Updated Sept. 20, 2022 | Print
20
Sickle cell anemia, which primarily affects Black people, can shorten life expectancy by more than 20 years.
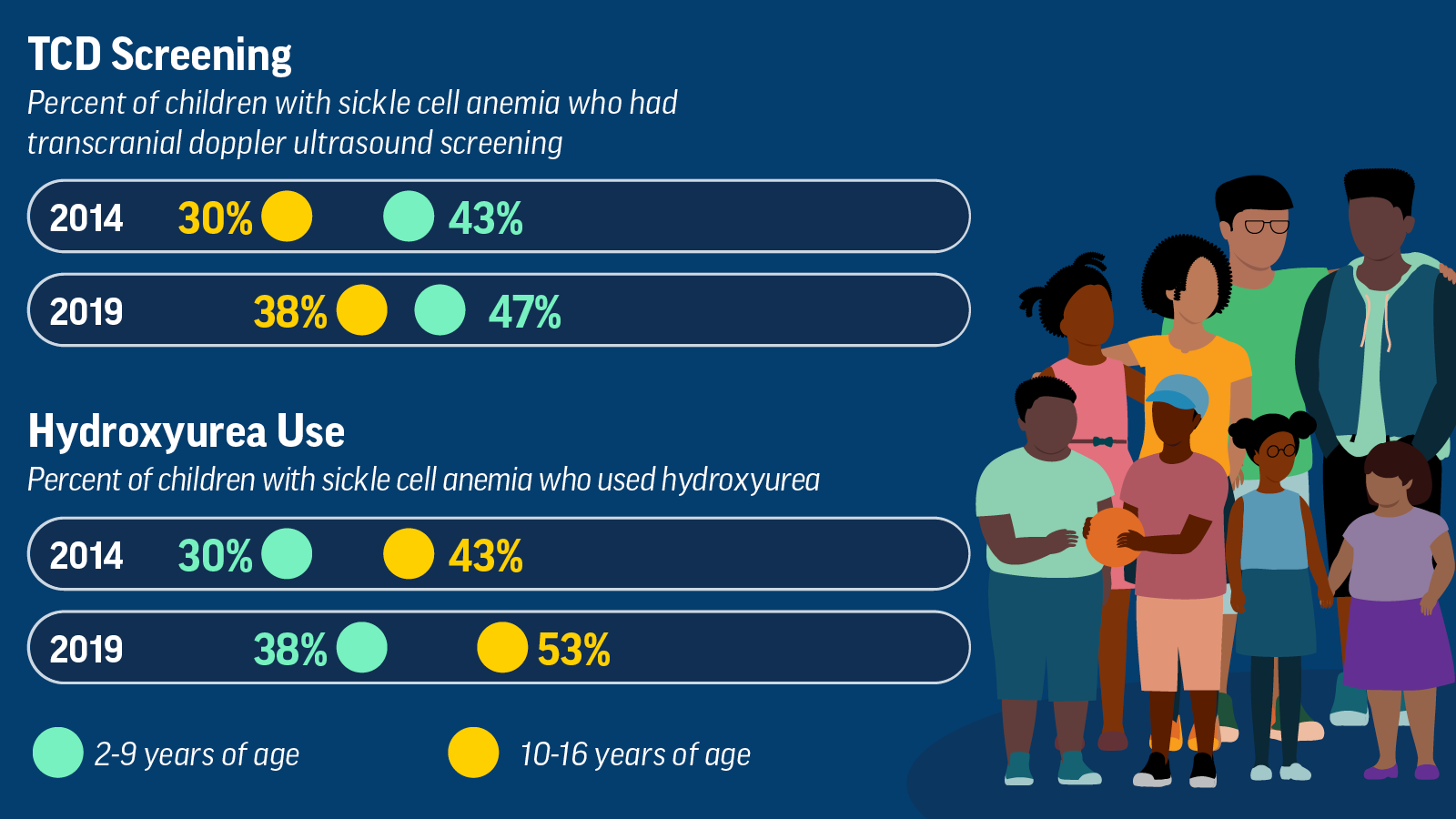
50%
Fewer than half of children 2–16 years received the recommended screening for stroke in 2019.
2 in 5
Only 2 in 5 children 2–9 years used recommended medication that can prevent sickle cell anemia complications in 2019.
