Moderate and Severe TBI
Also, see:
A moderate or severe TBI is caused by a bump, blow, or jolt to the head or by a penetrating injury (such as from a gunshot) to the head. In the United States, severe TBIs are linked to thousands of deaths each year.1
For those who survive, a moderate or severe TBI may lead to long-term or life-long health problems that may affect all aspects of a person’s life. These health problems have been described as being similar to the effects of a chronic disease.2
Falls and firearm-related injuries lead to most moderate and severe TBIs
Research shows:
- Falls are one of the leading causes of TBI-related hospitalizations among Americans, especially among older adults (age 75 years and older)3
- Firearm-related suicide is linked to many TBI-related deaths in the United States4,5
- Motor vehicle crashes and assaults are other common ways a person may get a moderate or severe TBI3
Moderate and severe TBIs are serious and costly
A person with a moderate or severe TBI may need ongoing care to help with their recovery. A moderate or severe TBI not only impacts the life of an individual and their family, but it also has a large societal and economic toll. The lifetime economic cost of TBI, including direct and indirect medical costs, was estimated to be approximately $76.5 billion (in 2010 dollars).6 Additionally, the cost of fatal TBIs and TBIs requiring hospitalization account for approximately 90% of total TBI medical costs.6
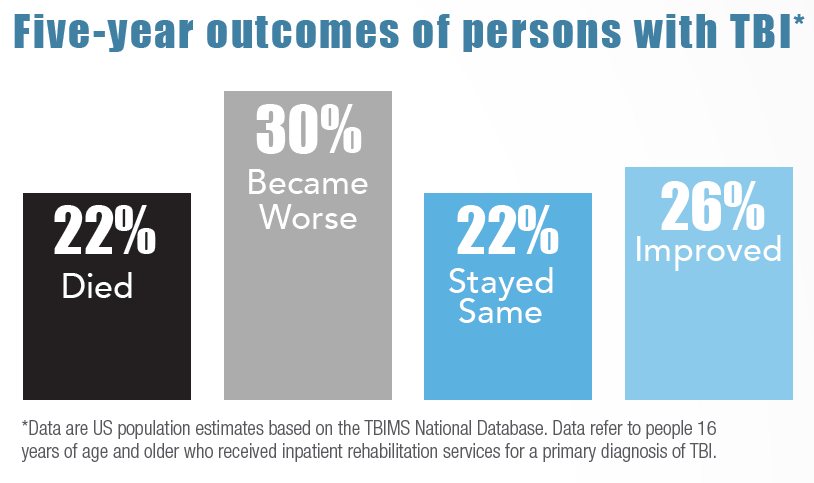
Five-year outcomes of persons with (Traumatic Brain Injury) TBI: 22% died, 30% became worse, 22% stayed same, and 26% improved. Data are US population estimates based on the TBIMS National Database. *Data refer to people 16 years of age and older who received inpatient rehabilitation services for a primary diagnosis of TBI.
- Iaccarino C, Carretta A, Nicolosi F, Morselli C. Epidemiology of severe traumatic brain injury. J Neurosurg Sci. 2018 Oct;62(5):535-541.
- MaselBE, DeWitt D. Traumatic brain injury: a disease process, not an event. J Neurotrauma. 2010;27(8):1529-1540.
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Surveillance report of traumatic brain injury-related emergency department visits, hospitalizations, and deaths—United States, 2014. Atlanta (GA): Centers for Disease Control and Prevention; 2019.
- Daugherty J, Waltzman D, Sarmiento K, Xu L. Traumatic brain injury–related deaths by race/ethnicity, sex, intent, and mechanism of injury — United States, 2000–2017. MMWR Morb Mortal Wkly Rep. 2019;68(46):1050-1056.
- Miller GF, Kegler SR, Stone DM. Traumatic brain injury–related deaths from firearm suicide: United States, 2008–2017. AJPH. 2020(0):e1-e3.
- Finkelstein E, Corso P, Miller T and associates. The Incidence and Economic Burden of Injuries in the United States. New York (NY): Oxford University Press; 2006.
