What to know
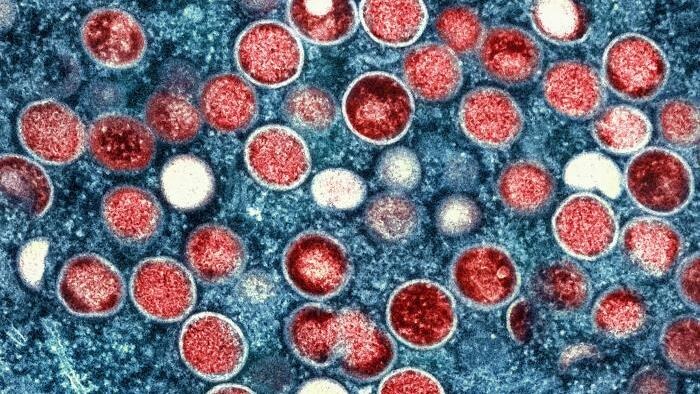
- There are two types of the virus that causes monkeypox, clade I and clade II. Both types can be spread, treated, and prevented in the same ways.
- There have been more than 46,000 cases of clade I monkeypox related to the outbreak in Central and Eastern Africa.
- There also have been many travel-associated clade I monkeypox cases around the globe, including recent outbreaks in some European countries.
- Clade II monkeypox cases continue to spread at low levels worldwide.
- CDC works with public health partners across the world to monitor for cases and prevent monkeypox from spreading.
Current situation
In the United States
- Since November 2024, there have been 11 reported cases of clade I monkeypox in the United States. These cases were in people who had recently traveled to areas associated with the outbreak in Central and Eastern Africa, or who were linked to people who'd traveled from these areas.
- This number includes three clade I monkeypox cases reported in October 2025 in people with no recent travel. Viral genomic (DNA fingerprint) data indicate that these three cases are linked to a different U.S. case reported in August 2025 following travel to an area with a known clade I monkeypox outbreak.
- This number includes three clade I monkeypox cases reported in October 2025 in people with no recent travel. Viral genomic (DNA fingerprint) data indicate that these three cases are linked to a different U.S. case reported in August 2025 following travel to an area with a known clade I monkeypox outbreak.
- The risk posed by the clade I monkeypox outbreak to most people within the United States remains low.
- Clade II monkeypox is still circulating at low levels.
- CDC noted a summer 2025 uptick of U.S. cases of clade II across several different states, some of which were linked to an outbreak of clade II monkeypox in Sierra Leone, Liberia, and other West African countries.
- CDC noted a summer 2025 uptick of U.S. cases of clade II across several different states, some of which were linked to an outbreak of clade II monkeypox in Sierra Leone, Liberia, and other West African countries.
Cases of clade I monkeypox originated in Central and Eastern Africa but have spread worldwide.
Clade II monkeypox is spreading in the United States and around the world.
Across the globe
- There are outbreaks of clade I monkeypox in Central and Eastern Africa.
- Clade I has two subclades, clade Ia and clade Ib.
- Based on what we know from recent outbreaks, clade Ib monkeypox has a lower case-fatality rate (less than 0.5%) than clade Ia monkeypox (about 2.5%).
- In Central Africa, people have gotten clade Ia monkeypox through contact with infected dead or live wild animals, household transmission, or patient care.
- Subclade Ib is a more recently discovered strain identified in the eastern part of the Democratic Republic of the Congo. Clade Ib is mostly spread initially through intimate or sexual contact, followed by spread within households.
- Sustained and local person-to-person spread of clade I monkeypox has taken place in some non-endemic countries through intimate or sexual contact, day-to-day household contact, and within the healthcare setting in the absence of personal protective equipment.
- Travel-associated cases of clade I monkeypox have occurred in several countries in Africa, Asia, Europe, the Middle East, North America, and South America, as well as in Australia.
- Beginning in Fall 2025, several countries in Western Europe began reporting clade Ib monkeypox cases among individuals who had no documented history of international travel. These cases were likely related to sexual exposure. We expect additional cases in Europe and the United States.
- To date, there have been more than 150 clade Ib cases in high-income countries since January 2024, and no deaths have been reported.
- The ongoing global outbreak of clade IIb monkeypox has caused more than 100,000 cases in 122 total countries, including 115 countries where monkeypox was not previously reported.
- Several countries in West Africa have been experiencing an outbreak of clade II monkeypox since Summer 2025.
