Measuring Outpatient Antibiotic Prescribing
Monitoring of outpatient antibiotic prescribing data is regularly conducted to analyze national and state antibiotic prescribing data in order to better understand trends in outpatient antibiotic prescribing, to identify where interventions to improve prescribing are most needed, and to measure progress. By measuring prescribing and appropriateness, we can compare performance across regions, states, and other entities. National goals are important to help drive change. Quality measures for outpatient antibiotic prescribing can be used by clinicians, healthcare systems, health plans, and public health to determine if antibiotic prescribing patterns meet appropriateness standards. Decision-makers can use these data to guide policy interventions.
Key U.S. Statistics
Below are a number of statistics that help describe how antibiotics are currently being prescribed in outpatient settings in the United States and how these practices are contributing to the larger issue of antimicrobial resistance.
- In 2014, 266.1 million courses of antibiotics are dispensed to outpatients in U.S. community pharmacies. This equates to more than 5 prescriptions written each year for every 6 people in the United States.1
- At least 28% of antibiotics prescribed in the outpatient setting are unnecessary, meaning that no antibiotic was needed at all.2
- Total inappropriate antibiotic use, inclusive of unnecessary use and inappropriate selection, dosing and duration, may approach 50% of all outpatient antibiotic use.3,4,5
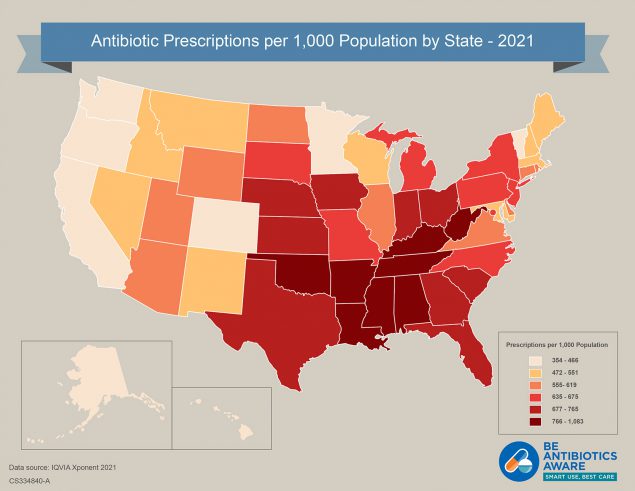
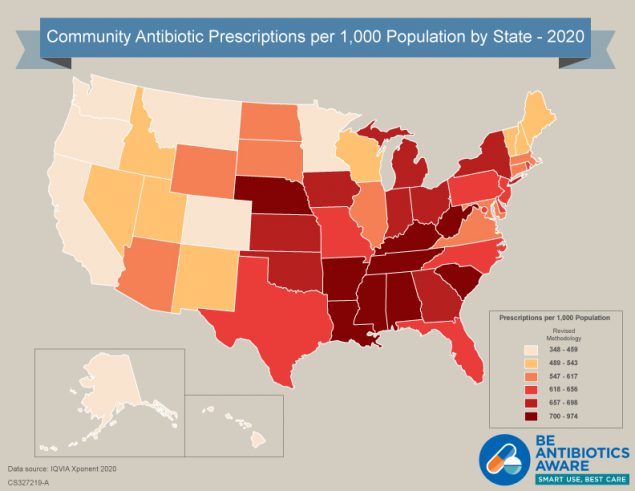
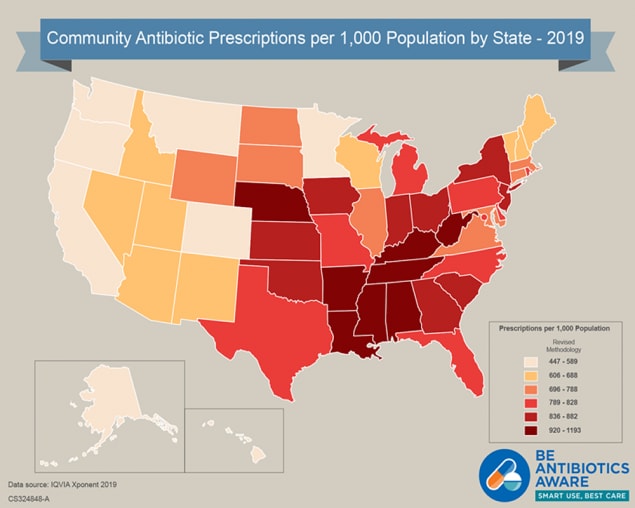
- Antibiotic prescribing in the outpatient setting varies by state.1
- Performance on quality measures for appropriate outpatient antibiotic prescribing varies both by region and health plan.6
- Local outpatient prescribing practices contribute to local resistance patterns.7
- Outpatient antibiotic prescribing is greatest in the winter months.8
- The majority (>60%) of antibiotic expenditures are associated with the outpatient setting.9
- An estimated 80-90% of the volume of human antibiotic use occurs in the outpatient setting.10,11
- Azithromycin and amoxicillin are among the most commonly prescribed antibiotics.1
Data Sources
How can rates and appropriateness of antibiotic prescribing in the U.S. be measured? There are several datasets that can be used:
- CDC’s National Ambulatory Medical Care Survey (NAMCS) and National Hospital Ambulatory Medical Care Survey (NHAMCS) can be used to measure outpatient antibiotic prescribing and appropriateness in U.S. doctor’s offices, emergency departments, and hospital-based clinics.
