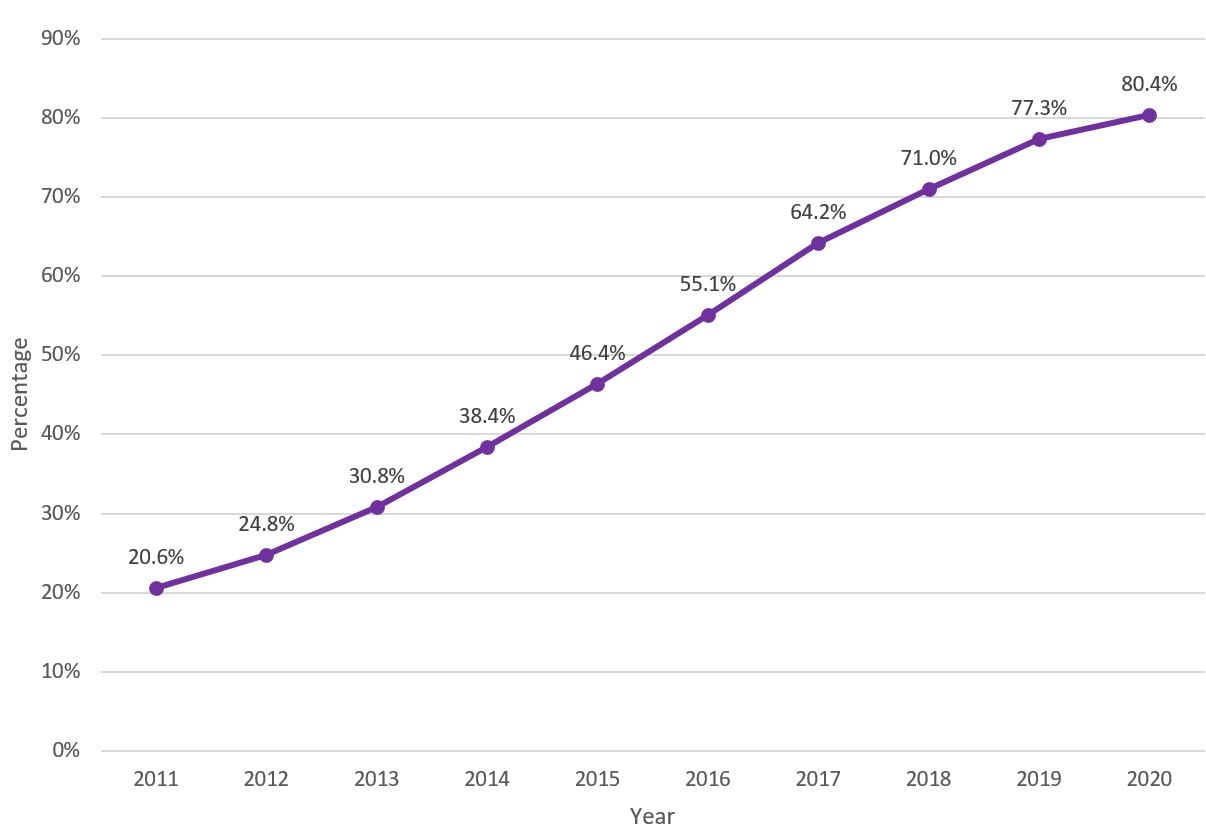
Figure 9 shows the percentage of embryo transfer cycles in which a single embryo was transferred, from 2011 through 2020. The percentage of single embryo transfer (SET) procedures is the percentage of all embryo transfer cycles in which only one embryo is transferred to the uterus, regardless of the number of embryos available. Over the last decade, the percentage of SET among all patients increased dramatically, from 20.6% in 2011 to 80.4% in 2020, and this trend was identified among all age groups [not shown].
Fresh and frozen eggs or embryos from patients and donors are included. Banking cycles are excluded.
The use of SET is a strategy to avoid a multiple-fetus pregnancy and reduce the risk of poor health outcomes, such as prematurity and low birth weight, among infants.