- Travelers to Liberia should review the Travel Health Notice, which includes information about the monkeypox vaccine for eligible people.
Global monkeypox case data
For global case data for clade I and clade II monkeypox since January 1, 2024, see 2022-24 Mpox (Monkeypox) Outbreak: Global Trends (shinyapps.io). Confirmed cases include those that are laboratory confirmed as monkeypox virus and may include cases only confirmed as orthopoxvirus. These data are provided for situational awareness and are subject to change.
What CDC is doing
In Africa
- CDC continues critical work to protect the United States from emerging and infectious diseases. CDC has collaborated closely with key partners in affected countries to help support efforts to stop monkeypox at the source.
- CDC and in-country partners across Africa have worked together on disease surveillance, laboratory capacity-building, strengthening local workforce capacity, case investigation, strengthening case management, infection prevention and control, and vaccine strategy and planning.
- CDC collaborated with governmental and civil society partners in affected countries to collect and analyze case data, and to identify how monkeypox is spreading.
- CDC trained 80 field epidemiologists in DRC and continues to provide key support for many who are still working in priority health zones. These CDC-trained epidemiologists are playing a key role in DRC efforts to detect cases, trace and monitor contacts, and increase community awareness of monkeypox, while also collecting and sending specimens to labs for testing, and training healthcare workers to do the same.
- CDC is coordinating technical assistance in response to urgent needs identified by national governments and local partners in the areas of laboratory, surveillance, risk communication and community engagement, case management, infection prevention and control, psychosocial support, and vaccine planning.
- The U.S. government is also working closely with several other countries in the region to assist with monitoring the situation as new information becomes available.
- CDC's staff stationed in several countries affected by or on the border with countries with monkeypox cases provide critical information to inform U.S. preparedness efforts. Staff are connected to CDC's response efforts and can provide critical, real-time information to inform CDC's understanding of the outbreak, mitigate importation of cases into the U.S., and inform U.S. preparedness efforts.
- Response efforts include increasing the number of monkeypox testing sites; improving specimen transport networks to quickly identify new cases; assisting with Ministry of Health-led vaccine implementation; strengthening emergency management systems; improving case surveillance; and training healthcare workers on infection prevention and control.
In the United States
- CDC works closely with state, tribal, local, and territorial public health departments to provide recommendations for clinical management, diagnosis, and prevention of monkeypox cases in the U.S.
- CDC continually increases capacity in communities across the United States for early detection of monkeypox through existing surveillance systems, including wastewater testing.
- CDC raises awareness for healthcare providers, including the latest guidance for considering monkeypox as a possible diagnosis in certain patients.
- CDC has information and recommendations for members of the public, including those traveling to Central or Eastern Africa: Travel Health Notice and Health Alert Network advisory.
- CDC works with researchers and partner organizations to increase health equity around monkeypox and ensure that the populations most affected by monkeypox have access to the monkeypox vaccine.
Resources
- Get monkeypox and other vaccine recommendations when traveling to areas with monkeypox outbreaks: Destinations | Travelers' Health | CDC
- Clade II Monkeypox in Liberia and Sierra Leone - Level 2 - Practice Enhanced Precautions - Travel Health Notices | Travelers' Health | CDC
- U.S. Monkeypox Wastewater Data | National Wastewater Surveillance System | CDC
- Health Alert Network (HAN) - 00519 | First Case of Clade I Monkeypox Diagnosed in the United States
- Health Alert Network (HAN) - 00516 | Prevention Strategies for Monkeypox, including Vaccinating People at Risk via Sexual Exposure, for U.S. Travelers Visiting Countries with Clade I Monkeypox Outbreaks
- Health Alert Network (HAN) – 00513 | Monkeypox Caused by Human-to-Human Transmission of Monkeypox Virus in the Democratic Republic of the Congo with Spread to Neighboring Countries (cdc.gov)
- Health Alert Network (HAN) – 00501 | Monkeypox Caused by Human-to-Human Transmission of Monkeypox Virus with Geographic Spread in the Democratic Republic of the Congo
- The CDC Domestic Monkeypox Response — United States, 2022–2023
- U.S. Preparedness and Response to Increasing Clade I Monkeypox Cases in the Democratic Republic of the Congo — United States, 2024
- Notes from the Field: Clade II Monkeypox Surveillance Update — United States, October 2023–April 2024
- Early Release - The Rise of Monkeypox in a Post-Smallpox World - Volume 31, Number 1—January 2025 - Emerging Infectious Diseases journal - CDC
