Antibiotic Use in the United States, 2022 Update: Progress and Opportunities
Introduction
Antibiotic stewardship is the effort to improve how antibiotics are prescribed and utilized across all healthcare settings and in all communities. Although antibiotics do not work against viruses like SARS-CoV-2 (the virus that causes COVID-19), antibiotics have been frequently prescribed for patients with COVID-19 during the pandemic. A CDC study reported that among Medicare beneficiaries who had an outpatient visit for COVID-19, more than 30% received an antibiotic, and most prescriptions were for azithromycin.1 Frequent prescribing of antibiotics used for treatment of community-acquired pneumonia among hospitalized patients and nursing home residents has also been observed during the COVID-19 pandemic, highlighting new opportunities to improve antibiotic use.
New Findings from CDC Studies
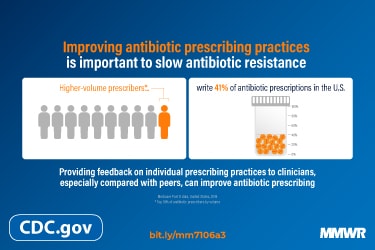
CDC examined antibiotic prescribing and factors that influence prescribing practices such as provider type, geographic location, setting, and patient age to inform targets for antibiotic stewardship. A Mortality and Morbidity Weekly Report [PDF – 4 pages] (MMWR) published in February 2022 evaluated publicly available data to better understand how antibiotics were prescribed for older adults (>65 years) in 2019. 2 The highest 10% of antibiotic prescribers prescribed 41% of total antibiotic prescriptions. Publicly available data can be used by public health organizations and healthcare systems to guide antibiotic stewardship interventions and optimize antibiotic prescribing to minimize antibiotic-associated adverse events and improve patient outcomes.
A study using machine-learning modeling examined drivers of inappropriate antibiotic prescribing for acute respiratory illnesses (IQVIA Medical Claims Data (Dx) and the IQVIA Longitudinal Prescription Data (LRx)).3 Antibiotics were prescribed in 11% of 42 million visits, and outpatient setting type, particularly urgent care, older patient age mix, and state location in the South were identified as top drivers of inappropriate prescribing. These findings give antibiotic stewards an opportunity to target education and resources to places where they are likely to have the most impact.
CDC collects, analyzes, and publishes data to inform antibiotic stewardship efforts in state and local jurisdictions and healthcare facilities.
Hospital Antibiotic Stewardship
CDC’s Core Elements of Hospital Antibiotic Stewardship provides a framework for implementation of antibiotic stewardship programs and are used by partners across the country. The implementation of antibiotic stewardship programs in acute care hospitals is assessed through the National Healthcare Safety Network’s (NHSN) Patient Safety Component Annual Hospital Survey [PDF – 19 pages]. Annual surveys are completed by staff in hospitals, and survey questions relating to antibiotic stewardship gauge a hospital’s uptake of CDC’s Core Elements of Hospital Antibiotic Stewardship Programs (ASPs). The percentage of hospitals meeting all 7 Core Elements increased to 94.9% in 2021. Additionally, hospitals meeting 6 of the 7 Core Elements is 98.1%.
Priorities for Hospital Core Element Implementation: Opportunities to Enhance Hospital Antibiotic Stewardship Programs
CDC is releasing the Priorities for Hospital Core Element Implementation to highlight a subset of implementation approaches that are highly effective and/or were prioritized by stewardship experts. The Priorities for Hospital Core Element Implementation are derived from the 2019 Hospital Core Elements and were identified for six of the seven Hospital Core Elements. The goal of the Priorities is to enhance the quality and impact of antibiotic stewardship programs.
NHSN Antimicrobial Use (AU) Option
The Antimicrobial Use (AU) Option of the CDC ’s NHSN is a surveillance resource that can provide actionable data for antibiotic stewardship programs. The data can be used to measure AU across hospitals and before, during, and after stewardship interventions. The NHSN AU data, in addition to other data sources, were used to characterize antibiotic use during the COVID-19 pandemic to identify opportunities for improvement. More than 2,400 acute care hospitals across the United States have submitted at least one month of data to the AU Option as of August 2022. Of those hospitals, 2,283 reported in the past 12 months (July 2021 – June 2022).
The growth in voluntary reporting suggests that hospitals are finding benefits in reporting and using this data. This growth, coupled with the growing recognition of the importance of national data on hospital antibiotic use and resistance prompted the Centers for Medicare and Medicaid Services to include a requirement for this reporting in their fiscal year 2023 Inpatient Prospective Payment System final rule. Reporting antimicrobial use and resistance data will be included in the Public Health and Clinical Data Exchange Objective as a required measure beginning with the EHR reporting period in CY 2024.