- Proprietary datasets from third party vendors. For example, IQVIA database can be used to measure the number and rates of outpatient, oral antibiotics dispensed in U.S. community pharmacies.
- Quality measure data, such as Healthcare Effectiveness Data and Information Set (HEDIS), can be used to examine the quality of antibiotic prescribing by region and across health plans.
- Antibiotics are classified into antibiotic classes based on mechanisms of action using IQVIA’s Uniform System of Classification (Print-Only) [PDF – 3 pages].
Outpatient Antibiotic Prescription Report by Year and Interactive Database
View outpatient antibiotic prescription volumes by year, age, sex, region, antibiotic agent, antibiotic class, and provider specialty from IQVIA Xponent® antibiotic prescription data. Yearly antibiotic prescription rates per 1,000 persons by age, sex, and region are calculated using annual U.S. Census files.
Healthcare provider specialties are based on the American Medical Association (AMA) self-designated practice specialties, Drug Enforcement Administration (DEA), and National Provider Identifier (NPI) sources and categorized into one of 17 groups. Provider specialty denominators are estimated by extracting the total number of providers in each provider specialty from the IQVIA Xponent® prescription database. Antibiotic prescription rates by provider specialty are calculated using provider denominators aggregated by IQVIA.
Rates of antibiotic prescriptions by provider specialty in 2011-2021 were calculated using the 2011 provider specialty denominators. Changes in the healthcare workforce numbers were not reflected in the denominators from 2012-2021. In 2022, provider specialty antibiotic prescription rates were calculated using the concurrent 2022 provider specialty denominators.
-
-
- Annual Report 2011
Print only version: Annual Report 2011 [PDF – 684 KB] - Annual Report 2012
Print only version: Annual Report 2012 [PDF – 606 KB] - Annual Report 2013
Print only version: Annual Report 2013 [PDF – 606 KB] - Annual Report 2014
Print only version: Annual Report 2014 [PDF – 338 KB] - Annual Report 2015
Print only version: Annual Report 2015 [PDF – 366 KB] - Annual Report 2016
Print only version: Annual Report 2016 [PDF – 261 KB] - Annual Report 2017
Print only version: Annual Report 2017 [PDF – 4 pages] - Annual Report 2018
Print only version: Annual Report 2018 [PDF – 5 pages] - Annual Report 2019
Print only version: Annual Report 2019 [PDF – 4 Pages] - Annual Report 2020
Print only version: Annual Report 2020 [PDF – 5 Pages] - Annual Report 2021
Print only version: Annual Report 2021 [PDF – 5 Pages] - Annual Report 2022
- Annual Report 2011
-
View outpatient antibiotic prescription data from IQVIA data and U.S. Census files in an interactive database, CDC’s Antibiotic Resistance & Patient Safety Portal.
Appropriateness of Outpatient Antibiotic Prescribing
Appropriate antibiotic prescribing means antibiotics are only prescribed when needed, and when needed, the right antibiotic is selected and prescribed at the right dose and for the right duration. Appropriate antibiotic prescribing should be in accordance with evidence-based national and local clinical practice guidelines, when available.
