Antibiotic Use in the United States, 2021 Update: Progress and Opportunities
Introduction
Antibiotic stewardship, or improving how antibiotics are prescribed and used, remains critical to optimize the treatment of patients who have infections, protect patients from harm, and combat antibiotic resistance. In 2020, The Centers for Disease Control and Prevention (CDC) released “Antibiotic Use in the United States, 2020 Update: Progress and Opportunities [PDF – 26 Pages],” which highlighted how antibiotics are being used in the United States through data, new resources, and examples of stewardship activities across all healthcare settings with a look at new challenges presented by the COVID-19 pandemic.
Some of the data, resources, and antibiotic stewardship examples included in this update capture the impact of the Coronavirus 2019 (COVID-19) pandemic on U.S. antibiotic use and stewardship activities. During the last year, CDC assessed changes in how antibiotics were used across healthcare settings and learned how states and antibiotic stewards were able to work through the challenges brought about by the COVID-19 pandemic to continue to focus on antibiotic stewardship activities.
In addition, CDC continues to work with partners to integrate antibiotic stewardship principles with other critical components of healthcare, including sepsis management, diagnostic stewardship, and telemedicine. CDC remains committed to addressing antibiotic prescribing health disparities and promoting health equity in all communities and across all healthcare settings.
This report also contains:
- Progress on the goals contained in the U.S. National Action Plan for Combating Antibiotic-Resistant Bacteria (CARB), first published in 2015 and updated in 2020
- Data describing U.S. outpatient antibiotic prescribing rates and implementation of hospital antibiotic stewardship programs by state, including examples of stewardship accomplishments during the COVID-19 pandemic
- Summaries of recently published literature highlighting progress and opportunities for stewardship across all healthcare settings
- New and updated resources for health departments, facilities, healthcare professionals, and payers to implement antibiotic stewardship
- Data on antibiotic use and examples of stewardship during the COVID-19 pandemic
- Emerging opportunities for antibiotic stewardship
Progress on the U.S. National Action Plan for Combating Antibiotic-Resistant Bacteria (CARB)
The U.S. National Action Plan for Combatting Antibiotic-Resistant Bacteria directs federal agencies to accelerate the U.S. government’s response to antibiotic resistance by presenting coordinated, strategic actions to improve the health and well-being of all Americans across the One Health spectrum. The National Action Plan was first released in 2015 and includes national targets to combat antibiotic-resistant bacteria, specifically those recognized in CDC’s 2019 Antibiotic Resistance Threats Report. In late 2020, CDC joined with other federal partners in the CARB Task Force to release the next iteration of the National Action Plan, outlining ambitious goals and actions to be completed from 2020 through 2025 National Action Plan for Combating Antibiotic-Resistant Bacteria, 2020-2025 | ASPE (hhs.gov).
An antibiotic stewardship goal from the first CARB National Action Plan (2015 – 2020) was to reduce inappropriate outpatient antibiotic use by 50% by 2020. To achieve this goal, CDC led various activities:
- Worked with partners to expand the use of data by states and payers to engage high prescribers
- Conducted outreach to partners and promotion of the appropriate use of diagnostic tools to inform antibiotic use
- Provided improved access to tools and resources for outpatient providers, including resources focused on prescribing during the transition between inpatient care and outpatient care
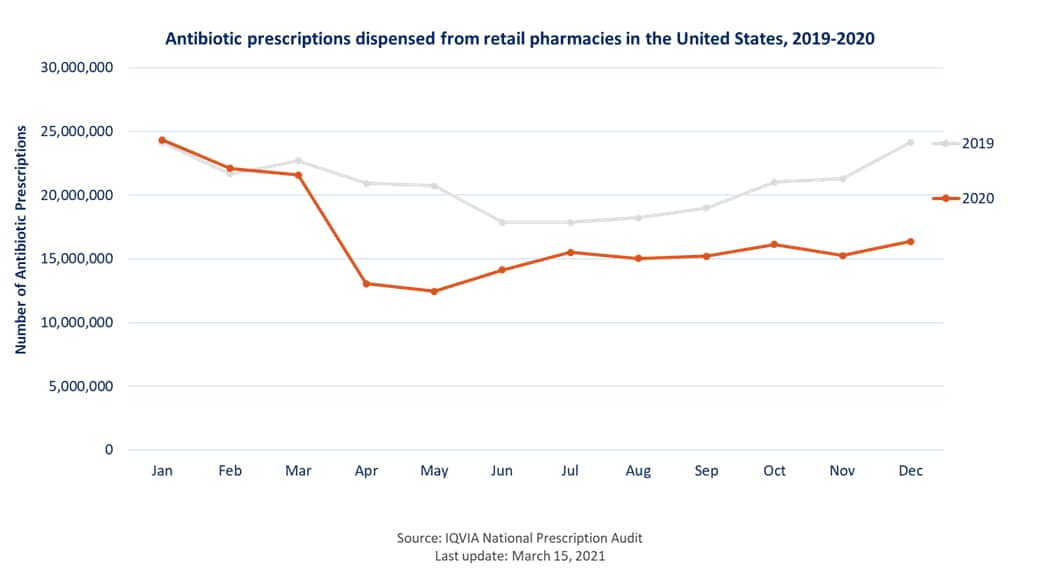
From 2011 to 2018, outpatient antibiotic prescriptions decreased overall by 10%, on track to meet the 2020 CARB goal. However, the COVID-19 pandemic had a significant impact on outpatient antibiotic prescribing – from 2019 to 2020 there was a 25% decrease in outpatient prescriptions resulting in prescribing rates that were much lower, exceeding the reduction of 15% in overall antibiotic prescribing needed to reach the 2020 CARB goal. This was likely due, in part, to decreases in outpatient visits and healthcare seeking due to the pandemic. CDC will continue to analyze prescribing data to identify the ongoing impact of the pandemic on prescribing. Healthcare providers, states, antibiotic stewards and other partners have all had an impact in moving us in the right direction to meet this goal.