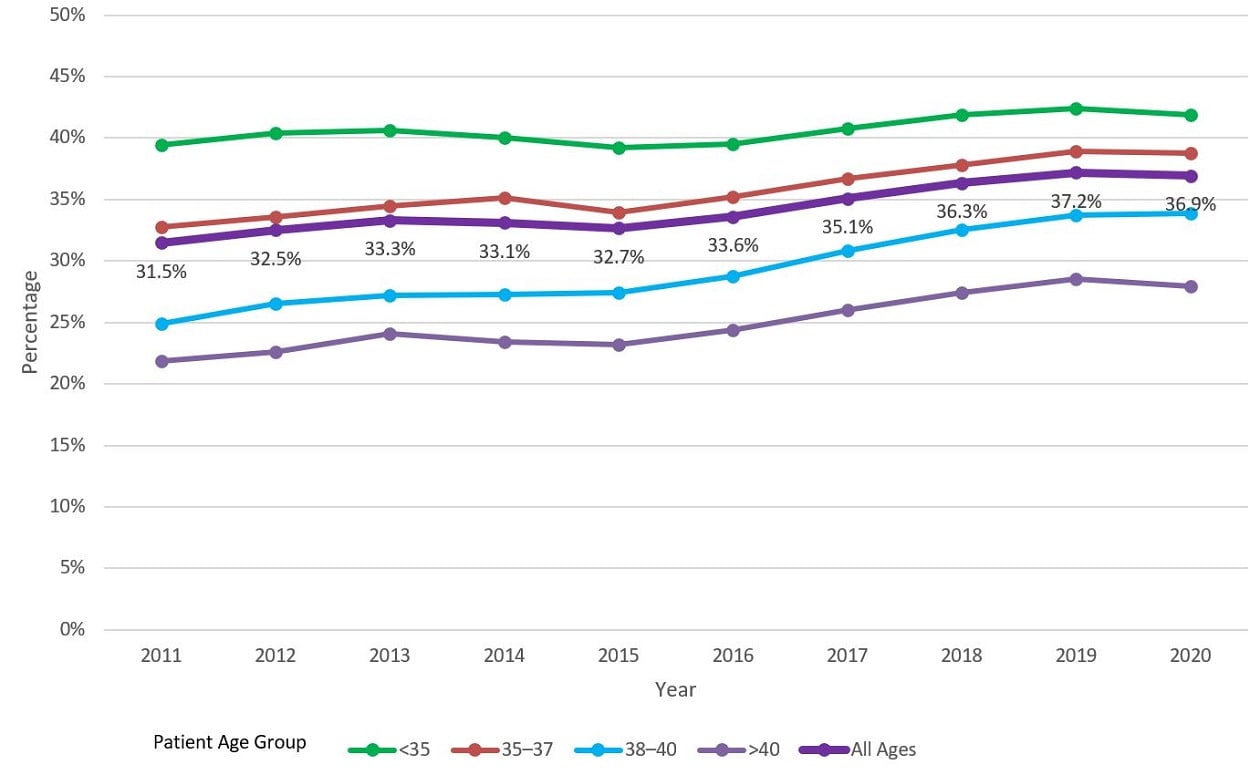
Figure 10 shows the percentage of ART cycles that resulted in live-birth deliveries by patient age group, from 2011 through 2020. For all age groups combined, percentages increased from 31.5% in 2011 to 36.9% in 2020. Percentage increased from 39.4% in 2011 to 41.9% in 2020 for patients younger than age 35, from 32.8% in 2011 to 38.7% in 2020 for patients aged 35 to 37, from 24.9% in 2011 to 33.9% in 2020 for patients aged 38 to 40, and from 21.9% in 2011 to 27.9% in 2020 for patients older than age 40.
Fresh and frozen eggs or embryos from patients and donors are included. Banking cycles are excluded.
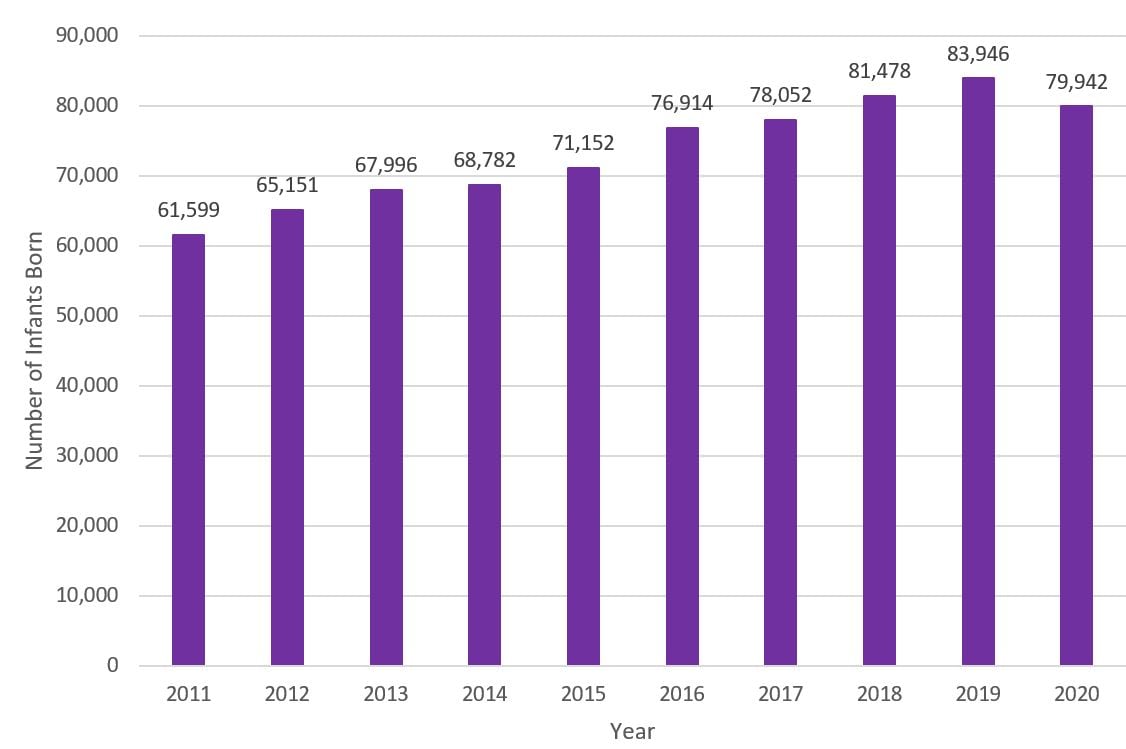
Figure 11 shows the number of infants born from 2011 through 2020 who were conceived using ART. The number of infants born who were conceived using ART increased from 61,599 in 2011 to 83,946 in 2019, with a decrease in 2020 (79,942).