Inappropriate antibiotic prescribing includes unnecessary prescribing of antibiotics and also when an antibiotic is needed but the wrong antibiotic is prescribed (inappropriate selection) or the wrong dose is given or the antibiotic is prescribed for the wrong length of time. CDC estimates that at least 30% of antibiotics prescribed in the outpatient setting are unnecessary, meaning that no antibiotic was needed at all.2 Total inappropriate antibiotic use, inclusive of unnecessary use and inappropriate selection, dosing and duration, may approach 50% of all outpatient antibiotic use.3,4,5
Quality Measures for Outpatient Antibiotic Prescribing
Healthcare Effectiveness Data and Information Set
HEDIS is a performance measurement tool used by over 90% of the nation’s health plans. HEDIS makes it possible to compare the performance of health plans. CDC and the National Committee on Quality Assurance have written three HEDIS measures related to antibiotic use in outpatient settings.
The pediatric measures, which were incorporated into HEDIS in 2004, are
- Appropriate testing for children with pharyngitis: percentage of children 2 to 18 years of age who were diagnosed with pharyngitis, prescribed an antibiotic and received a group A Streptococcus (strep) test for the episode.
- Nationally, in 2012, mean performance across all health plans was 80% (range 2–97%), compared to a goal of 100%.6
- Appropriate treatment for children with upper respiratory infection (URI): percent of children 3 months to 18 years of age with a diagnosis of URI who were not prescribed antibiotics on or three days after the episode date.
- Nationally, in 2012, mean performance across all health plans was 83% (range 45–99%), compared to a goal of 100%.6
The adult measures, which were incorporated into HEDIS in 2006, are
- Avoidance of antibiotic treatment in adults with acute bronchitis (inverted the measure rate and renamed measure for 2008): percent of adults diagnosed with acute bronchitis who were not dispensed an antibiotic prescription.
- Nationally, in 2012, mean performance across all health plans was 23% (range 7-72), compared to a goal of 100%.
Learn more about HEDIS
National Goals for Improving Outpatient Antibiotic Prescribing
National Action Plan for Combating Antibiotic Resistant Bacteria
The 2020-2025 National Action Plan for Combating Antibiotic-Resistant Bacteria (CARB) targets lowering the annual rate of outpatient dispensing per 1,000 U.S. population, overall and among specified subpopulations. Learn more about how CDC is working to reduce inappropriate antibiotic prescribing.
Healthy People 2020
Healthy People provides science-based, 10-year national objectives for improving the health of all Americans. There are 2 objectives included in the 2020 plan that relate to antibiotic use:
 [JPG - 252 KB]
[JPG - 252 KB]Click to view antibiotic prescribing rates for U.S. health provider offices (2021)
 [JPG - 216 KB]
[JPG - 216 KB]Click to view antibiotic prescribing rates for U.S. health provider offices (2020)
 [PNG - 650 KB]
[PNG - 650 KB]Click to view antibiotic prescribing rates for U.S. health provider offices (2019)
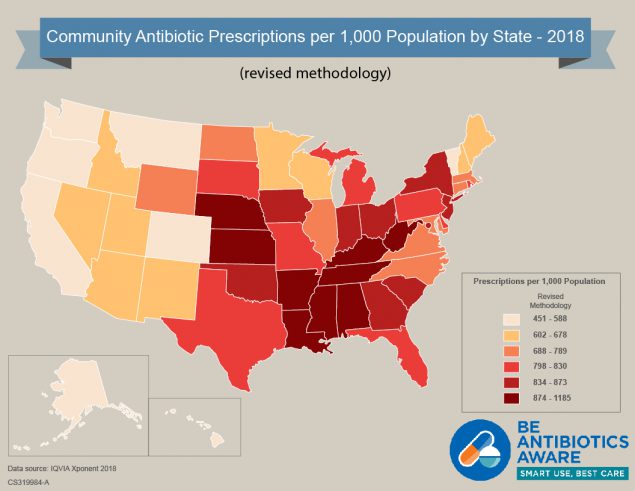 [JPG - 318 KB]
[JPG - 318 KB]Click to view antibiotic prescribing rates for U.S. health provider offices (2018 revised methodology)