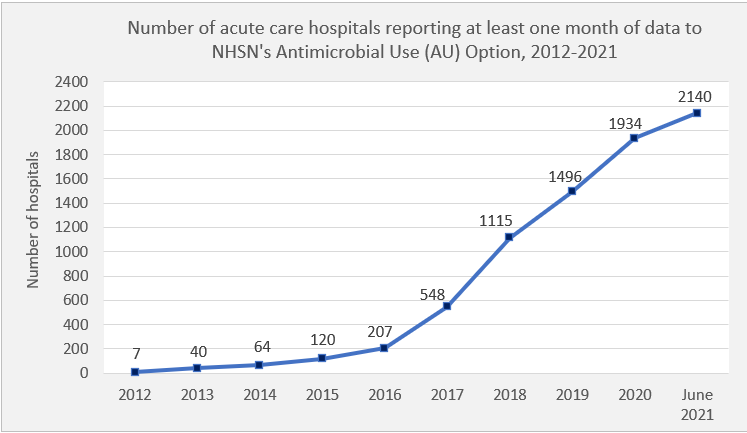
CDC also made great progress toward a second stewardship-related CARB goal of establishing antibiotic stewardship programs in all acute care hospitals with the percentage of hospitals that implemented stewardship programs increasing from 48% in 2015 to 91% in 2020.
CDC continues to pursue ambitious goals in the new CARB plan, which builds on the 2015 National Action Plan by expanding evidence-based activities that have already been shown to slow resistance.
Goals and objectives in the new report relevant to stewardship include:
- Engage the public and other partners to develop, expand, and increase national and state education, training, and communication efforts focused on using antibiotics responsibly, stopping the spread of antibiotic resistance, and preventing infections and life-threatening conditions like sepsis. This includes expanding the scope and reach of CDC’s educational efforts, including Be Antibiotics Aware and Get Ahead of Sepsis.
- Develop and implement policies and practices to promote the responsible use of antibiotics. This includes improving national outpatient antibiotic use, including lowering the annual rate of outpatient antibiotic dispensing per 1,000 US population as well as lowering the annual proportion and rate of antibiotic prescriptions for outpatient visits where antibiotics are not needed, according to evidence based guidelines. This goal also includes supporting national and state policies that improve antibiotic use across all healthcare settings and supporting research to improve responsible use of antibiotics.
- Expand the number of sources for and quantity of surveillance data on the use of antibiotics from inpatient and outpatient healthcare facilities to improve understanding and implementation of the optimal use of antibiotics. This includes the target of having 100 percent of acute care and 50 percent of critical access hospitals reporting to the CDC National Healthcare Safety Network (NHSN) Antimicrobial Use option.
The Antibiotic Resistance and Patient Safety Portal is a resource to explore and visualize data on outpatient antibiotic prescribing, hospital antibiotic stewardship implementation, antibiotic resistance, and healthcare-associated infections.
Explore here: https://arpsp.cdc.gov/
CDC works to improve antibiotic use by collecting, analyzing, and publishing data to support antibiotic stewardship efforts in state, tribal, local, or territorial health departments, in healthcare facilities across the spectrum of human healthcare, and by individual prescribers.
Community Antibiotic Prescriptions by State – 2019 (Map)
Outpatient antibiotic prescribing is improving, but prescribing rates still vary widely across the United States. This map suggests that there are stewardship opportunities for providers, facilities, and other partners interested in improving how antibiotics are used. This map displays prescription rates of all antibiotic classes per 1,000 population dispensed in outpatient pharmacies across U.S. states in 2019.
This project was made possible through a partnership with the CDC Foundation. Support for this project was provided by The Pew Charitable Trusts.
Percentage of Hospitals Meeting All 7 Core Elements, by State – 2020 (Map)
CDC’s Core Elements of Hospital Antibiotic Stewardship provides a framework for implementation of antibiotic stewardship programs. Partners across the country are using the Core Elements to guide antibiotic stewardship efforts in hospital settings. The Core Elements form the foundation for antibiotic stewardship accreditation standards from the Joint Commission and DNV-GL. The 2019 hospital Conditions of Participation from the Centers for Medicare and Medicaid Services (CMS) created a federal regulation for hospital antibiotic stewardship programs and reference the Core Elements. This map shows the percentage of hospitals meeting all 7 Core Elements, by state, in 2020.
National Healthcare Safety Network Antimicrobial Use Option (Figure and Map)
The NHSN AUR Module [PDF – 57 pages] provides a voluntary mechanism for facilities to monitor antibiotic use and resistance data to help reduce antibiotic-resistant infections through antibiotic stewardship and interrupt transmission of resistant pathogens. One output measure included in NHSN’s Antimicrobial Use (AU) Option of the AUR Module is the Standardized Antimicrobial Administration Ratio (SAAR). The SAAR is a risk-adjusted benchmarking measure of antibiotic use and can help inform stewardship efforts by enabling hospitals to see how their SAARs compare to other facilities. More than 2,100 acute care hospitals across the United States have submitted at least one month of data to the AU Option as of June 2021. Of those hospitals, 1,946 reported in the past 12 months.