Fresh and frozen eggs or embryos from patients and donors are included. Banking cycles are excluded.
Because more than one infant can be born during a live-birth delivery (such as twins), the total number of infants born is higher than the number of live-birth deliveries.
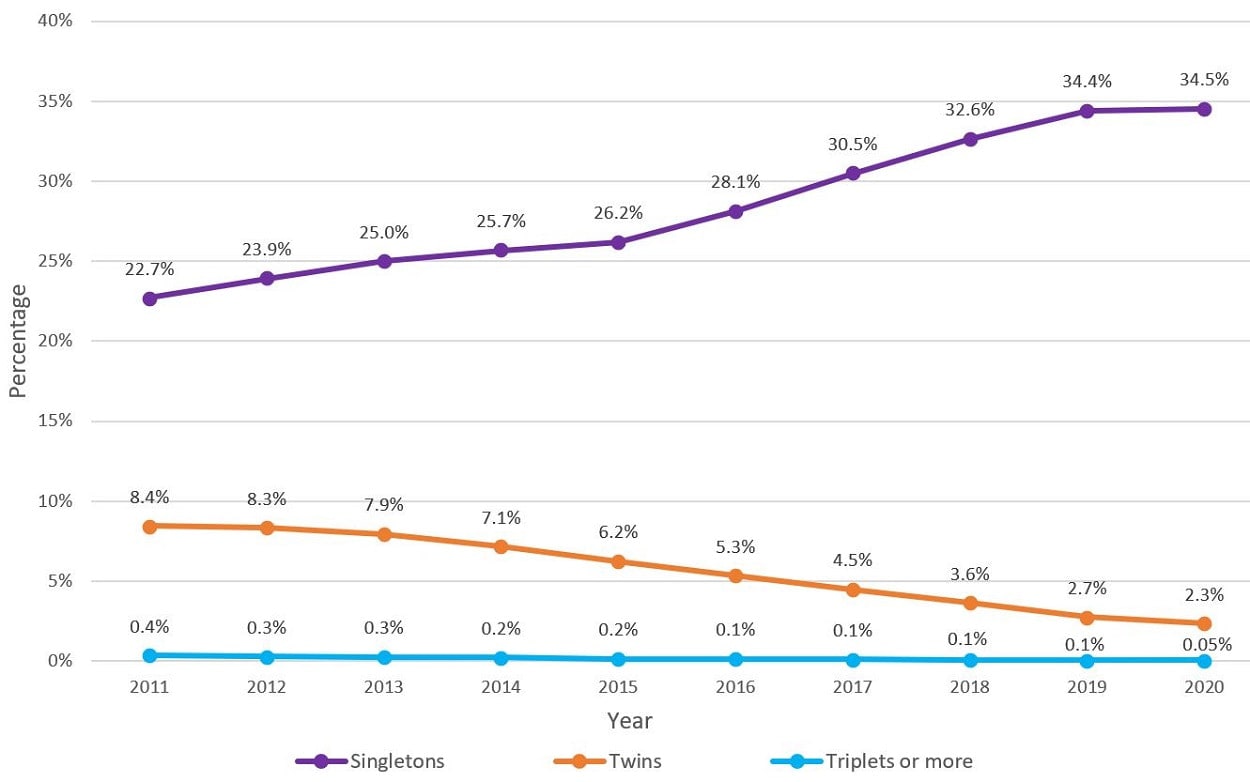
Figure 12 shows the percentage of embryo transfer cycles that resulted in the live-birth delivery of singletons, twins, or triplets or more, from 2011 through 2020. Over the last decade, the percentage of embryo transfer cycles that resulted in singleton births increased from 22.7% in 2011 to 34.5% in 2020, while the percentage that resulted in multiple births decreased. The percentage of twins decreased from 8.4% in 2011 to 2.3% in 2020, while the percentage of triplets or more decreased from 0.4% in 2011 to 0.05% in 2020.
