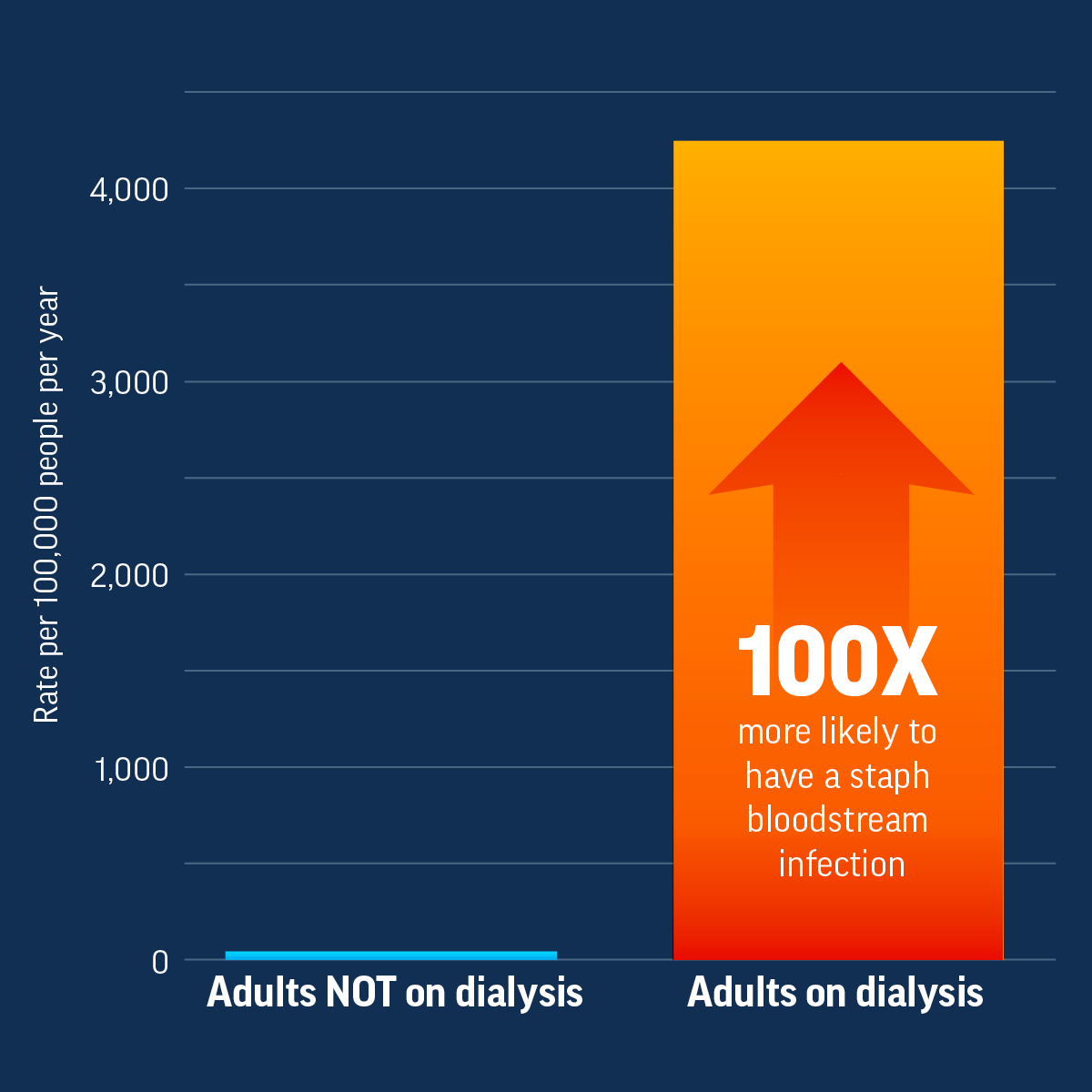
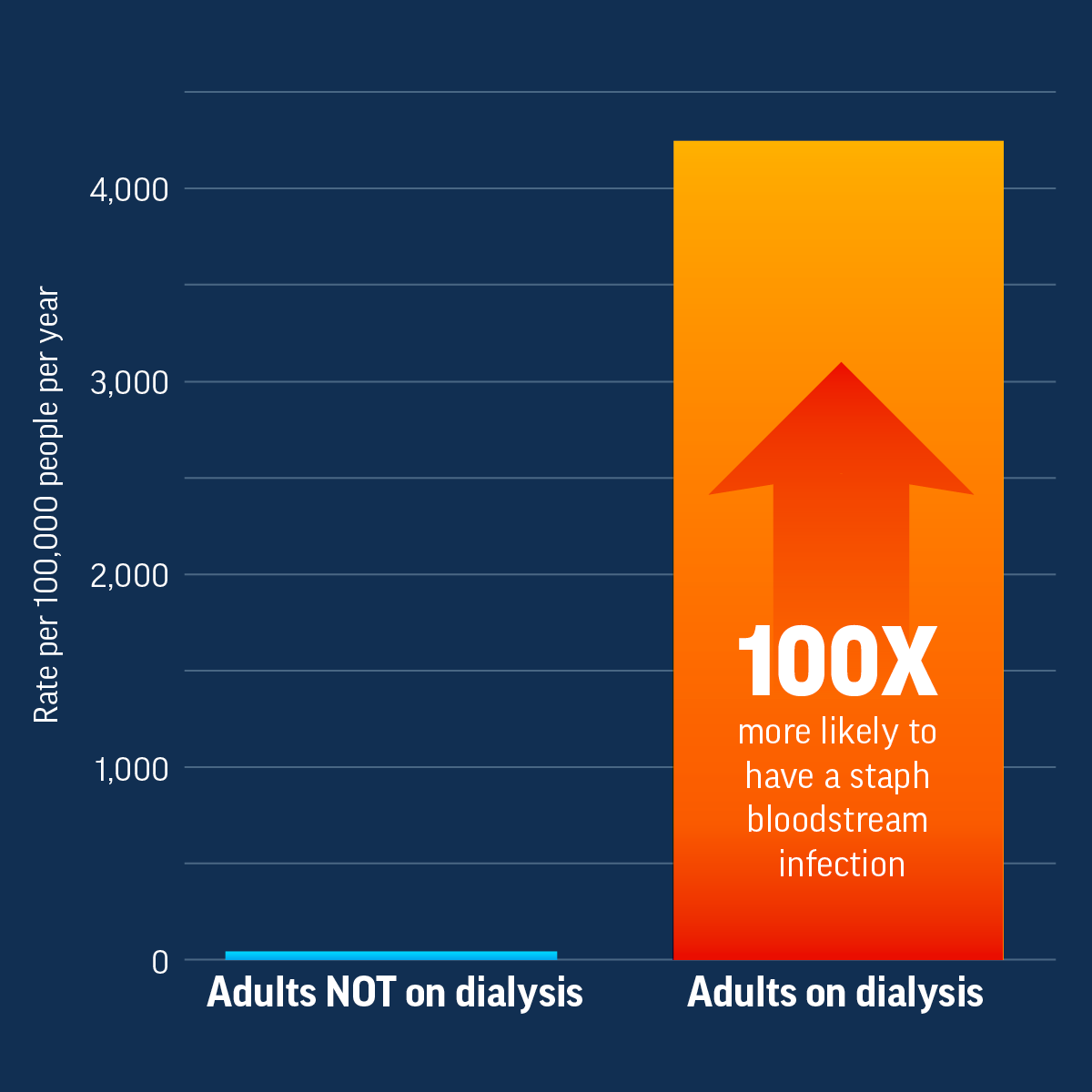
High risk for infection: Infections are common among patients on dialysis. These patients are more likely to get a staph bloodstream infection than people not on dialysis. Staph bloodstream infections can be serious or lead to death, and some infections are resistant to some of the most common antibiotics used to treat them, making the drugs ineffective.