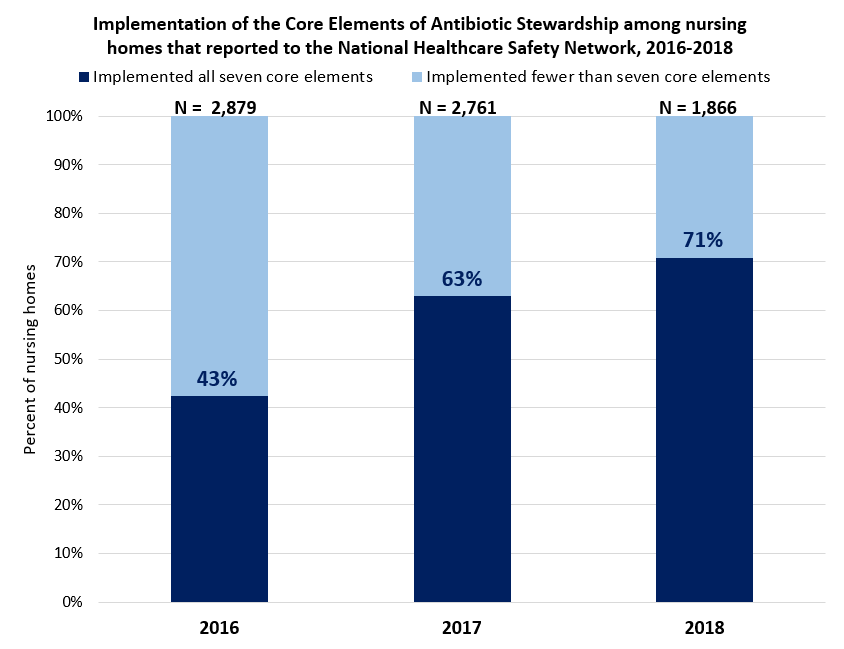
Implementation of Core Elements in Nursing Homes 2016-2018
CDC’s Core Elements of Antibiotic Stewardship for Nursing Homes adapted the hospital framework for implementation of antibiotic stewardship programs to the unique needs and challenges of nursing homes. CMS released a federal rule requiring nursing homes to implement an antibiotic stewardship program that also references the Core Elements in 2016. In 2018, nearly three quarters of nursing homes reporting to CDC’s National Healthcare Safety Network implemented all 7 Core Elements of antibiotic stewardship. From 2016 to 2018, a 28% increase in reported implementation of Core Elements was observed in nursing homes.
Highlights of Progress and Opportunities for Stewardship Across All Healthcare Settings
These studies are examples of how data can be used to inform action at the community, facility, or individual healthcare provider level across healthcare settings.
Antimicrobial Use in U.S. Hospitals: Comparison of Results from Emerging Infections Program Prevalence Surveys, 2015 and 2011
Magill SS, O’Leary E, Ray SM, et al. Clin Infect Dis. 2021 May 18;72(10):1784-1792.
In the 2011 U.S. hospital prevalence survey of healthcare-associated infections and antimicrobial use 50% of patients received antimicrobial medications on the survey date or day before. A repeat of the survey was conducted in 2015 to determine antimicrobial use prevalence and describe changes since 2011. Overall hospital antimicrobial use prevalence was not different in 2011 and 2015; however, differences observed in selected patient or antimicrobial groups may provide evidence of stewardship impact.
Health Experts Establish Targets to Improve Hospital Antibiotic Prescribing
National Data shows inappropriate prescribing, opportunities for improvement
The Pew Charitable Trusts partnered with the CDC and other public health and medical experts to evaluate antibiotic use in hospitals and set national targets to improve prescribing. Using national prescribing data from the prevalence survey conducted by Magill and colleagues published in JAMA Network Open in 2021, the experts examined the use of two types of antibiotics—vancomycin and fluoroquinolones—and antibiotic treatments associated with two conditions: community-acquired pneumonia (CAP) and urinary tract infections (UTIs). The panel recommended a national target to reduce inappropriate use for each of the antibiotics by 95% and for each of the conditions by 90%. Read the CDC Safe Healthcare Blog to learn more.
Assessment of the Appropriateness of Antimicrobial Use in U.S. Hospitals
Magill SS, O’Leary E, Ray SM, et al. JAMA Netw Open. 2021 Mar 1;4(3):e212007.
A point prevalence survey was conducted in 2015 and establishes a baseline assessment of antibiotic prescribing quality for four common prescribing scenarios in hospitals. More than half of antibiotic prescribing for selected events in hospitals was not consistent with recommended prescribing practices. Antibiotics were often prescribed for too long, when there was no clinical indication, or the antibiotic selected didn’t follow treatment guidelines.
Antimicrobial Use in a Cohort of U.S. Nursing Homes, 2017
Thompson ND, Stone ND, Brown CJ, et al. JAMA. 2021 Apr 6;325(13):1286-1295.
A point prevalence survey was conducted in 2017 to collect data on characteristics of residents and antimicrobials administered in 161 nursing homes. Antimicrobial use prevalence was 8.2 per 100 residents who received at least 1 antimicrobial on a given day. Antibiotics were most commonly used to treat urinary tract infections.
Urinary Tract Infection Treatment Practices in Nursing Homes Reporting to the National Healthcare Safety Network, 2017
Kabbani S, Palms D, Bell JM, et al. Infect Control Hosp Epidemiol. 2021 Mar 12;1-3.
Epidemiology of Antibiotic Use for Urinary Tract Infection in Nursing Home Residents
Thompson ND, Penna A, Eure TR, et al. J Am Med Dir Assoc. 2020 Jan;21(1):91-96.