Fresh and frozen eggs or embryos from patients and donors are included. Banking cycles are excluded.
The increased use of single embryo transfer (SET) in recent years has likely contributed to this trend. SET is used to avoid multiple-fetus pregnancies and reduce the risk of poor health outcomes, such as prematurity and low birth weight, among infants.
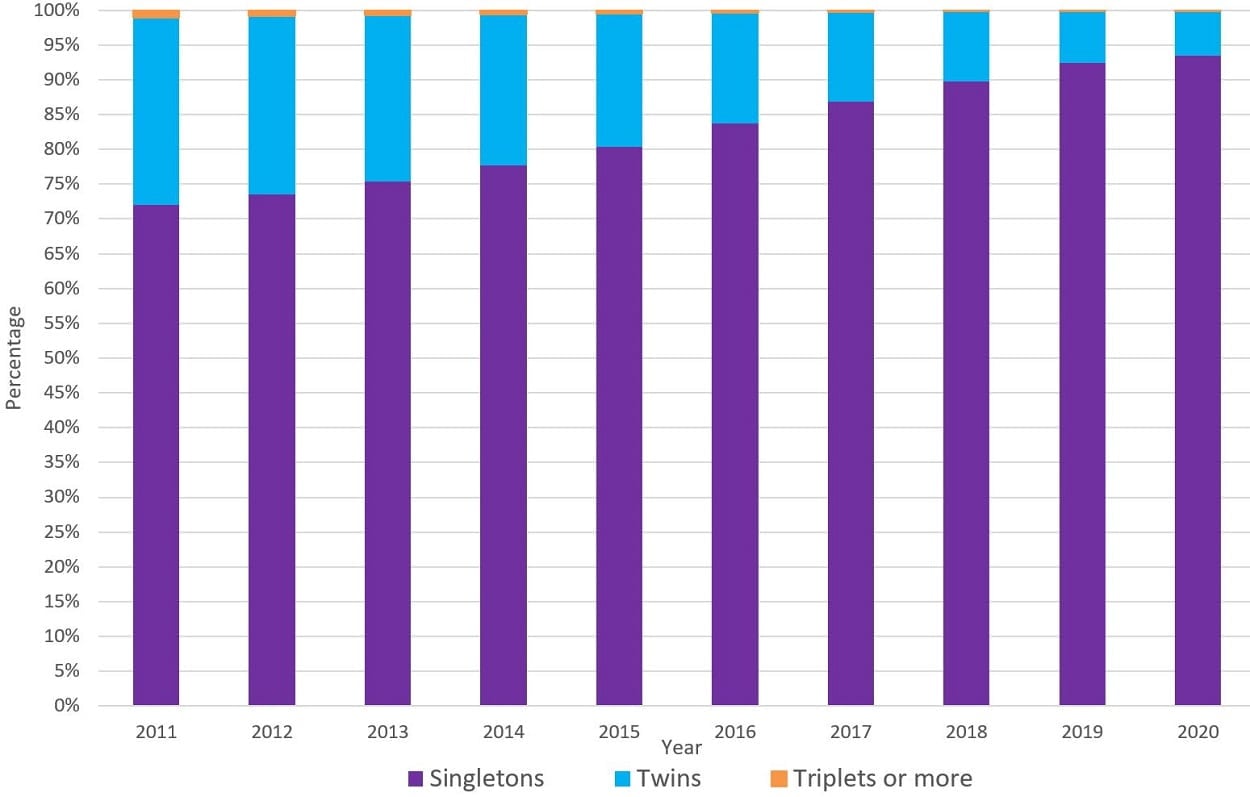
Figure 13 shows the percentage of infants who were conceived using ART cycles that resulted in the live-birth delivery of singletons, twins, or triplets or more, from 2011 through 2020. Over the last decade, the percentage of ART-conceived live-birth deliveries that resulted in singletons increased from 72.1% in 2011 to 93.5% in 2020. The percentage that resulted in twins decreased from 26.8% in 2011 to 6.4% in 2020, while the percentage that resulted in triplets or more decreased from 1.1% to 0.1%.
Fresh and frozen eggs or embryos from patients and donors are included. Banking cycles are excluded.
Infants born from multiple gestations, including twins, are at higher risk of poor outcomes—including preterm birth, low birth weight, neurological impairments, or death—than infants born as singletons.