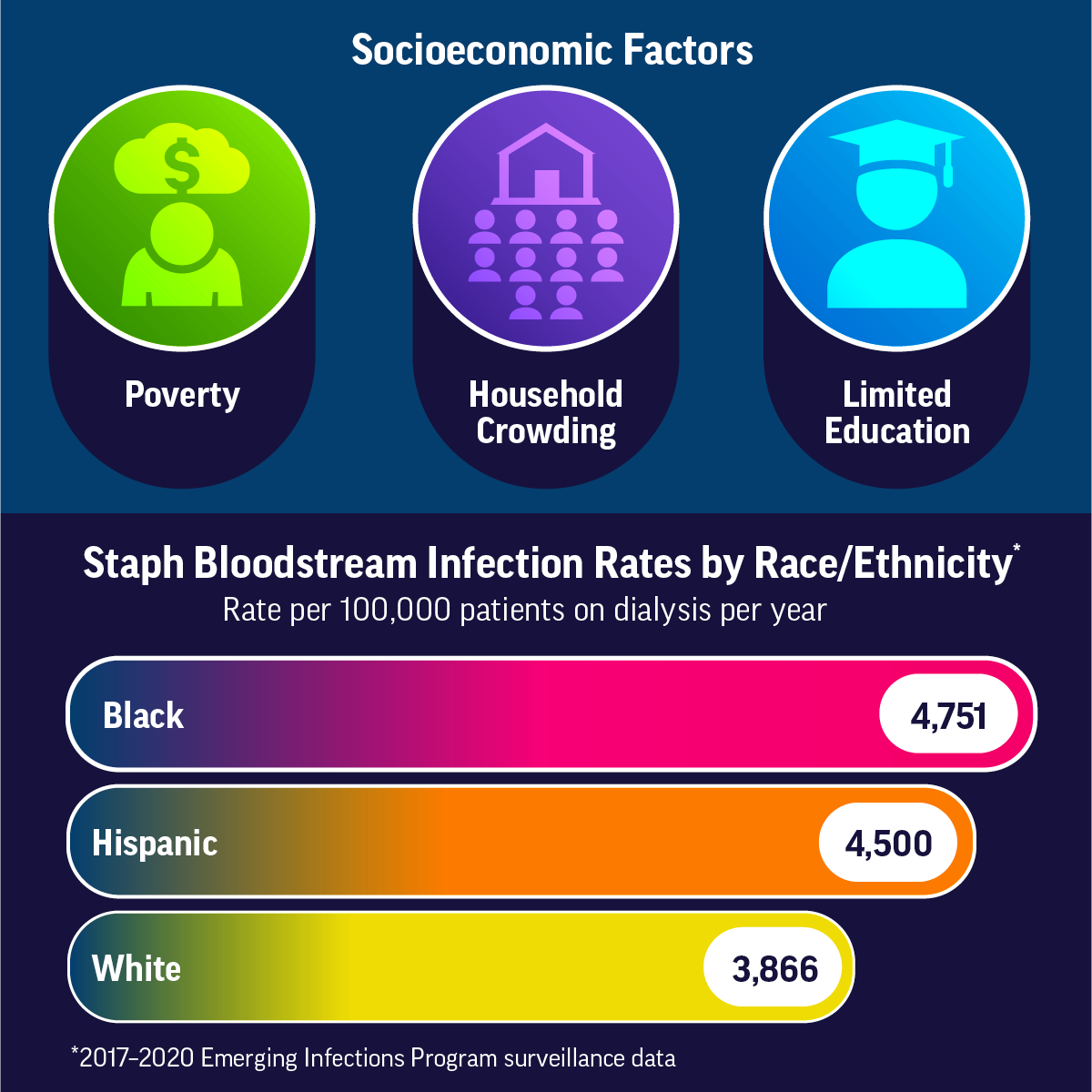
Racial and ethnic gaps: End-stage kidney disease affects Black and Hispanic people more than White people. Black and Hispanic people have greater numbers of medical conditions, such as high blood pressure and diabetes, which increase their risk of developing end-stage kidney disease. There are also differences in the types of therapies and treatments that Black and Hispanic patients receive for end-stage kidney disease. In addition, more Black and Hispanic patients on dialysis get staph bloodstream infections than White patients on dialysis.
Social and economic factors: Lack of prevention and care of kidney disease, socioeconomic and insurance status, and lack of patient education about treatment options are all factors in end-stage kidney disease treatment differences.