Two analyses highlighted antibiotic use for urinary tract infections in nursing homes. One analysis described differences between urinary tract infection treatment and events reported by nursing homes enrolled in the National Healthcare Safety Network. In 2017, almost 4 times as many antibiotics starts as an infection events were reported. The second analysis reported that nursing home-specific prevalence rates for urinary tract infections varied by more than 10-fold. Urinary tract infection prophylaxis was common with a long-planned duration, despite limited evidence to support this practice among older persons in nursing homes. Both analyses suggest that opportunities exist for antibiotic stewardship and improvement of diagnosis and treatment of urinary tract infections in nursing homes.
Data on Antibiotic Use and Examples of Stewardship During the COVID-19 Pandemic
The COVID-19 pandemic has presented both challenges and opportunities for healthcare providers, public health professionals, health systems, and other partners to continue stewardship activities. The following examples help us better understand how antibiotic use and stewardship were impacted by the pandemic, and how healthcare providers, health systems, and state health departments were able to continue their focus on antibiotic stewardship activities, despite the many additional challenges faced during the COVID-19 pandemic.
The Pew Charitable Trusts: Could Efforts to Fight the Coronavirus Lead to Overuse of Antibiotics?
A Pew study found more than half of hospitalized COVID-19 patients in the U.S. received antibiotics in the pandemic’s first six months.
Trends in U.S. Outpatient Antibiotic Prescriptions During the Coronavirus Disease 2019 Pandemic
King LM, Lovegrove MC, Shehab N et al, Clin Infect Dis. 2020 Dec 29
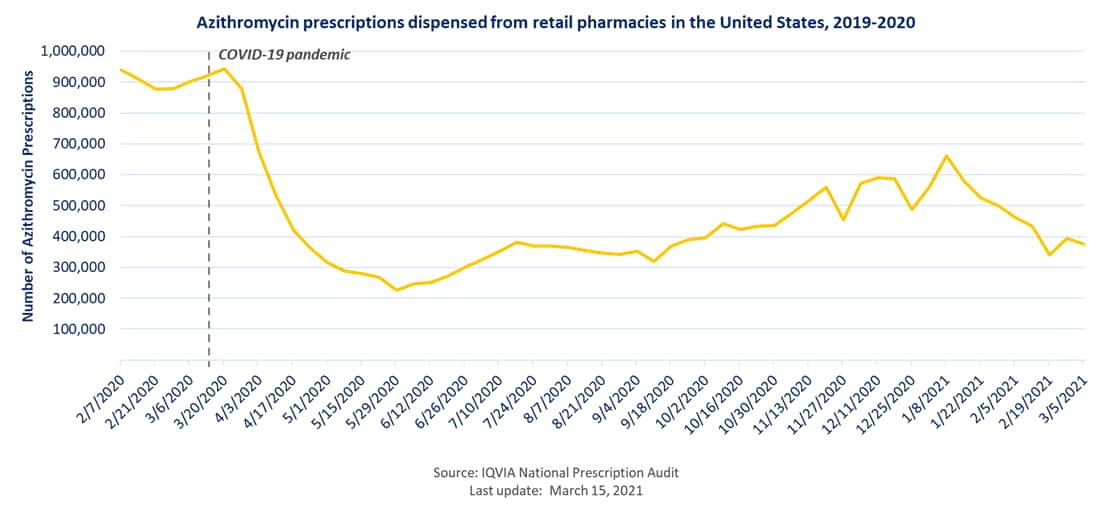
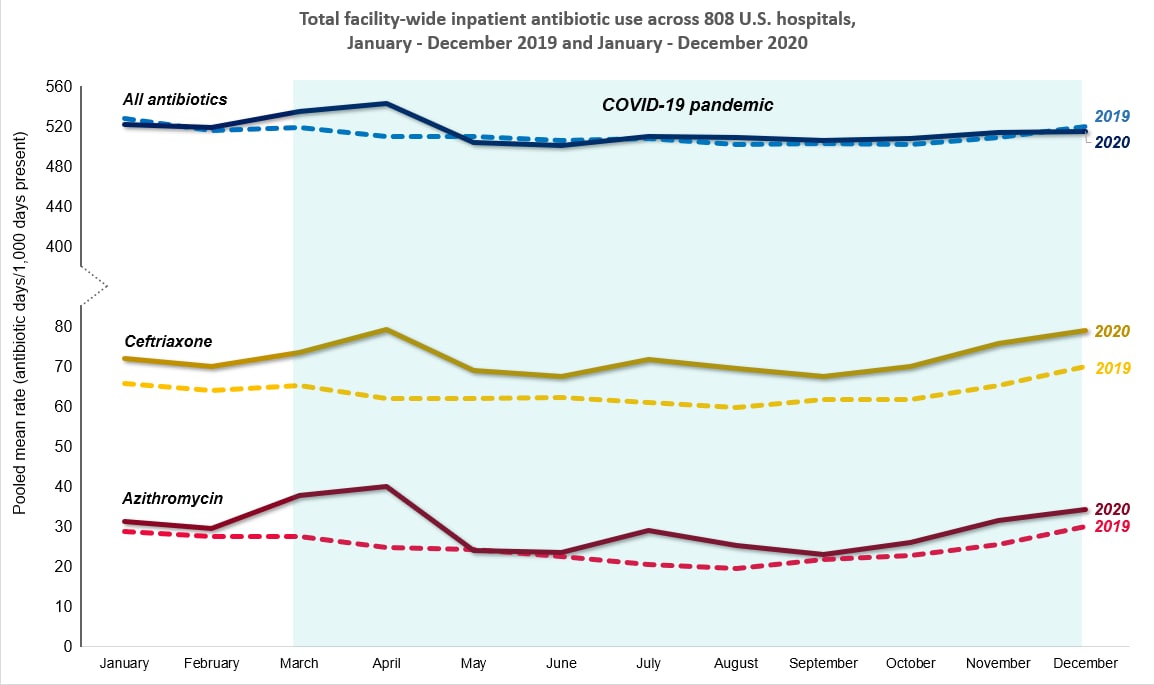
From January to May of 2020, antibiotic prescribing decreased substantially in outpatient settings, potentially due to a decrease in the spread of non-COVID-19 respiratory diseases (e.g. common cold, flu) and changes in outpatient healthcare access. However, azithromycin prescribing rates differed from other antibiotics; prescribing for this antibiotic was higher than expected early in the COVID-19 pandemic.