 [JPG - 1 MB]
[JPG - 1 MB]Click to view antibiotic prescribing rates for U.S. health provider offices (2017)
 [JPG - 1 MB]
[JPG - 1 MB]Click to view antibiotic prescribing rates for U.S. health provider offices (2016)
 [JPG - 1 MB]
[JPG - 1 MB]Click to view antibiotic prescribing rates for U.S. health provider offices (2015)
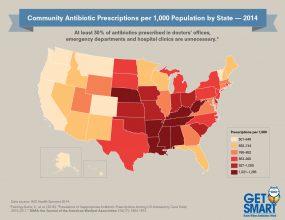 [JPG - 454 KB]
[JPG - 454 KB]Click to view antibiotic prescribing rates for U.S. health provider offices (2014)
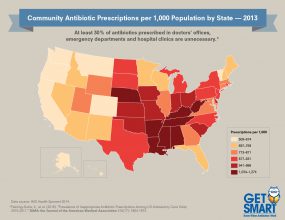 [JPG - 454 KB]
[JPG - 454 KB]Click to view antibiotic prescribing rates for U.S. health provider offices (2013)
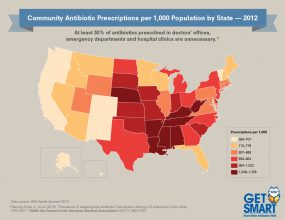 [JPG - 455 KB]
[JPG - 455 KB]Click to view antibiotic prescribing rates for U.S. health provider offices (2012)
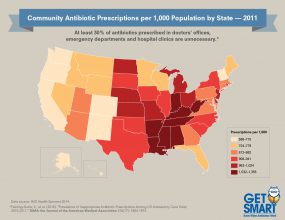 [JPG - 454 KB]
[JPG - 454 KB]Click to view antibiotic prescribing rates for U.S. health provider offices (2011)
Footnotes
- Centers for Disease Control and Prevention. Outpatient antibiotic prescriptions — United States, 2014. Available via the internet: https://www.cdc.gov/antibiotic-use/community/pdfs/annual-reportsummary_2014.pdf [PDF – 336 KB]
- Hersh AL, King LM, Shapiro DJ, Hicks LA, Fleming-Dutra KE. Unnecessary Antibiotic Prescribing in US Ambulatory Care Settings, 2010-2015. Clin Infect Dis. 2021;72(1):133-137.
- Centers for Disease Control and Prevention (CDC). Office-related antibiotic prescribing for persons aged ≤14 years — United States, 1993—1994 to 2007—2008. MMWR Morb Mortal Wkly Rep. 2011;60(34):1153-6.
- Pichichero ME. Dynamics of antibiotic prescribing for children. JAMA. June 19, 2002;287(23):3133-5.
- Shapiro DJ, Hicks LA, Pavia AT, Hersh AL. Antibiotic prescribing for adults in ambulatory care in the USA, 2007–09. J Antimicrob Chemother. 2014;69(1):234-40.
- Roberts, R., et al. (2016). “Variation in US outpatient antibiotic prescribing quality measures according to health plan and geography.” The American journal of managed care 22(8): 519-523.
- Hicks LA, Chien YW, Taylor TH Jr, Haber M, Klugman KP; Active Bacterial Core surveillance (ABCs) Team. Outpatient antibiotic prescribing and nonsusceptible Streptococcus pneumoniae in the United States, 1996-2003. Clin Infect Dis. 2011;53(7):631-9.
- Suda KJ, Hicks LA, Roberts RM, Hunkler RJ, Taylor TH. Trends and seasonal variation in outpatient antibiotic prescription rates in the United States, 2006 to 2010. Antimicrob Agents Chemother. 2014;58(5):2763-6.
- Suda KJ, Hicks LA, Roberts RM, Hunkler RJ, Danziger LH. A national evaluation of antibiotic expenditures by healthcare setting in the United States, 2009. J Antimicrob Chemother. 2013;68:715-8
- Public Health England. English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR): report 2014 [Internet]. London, England: Public Health England; 2014. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/362374/ESPAUR_Report_2014__3_.pdf [PDF – 4.35 MB]
- Public Health Agency of Sweden, National Veterinary Institute. Consumption of antibiotics and occurrence of antibiotic resistance in Sweden [Internet]. Swedres-Svarm 2014. Solna and Uppsala, Sweden: Public Health Agency of Sweden, National Veterinary Institute; 2015. Report No.: ISSN 1650–6332. https://www.folkhalsomyndigheten.se/pagefiles/20281/Swedres-Svarm-2014-14027.pdf [PDF -4.9 MB]