Challenges
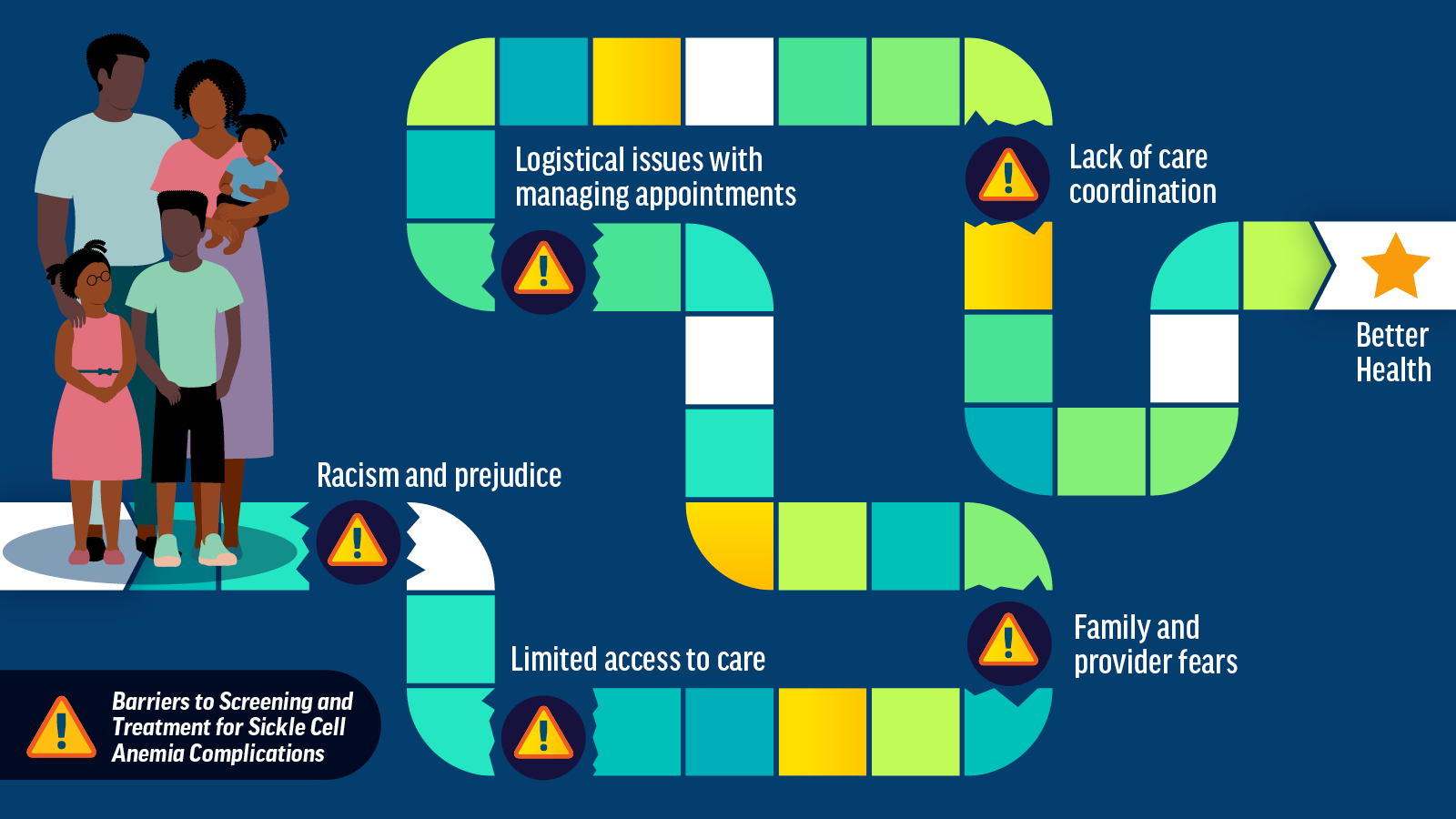
Barriers to Care
- Limited access to care: There is a shortage of healthcare providers with expertise in treating patients with sickle cell anemia. Many providers may be unfamiliar with TCD screening and hydroxyurea guidelines.
- Family and provider fears: Fears of potential hydroxyurea side effects and uncertainty about whether the medicine will work can lead to low use.
- Logistical issues with managing appointments: Hydroxyurea therapy requires regular monitoring and laboratory visits. Availability of TCD screening appointments may be limited. Radiology centers that perform TCD screening may be far from where a child receives regular care.
- Lack of care coordination: Lack of timely information from radiology centers can make it hard for providers to track patients who are due for TCD screening.
- Racism and prejudice: Prejudice, discrimination, and bias against people with sickle cell anemia can lead to poor, unequal care. Policies leading to unequal opportunities in housing, employment, and health insurance access widen healthcare gaps and inequalities.
Too Few Children with Sickle Cell Anemia Are Getting Recommended Screening and Treatment
Despite recent improvements, many children with sickle cell anemia are still not receiving transcranial doppler ultrasound screenings and/or using hydroxyurea.
Children with Sickle Cell Anemia Face Barriers That Make It Hard to Get Care
While multiple paths can lead to better health, barriers to care widen health inequities for children with sickle cell anemia.
What Can Be Done
email_03Vital Signs Update
Get email updates about Vital Signs
VITAL SIGNS RESOURCES