Antibiotic Use in U.S. Hospitals During the COVID-19 Pandemic
Rose AN, Baggs J, Wolford H, et al. Trends in Antibiotic Use in U.S. Hospitals during the COVID-19 Pandemic. Open Forum Infect Dis. 2021 Jun 3; 8(6): 1-5.
This study showed that almost 80% of patients hospitalized with COVID-19 received antibiotic therapy, frequently agents used to treat lower respiratory tract infections. Approximately half of hospitalized patients received ceftriaxone, which was commonly prescribed with azithromycin.
Acute Care Antibiotic Use During the COVID-19 Pandemic
The following figure uses NHSN AU Option data to show total facility-wide inpatient antibiotic use across more than 800 hospitals in the United States from January 2019-January 2020..
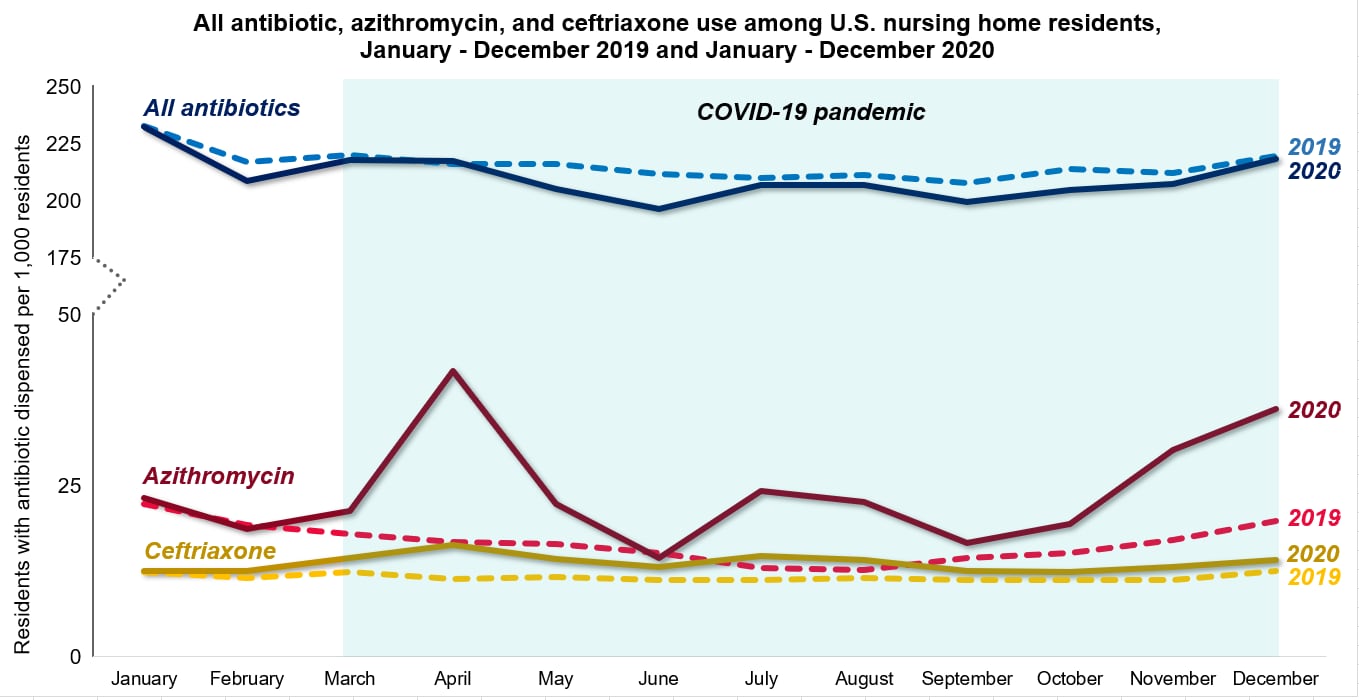
Trends in Prescribing of Antibiotics and Drugs Investigated for COVID-19 Treatment in U.S. Nursing Home Residents During the COVID-19 Pandemic
Gouin KG, Creasy S, Beckerson M et al, Clin Infect Dis. 2021 Mar 10
From January to December, overall antibiotic prescribing in nursing homes was 3% lower in 2020 than in 2019, which may be attributed to several factors, including changes in healthcare delivery among nursing home residents, changes in the resident population during the pandemic and increased awareness and improved implementation of infection prevention and control measures. However, increased prescribing of antibiotic agents that are commonly used for respiratory infections was observed. Specifically, azithromycin prescribing was 46% higher compared to 2019 and ceftriaxone prescribing was 18% higher compared to 2019..