Standardized Antimicrobial Administration Ratio (SAAR)
One output measure included in NHSN’s AU Option of the Antimicrobial Use and Resistance (AUR Module) is the Standardized Antimicrobial Administration Ratio (SAAR). The SAAR is a risk-adjusted benchmarking measure of antibiotic use that can help inform stewardship efforts by enabling hospitals to see how their antibiotic use compares to other facilities. The 2021 NHSN AU Option Report provides a summary of SAAR distributions and percentages of use within the SAAR antimicrobial agent categories in adult, pediatric and neonatal patient care locations. Data on inpatient antibiotic use is available on the CDC’s Antibiotic Resistance & Patient Safety Portal.
Outpatient Antibiotic Use
Outpatient antibiotic prescribing decreased overall during the pandemic, but prescribing rates still vary widely across the United States; some states in the South have prescribing rates more than double rates in states in other regions. Variation in outpatient antibiotic use suggests that there are stewardship opportunities for healthcare providers, facility and healthcare system leadership, and other partners to improve how antibiotics are used. Monitoring of outpatient antibiotic prescribing data is regularly conducted by CDC to better understand trends in outpatient antibiotic prescribing, identify where interventions to improve prescribing are most needed, and measure progress.
Outpatient antibiotic prescriptions can be viewed by year, age, antibiotic, antibiotic class, and provider specialty (IQVIA Xponent data and U.S. Census files). These data reflect oral antibiotic prescriptions dispensed to humans in U.S. outpatient pharmacies during 2021.
Outpatient Antibiotic Prescribing During the COVID-19 Pandemic — United States, January 2019– October 20214
Monthly outpatient antibiotic prescriptions dispensed from retail pharmacies during the COVID-19 pandemic were compared to corresponding months in 2019 using the IQVIA National Prescription Audit (NPA) dataset. During March 2020 to October 2021, the overall volume of antibiotic prescriptions was lower than the corresponding months in January – December 2019. The lowest volume of outpatient antibiotic prescriptions occurred during May 2020 (40% lower than May 2019), with greatest decreases seen among children 0-19 years of age. One notable exception to this finding was an increase in the volume of antibiotic prescriptions for azithromycin, which exceeded 2019 levels in July 2021 (11% higher than 2019) and August 2021 (35% higher than 2019), likely reflecting inappropriate prescribing for COVID-19. These data highlight the impact of the COVID-19 pandemic on outpatient antibiotic prescribing and ongoing opportunities for improvement.
Nursing Home Antibiotic Use
Tracking and reporting antibiotic use in nursing homes is critical to monitor trends in antibiotic prescribing, inform opportunities to guide practice change, and evaluate the impact of stewardship interventions. CDC researchers evaluated the utility of electronic health record data to monitor antibiotic use and characterized antibiotic prescribing practices. Electronic health record data can be leveraged to support nursing homes in tracking and reporting antibiotic use.
Description of antibiotic use variability among US nursing homes using electronic health record data | Antimicrobial Stewardship & Healthcare Epidemiology | Cambridge Core
Electronic health record antibiotic orders in 1,664 U.S. nursing homes were used to describe antibiotic use at the facility and national levels.5 In 2016, 54% of residents received an antibiotic. The antibiotic use rate was 88 days of therapy (DOT) per 1,000 resident days and the median antibiotic course duration was 7 days (interquartile range, 5–10). Antibiotic use rates varied considerably across nursing homes and were only partially explained by nursing home and resident characteristics, highlighting potential opportunities for targeted improvement of prescribing practices.
Resources
CDC’s Core Elements of Antibiotic Stewardship offer healthcare professionals and antibiotic stewardship leaders a framework to guide efforts to optimize antibiotic use and improve patient outcomes. These frameworks complement existing guidelines and standards from key healthcare partner organizations. Core Elements implementation resources are available for hospitals, outpatient facilities, and nursing homes.
New and updated antibiotic stewardship resources for healthcare professionals, facilities, and partners:
- 5 Ways Community Pharmacists Can Be Antibiotics Aware
- Nursing Home Professionals: Effective Communication Toolkit [PDF – 3 pages]
- Healthcare Professionals: Be Antibiotics Aware At Hospital Discharge [PDF – 1 page]
- Guide to Using Outpatient Antibiotic Prescription Data for Peer Comparison Audit & Feedback [PDF – 1 page]

Be Antibiotics Aware / Get Ahead of Sepsis
Through the award-winning national educational efforts, Be Antibiotics Aware and Get Ahead of Sepsis, CDC educates the public and healthcare professionals (HCP) about the importance of antibiotic stewardship to ensure appropriate and timely antibiotic use in sepsis management.