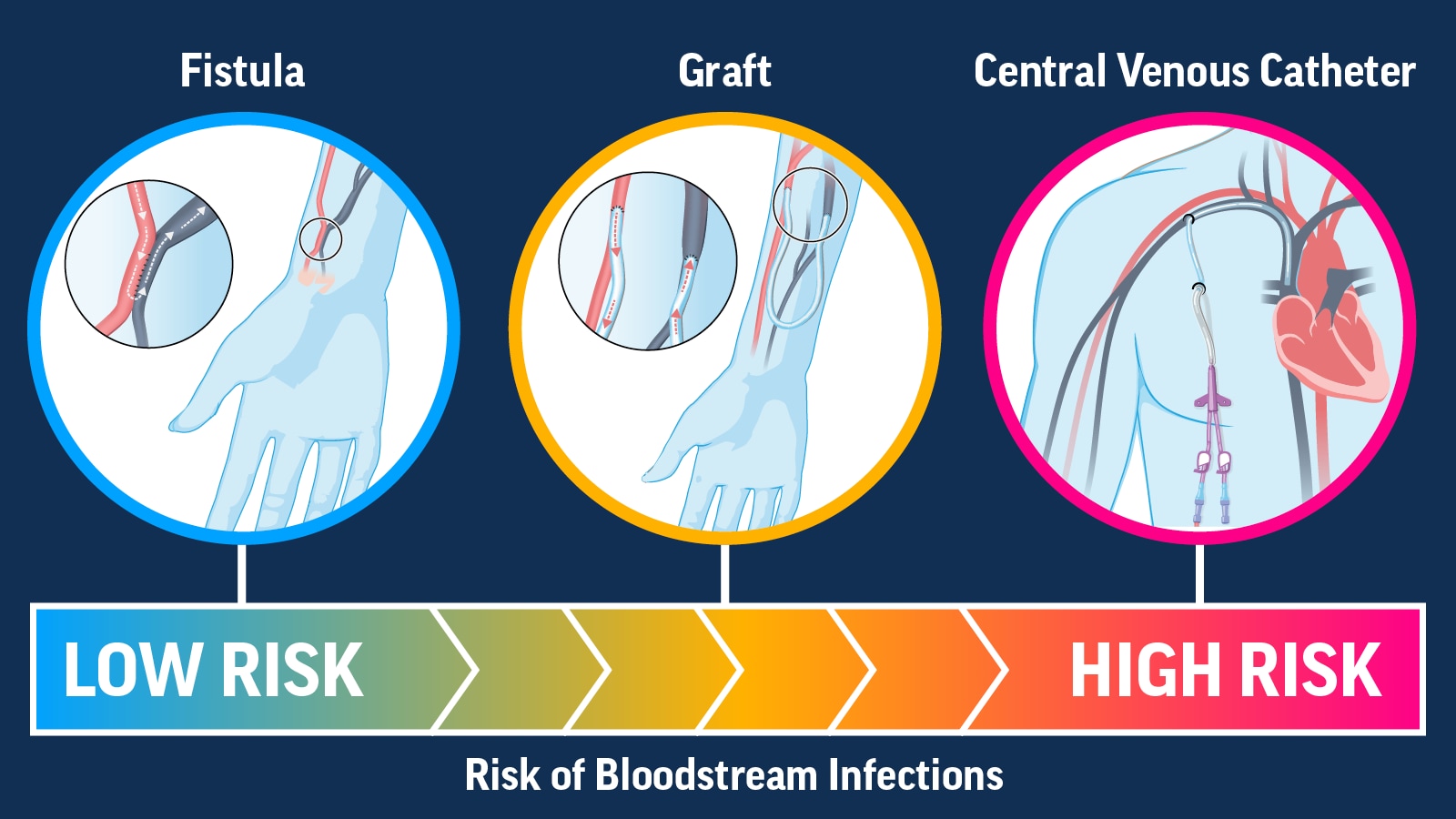
Catheter use: Vascular access type is the major risk factor for bloodstream infections regardless of race, ethnicity, or socioeconomic status. There are three access types: fistula, graft, and central venous catheter. People with any access type can develop an infection, but fistulas have the lowest risk of infection and central venous catheters have the highest risk of infection.
Increase Use of Lower-Risk Vascular Access Types for Dialysis
Reducing the use of central venous catheters for people on dialysis can help prevent bloodstream infections.
Use Proven Practices
- Follow CDC’s approach to bloodstream infection prevention in dialysis facilities, which has been shown to help reduce infections.
- Raise awareness and promote use of CDC audit tools and checklists for recommended infection prevention practices.
- Act fast if you suspect sepsis. Know sepsis signs and symptoms to identify and treat patients early.
Support Catheter Reduction
- Educate patients and staff about end-stage kidney disease therapies, including kidney transplant and vascular access options for dialysis, with culturally appropriate materials in their preferred language. When appropriate, refer patients to vascular access surgeons and assess patients for transplant suitability.
- Identify and address barriers to central venous catheter removal and placement of permanent vascular access types, such as fistulas and grafts.
- Promote education and partnership initiatives like the Making Dialysis Safer for Patients Coalition and the End Stage Renal Disease Network Program.
Everyone can:
- Prevent chronic kidney disease by managing diabetes and high blood pressure. Learn about chronic kidney disease and its risk factors.
- Read and share infection prevention resources for patients on dialysis.
- Clean your hands often with alcohol-based hand sanitizer or soap and water to prevent the spread of germs.
- Watch for signs of infection and its complications, like sepsis.
Get email updates about Vital Signs
VITAL SIGNS RESOURCES