Intermountain Healthcare Intervention To Improve Urgent Care Prescribing
Prior to the start of the pandemic, partners at Intermountain Healthcare had already planned work to improve respiratory antibiotic prescribing in a large network of urgent care clinics by implementing a comprehensive, multifaceted stewardship program based on the CDC Core Elements of Outpatient Stewardship. The intervention ran from July 2019 through June 2020 (compared with a baseline period of July 2018–June 2019) and included five categories of activities: (1) education, (2) electronic health record (EHR) tools, (3) provider benchmarking dashboard, (4) media, and (5) organizational alignment. The researchers found a similar number of encounters in the baseline and intervention periods for respiratory diagnoses (baseline: 235,061 or 41% of all visits vs. intervention: 202,064 or 39% of all visits). The respiratory encounter prescribing rate decreased from an average of 49% during the baseline period to an average of 34% during the intervention period. First-line therapy use for sinusitis, otitis media (OM), and pharyngitis improved from 70% to 74% in the intervention period. Antibiotic prescribing for respiratory conditions that do not require antibiotic treatment decreased from 20% in the baseline period to 8% during the intervention period. Likewise, azithromycin prescribing decreased from 9.7% to 3.3% during the intervention period.
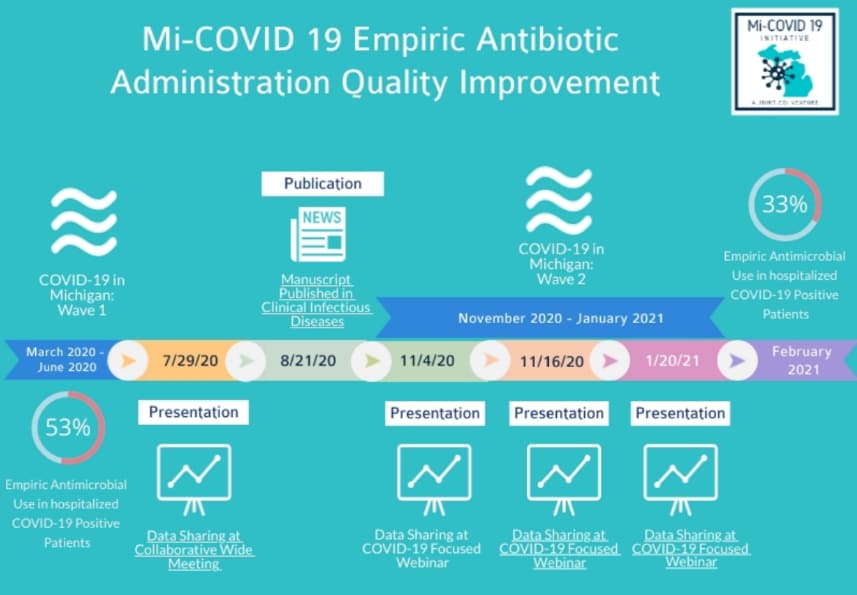
Michigan COVID-19 Initiative (Mi-COVID19) Joint Collaboration
In response to the COVID-19 pandemic, a joint CQI (Collaborative Quality Initiative) venture, Mi-COVID 19, rapidly formed under the leadership of the Michigan Hospital Medicine Safety Consortium (HMS), a collaborative of hospitals working towards optimizing antimicrobial use since 2017. Several different Blue Cross Blue Shield of Michigan (BCBSM) CQIs joined together and built the Mi-COVID19 Registry three weeks after the first case of COVID-19 in Michigan. From April 2020 through January 2021, over 40 hospitals across Michigan helped collect and share data on thousands of patients hospitalized with COVID-19. Data collected from the first surge of patients with COVID-19 showed high rates of early empiric antibiotic use (within 2 days of hospitalization) despite low rates of community-onset bacterial co-infection.
In response to these data, a multi-pronged improvement strategy was implemented that included early data sharing of hospital prescribing practices and variability, focused educational webinars, and identification and sharing of risk factors for bacterial co-infection. Between the first COVID-19 wave (March 2020–June 2020) and second wave (November 2020–January 2021), collaborators observed a decrease from 53% to 33% (p <.0001) in early empiric antibiotic use among non-critically ill patients hospitalized with COVID-19 (n=2,368). The Mi-COVID-19 collaboration demonstrated how an existing CQI infrastructure can be rapidly leveraged as a larger team to focus antibiotic stewardship efforts on improving antibiotic use during the COVID-19 pandemic.
Be Antibiotics Aware and Get Ahead of Sepsis

CDC educates the public and healthcare professionals (HCP) about improving antibiotic use through the award-winning national educational effort, Be Antibiotics Aware. Together with the Get Ahead of Sepsis educational effort, CDC is promoting the importance of antibiotic stewardship to ensure appropriate and timely antibiotic use in sepsis management. Antibiotics can save lives and are critical tools for treating infections, including those that can lead to sepsis. However, any time antibiotics are used, they can cause side effects or adverse events, such as Clostridioides difficile (or C. diff) infection and contribute to the development of antibiotic resistance.
In spring and summer 2021, Be Antibiotics Aware and Get Ahead of Sepsis launched a two-phased paid media campaign to raise awareness about antibiotic use and sepsis among consumer and healthcare professional audiences, increase engagement with CDC antibiotic use and sepsis information, and increase downloads of educational materials on these topics from CDC’s website. Both educational efforts used a variety of channels (e.g., Facebook, LinkedIn) to disseminate information about appropriate antibiotic use and sepsis to healthcare professionals and consumers, including updating current messages for consistency with COVID-19-specific messaging.