Be Antibiotics Aware advertisements to healthcare professionals and patients generated more than 57 million impressions and 364K+ link clicks to the website between April 2021 – May 2022. Webpage views more than doubled on the website from April 2021 (5 million+) to April 2022 (12 million+).
Diagnostic stewardship is defined as ordering the right tests for the right patient at the right time to inform and optimize patient care. CDC published a report that summarizes emerging issues in the field of laboratory diagnostic stewardship emphasizing improving patient treatment, outcomes, and safety. 6
CDC has developed an antibiotic stewardship online training course that offers participants more than 10 hours of free continuing education. It can be accessed in multiple modules and was last updated in 2022.
The Path Forward
The COVID-19 pandemic has presented many challenges and opportunities for improving antibiotic use and sustaining antibiotic stewardship activities and programs. Antibiotic stewardship expertise has been invaluable for supporting the pandemic response, but antibiotic stewardship activities suffered as a result. Health departments, health systems, healthcare facilities, and antibiotic stewards need more resilient antibiotic stewardship programs and activities across all healthcare settings and in all communities. CDC, through the American Rescue Plan, provided more than $120 million in supplemental funding to state and local jurisdictions to expand access to antibiotic stewardship expertise and support antibiotic stewardship interventions in all healthcare settings.
CDC recognizes the importance of reducing and eliminating health inequities to build a healthier nation. Recent expansion of telemedicine may offer opportunities for greater access to care for more Americans. Promoting judicious antibiotic prescribing in this setting is important to ensure patients receive equitable high-quality care. Demographic and socioeconomic factors, such as race and ethnicity, geographic location, insurance status, and patient education, are associated with differences in antibiotic prescribing. Additionally, differences in prescribing practices among healthcare professionals may contribute to inequities. Variability in the quality of antibiotic stewardship programs and activities and access to stewardship expertise may also exacerbate or create health inequities. Healthcare professionals and other partners focused on improving antibiotic use should explore and address potential inequities in the quality of antibiotic prescribing when planning programs, interventions, and activities. CDC is working to characterize disparities in antibiotic prescribing to identify where opportunities exist to improve the quality of care and equity. Additional steps will include identifying research gaps, incorporating equity considerations into policies and practices, and engaging with partners to promote high quality antibiotic prescribing for all.
References
- Tsay SV, Bartoces M, Gouin K, Kabbani S, Hicks LA. Antibiotic Prescriptions Associated With COVID-19 Outpatient Visits Among Medicare Beneficiaries, April 2020 to April 2021. Published online April 08, 2022. doi:10.1001/jama.2022.5471
- Gouin KA, Fleming-Dutra KE, Tsay S, Bizune D, Hicks LA, Kabbani S. Identifying Higher-Volume Antibiotic Outpatient Prescribers Using Publicly Available Medicare Part D Data – United States, 2019. MMWR Morb Mortal Wkly Rep. 2022 Feb 11;71(6):202-205. doi: 10.15585/mmwr.mm7106a3. PMID: 35143465; PMCID: PMC8830623
- King LM, Kusnetsov M, Filippoupolitis A, Arik D, Bartoces M, Roberts RM, Tsay SV, Kabbani S, Bizune D, Rathore AS, Valkova S, Eleftherohorinou H, Hicks LA. Using machine learning to examine drivers of inappropriate outpatient antibiotic prescribing in acute respiratory illnesses. Infect Control Hosp Epidemiol. 2022 Jan 10:1-5. doi: 10.1017/ice.2021.476. Epub ahead of print. PMID: 35001867.
- Bizune D, Tsay S, Kabbani S, Hicks L. (2022). Outpatient antibiotic prescribing during the COVID-19 pandemic-United States, January 2019-October 2021. Antimicrobial Stewardship & Healthcare Epidemiology, 2(S1), S2-3. https://doi.org/10.1017/ash.2022.59
- Kabbani S, Wang S, Ditz L, Gouin K, Palms D, Rowe T, Hyun D, Chi N, Stone N, Hicks L. (2021). Description of antibiotic use variability among US nursing homes using electronic health record data. Antimicrobial Stewardship & Healthcare Epidemiology. 1. 10.1017/ash.2021.207.
- Curren EJ, Lutgring JD, Kabbani S, Diekema DJ, Gitterman S, Lautenbach E, Morgan DJ, Rock C, Salerno RM, McDonald LC. Advancing Diagnostic Stewardship for Healthcare-Associated Infections, Antibiotic Resistance, and Sepsis. Clin Infect Dis. 2022 Mar 1;74(4):723-728. doi: 10.1093/cid/ciab672. PMID: 34346494.