Social Determinants of Health at CDC
Social determinants of health (SDOH) are the nonmedical factors that influence health outcomes. They are the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life. These forces and systems include economic policies and systems, development agendas, social norms, social policies, racism, climate change, and political systems. Centers for Disease Control and Prevention (CDC) has adopted this SDOH definition from the World Health Organization.
What is CDC Doing to Address SDOH?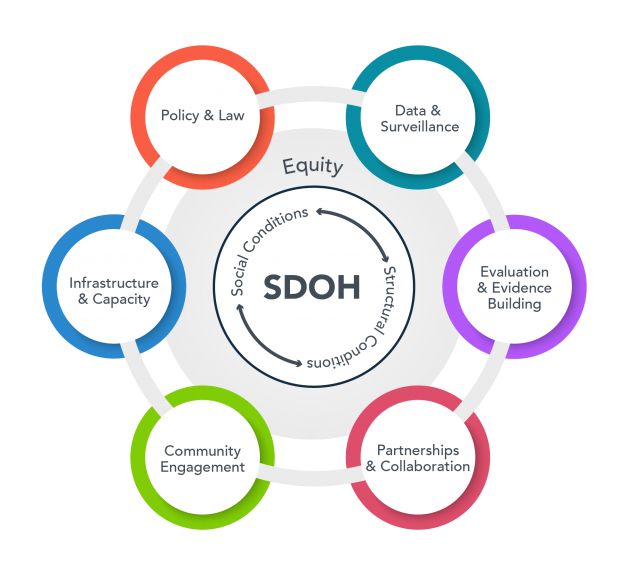
SDOH are one of three priority areas for Healthy People 2030, along with health equity and health literacy. Healthy People 2030 sets data-driven national objectives in five key areas of SDOH: healthcare access and quality, education access and quality, social and community context, economic stability, and neighborhood and built environment. Some examples of SDOH included in Healthy People 2030 are safe housing, transportation, and neighborhoods; polluted air and water; and access to nutritious foods and physical health opportunities.
Public health organizations can convene, integrate, influence, and contribute to big changes.
CDC has taken multiple steps to ensure efforts to address SDOH are built into the agency’s work.
CDC SDOH Resources
- National Center for HIV, Viral Hepatitis, STD, and TB Prevention (NCHHSTP)
- Public Health Infrastructure Center (PHIC)
- National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP)
- Adverse Childhood Experiences at the National Center for Injury Prevention and Control (NCIPC)
- Health Impact in 5 Years (OPPE)
Additional SDOH Resources
SDOH Publications
- Hacker K, Auerbach J, Ikeda R, Philip C, Houry D; SDOH Task Force. Social determinants of health—an approach taken at CDC. J Public Health Manag Pract. 2022;28(6):589-594. doi: 10.1097/PHH.0000000000001626
- Hacker K, Houry D. Social needs and social determinants: the role of the Centers for Disease Control and Prevention and public health. Public Health Rep. 2022; Sep 9:00333549221120244.
- JPHMP Direct. CDC’s Approach to Social Determinants of Health. Accessed October 31, 2022. https://jphmpdirect.com/2022/10/07/cdcs-approach-to-social-determinants-of-health/