Core Elements of Antibiotic Stewardship
CDC’s Core Elements of Antibiotic Stewardship offers healthcare professionals and antibiotic stewardship leaders a set of key principles to guide efforts to improve antibiotic use, in order to protect patients and improve outcomes. This framework complements existing guidelines and standards from key healthcare partner organizations. The following Core Element documents are available for healthcare professionals and facility use in implementing antibiotic stewardship activities:
- Core Elements of Hospital Antibiotic Stewardship Programs
- Implementation of Antibiotic Stewardship Core Elements at Small and Critical Access Hospitals
- Core Elements of Outpatient Antibiotic Stewardship
- Core Elements of Antibiotic Stewardship for Nursing Homes
- Core Elements of Human Antibiotic Stewardship Programs in Resource-Limited Settings
CDC Training on Antibiotic Stewardship
CDC has an antibiotic stewardship online training course that offers participants more than 10 hours of free continuing education. It can be accessed in multiple modules. Course objectives include informing healthcare professionals about proper antibiotic prescribing in all healthcare settings and the threat of antibiotic-resistant organisms, as well as encouraging open discussion among healthcare professionals and patients. Content includes new information on serious and urgent antibiotic resistance threats, guidelines and resources for dental prescribing, and the Core Elements of Antibiotic Stewardship Programs across various healthcare settings.
Nursing Home Stewardship Intervention
Baier RR, Jump RLP, Zhang T, et al. Feasibility of a Nursing Home Antibiotic Stewardship Intervention. J Am Med Dir Assoc. 2021 Sep 7;S1525-8610(21)00746-5.
CDC contracted Brown University School of Public Health to develop and test an intervention to help nursing staff implement antibiotic stewardship practices in nursing homes. The researchers developed a bundle of three electronic tools to improve antibiotic use that was piloted in five nursing homes and then implemented, with revisions and additions, in another eight nursing homes. The three tools were: (1) a change in condition tool; (2) electronic health record antibiotic follow-up based on existing algorithms [PDF – 1 Page] and (3) an infection tracking log. Along with training, the bundled intervention standardized documentation of clinical and prescribing data to track a change in resident condition, infections, antibiotic prescribing, and antibiotic follow-up.
The 2020 NHSN AU Option Report provides a summary of SAAR distributions and percentages of use within the SAAR antimicrobial agent categories in adult, pediatric and neonatal patient care locations. The SAAR distributions can help inform stewardship efforts by enabling hospitals to see how their SAARs compare to the national distribution.
State, Federal, and Academic Partners
Colorado Department of Public Health & Environment (CDPHE): During the pandemic, most of the CDPHE Healthcare-Associated Infection and Antibiotic Resistance program staff were deployed to support the COVID-19 pandemic. CDPHE responded by integrating antibiotic stewardship work into other program activities, involving more staff in the work, and choosing activities that were efficient and likely to have impact. CDPHE chose to focus on an audit and feedback intervention, because it was evidence-based, coordinated by CDC, and involved leveraging antibiotic use data from IQVIA. During U.S. Antibiotic Awareness Week 2020, CDPHE sent approximately 1,500 peer-comparison letters to the state’s top 10% of prescribers of antibiotics by volume. A few recipients completed a feedback form and indicated that they recognized that appropriate antibiotic prescribing was an important public health issue and that they planned to access the resources and change their prescribing practices.
CDPHE also had the opportunity in 2020 to work with Dr. Danny Dodson, who is a Leadership in Epidemiology, Antibiotic Stewardship, and Public Health (LEAP) Fellow and Infectious Diseases fellow at Children’s Hospital Colorado. Dr. Dodson systematically evaluated antibiotic stewardship programs in Colorado hospitals through a survey and interviews. The objectives of his work were to evaluate 1) the scope and quality of antibiotic stewardship programs, 2) interventions for pediatric patients, and 3) the impact of the COVID-19 pandemic on antibiotic stewardship. Dr. Dodson was able to identify some needs of hospitals that public health and academic partners may begin to address as well as maintain a public health presence for antibiotic stewardship during the pandemic.
Diagnostic stewardship means ordering the right tests for the right patient at the right time to optimize antibiotic use and improve patient outcomes, including reductions in antibiotic-resistant infections, and treatment of sepsis. Guidelines developed for the treatment and management of infections should include criteria for the appropriate use of laboratory tests. CDC’s Division of Healthcare Quality Promotion (DHQP) hosted a meeting on improving patient safety through diagnostic stewardship with a focus on the use of the laboratory. A white paper that summarizes the needs and future avenues for diagnostic stewardship implementation, including areas of needed research, was published in August 2021.
Improving Outpatient Antibiotic Prescribing: A Toolkit for Healthcare Payers [PDF – 30 Pages]
Recognizing that healthcare payers are leaders in healthcare quality improvement and have a unique role to play in improving outpatient antibiotic use, this new toolkit provides a framework for payers to get started with outpatient antibiotic stewardship work and materials and examples specific to this audience.
Quality Measure: Antibiotic Utilization for Acute Respiratory Infection
The National Committee for Quality Assurance (NCQA), who maintains the Healthcare Effectiveness Data and Information Set® (HEDIS) measures, has developed a new measure: Antibiotic Utilization for Respiratory Conditions (AXR). This measure assesses antibiotic prescribing across respiratory conditions, which drive a large portion of antibiotic use. The measure will provide context for antibiotic use across a health plan’s membership and better characterize opportunities for improvement in this area. AXR will be included in HEDIS Measurement Year 2022.
Antibiotic Stewardship in Action
- The Florida Department of Health (FDOH) analyzed IQVIA Xponent data to describe the overall top 10% of antibiotic prescribers in the state, grouped by specialty type, for the year of 2018. These data were used to target interventions to specific specialty groups and led to CDC Field Medical Officer with FDOH’s Healthcare-Associated Infection Prevention Program, Dr. Christopher Prestel, providing a statewide webinar on antibiotic stewardship. Topics covered during the webinar included highlights of recent studies examining antibiotic stewardship principles and outcomes, practices to improve antibiotic stewardship across the spectrum of health care and action steps healthcare facilities and providers can take to improve their antibiotic prescribing practices.
- OASIS© (Outpatient Automated Stewardship Information System)leverages statistical software that accesses the electronic health record data warehouse to automate extraction, computation, and formatting to create and email individualized provider antibiotic prescribing reports with peer comparison directly to clinicians. OASIS© programs can be freely shared between healthcare organizations to facilitate stewardship collaboration. Dr. Holly M. Frost and colleagues at Denver Health and the University of Colorado developed OASIS© to reduce the financial and time resources needed for tracking and reporting. (Frost HM, Munsiff SS, Lou Y, Jenkins TC. Simplifying Outpatient Stewardship. Infect Control Hosp Epidemiol. 2021 Feb 1;1-2. doi: 10.1017/ice.2020.1409. Online ahead of print.)
- The Agency for Healthcare Research and Quality (AHRQ), in partnership with Johns Hopkins Medicine and NORC at The University of Chicago, created the AHRQ Safety Program for Improving Antibiotic Use to develop and implement a bundle of interventions designed to improve antibiotic stewardship and antibiotic prescribing practices in acute care, long-term care, and ambulatory care facilities across the United States. The Antibiotic Stewardship Toolkit for Hospitals, publicly available on AHRQ’s website, guides users through the signature “Four Moments of Antibiotic Decision Making,” providing a step-by-step approach for physicians to optimize antibiotic prescribing. The toolkit offers more than 50 tools, including best practices for diagnosis and treatment of infections, approaches to improve safety culture and sustain overall success, plus tactical recommendations to demonstrate the value of antibiotic stewardship programs to hospital administrators and prescribers.
Do you have an antibiotic stewardship success story that others could learn from? Submit success stories by emailing antibioticuse@cdc.gov.
Emerging Opportunities for Antibiotic Stewardship
The COVID-19 pandemic has presented many challenges and opportunities for improving antibiotic use and sustaining antibiotic stewardship activities and programs. Many antibiotic stewardship programs were unable to sustain key activities during the pandemic due to staffing cuts and need to pivot to pandemic-related activities. It has become more evident than ever that there is a need for health departments, health systems, healthcare facilities, and antibiotic stewards to identify how to support resilience of antibiotic stewardship programs across all healthcare settings and in all communities. There is also a need for expansion and better understanding and utilization of diagnostic stewardship; for healthcare providers to have the access and ability to use rapid, accurate testing to assist in the diagnosis and treatment of many conditions for which antibiotics are so often inappropriately prescribed. The pandemic also highlighted the need to address two very important topic areas that are relevant to antibiotic stewardship: health equity and telehealth.
Health Equity and Antibiotic Use
Reducing and eliminating health disparities are critical to building a healthier nation and achieving health equity. Health equity is the attainment of the highest level of health for all people. Population-level factors, such as the physical, built, social, and policy environments, can have a greater impact on health outcomes than individual-level factors. The root causes of health inequity can be directly linked to a failure to address these population-level factors. In addition, linkages between science, policy, and practice are critical to achieving health equity. Health disparities are health differences closely linked with social, economic, and/or environmental disadvantage or other characteristics historically linked to discrimination or exclusion. There are opportunities within the field of antibiotic stewardship to assess and address health disparities related to antibiotic prescribing to pursue health equity. For example, children who receive care from a pediatrician compared to other healthcare professionals (e.g. family practice provider, nurse practitioner) are more likely to receive appropriate antibiotic therapy. The quality of antibiotic stewardship programs and activities in locations that may have fewer resources to allocate to stewardship also vary in ways that could exacerbate or create health disparities. Healthcare providers and other partners focused on improving antibiotic use should explore whether disparities exist in the quality of antibiotic prescribing when planning programs, interventions, and activities. CDC is working to more fully characterize disparities in antibiotic prescribing to identify where opportunities exist to improve the quality of care and equity. CDC is also working with partners to prioritize work in this area, including serving as a member of the Presidential Advisory Council on Combating Antibiotic-Resistant Bacteria (PACCARB) subcommittee on Antibiotic Access and Use.
Telehealth and Antibiotic Stewardship
Over the course of the COVID-19 pandemic, telehealth services have been leveraged to facilitate ongoing patient care during a time when healthcare professionals had to decrease or cease in-person visits. Many health systems and clinical practices have integrated telehealth into their healthcare delivery model. In addition, direct-to-consumer telehealth companies offer access to healthcare by phone or through virtual platforms. There are potential implications for antibiotic stewardship. First, antibiotic prescribing practices are not well-defined in telehealth. Second, few studies have assessed the impact of antibiotic stewardship interventions for telehealth. Lastly, antibiotic stewardship guidance specific to telehealth doesn’t currently exist. CDC is analyzing existing data sources and working with partners to better characterize prescribing in telehealth, identify best practices, and develop guidance to optimize antibiotic prescribing in this growing healthcare delivery model.
Additional information on the expansion of telehealth as a healthcare delivery model: