Increase in Measles Cases — United States, January 1–April 26, 2019
Weekly / May 3, 2019 / 68(17);402–404
On April 29, 2019, this report was posted online as an MMWR Early Release.
Manisha Patel, MD1; Adria D. Lee, MSPH1; Susan B. Redd1; Nakia S. Clemmons, MPH1; Rebecca J. McNall, PhD1; Amanda C. Cohn, MD2; Paul A. Gastañaduy, MD1 (View author affiliations)
View suggested citationSummary
What is already known about this topic?
Measles was eliminated in the United States in 2000.
What is added by this report?
During January 1–April 26, 2019, a total of 704 cases were reported, the highest number of cases reported since 1994. Outbreaks in close-knit communities accounted for 88% of all cases. Of 44 cases directly imported from other countries, 34 were in U.S. residents traveling internationally; most were not vaccinated.
What are the implications for public health practice?
Unvaccinated U.S. residents traveling internationally are at risk for acquiring measles. Close-knit communities with low vaccination rates are at risk for sustained measles outbreaks. High coverage with measles, mumps, rubella (MMR) vaccination is the most effective way to limit transmission and maintain elimination of measles in the United States.
Altmetric:
As of April 26, 2019, CDC had reported 704 cases of measles in the United States since the beginning of 2019, representing the largest number of cases reported in the country in a single year since 1994, when 963 cases occurred, and since measles was declared eliminated* in 2000 (1,2). Measles is a highly contagious, acute viral illness characterized by fever and a maculopapular rash; complications include pneumonia, encephalitis, and death. Among the 704 cases, 503 (71%) were in unvaccinated persons and 689 (98%) occurred in U.S. residents. Overall, 66 (9%) patients were hospitalized. Thirteen outbreaks have been reported in 2019, accounting for 663 cases, 94% of all reported cases. Six of the 13 outbreaks were associated with underimmunized close-knit communities and accounted for 88% of all cases. High 2-dose measles vaccination coverage in the United States has been critical to limiting transmission (3). However, increased global measles activity poses a risk to U.S. elimination, particularly when unvaccinated travelers acquire measles abroad and return to communities with low vaccination rates (4). Health care providers should ensure persons are up to date with measles, mumps, rubella (MMR) vaccine, including before international travel, and rapidly report all suspected cases of measles to public health authorities.
Measles cases are classified according to the Council of State and Territorial Epidemiologists’ case definition for measles (5). Cases are considered to be internationally imported if at least part of the exposure period (7–21 days before rash onset) occurred outside the United States and rash occurred within 21 days of entry into the United States, with no known exposure to measles in the United States during the exposure period. An outbreak of measles is defined as a chain of transmission of three or more cases linked in time and place and is determined by local and state health department investigations.
During January 1–April 26, 2019, a total of 704 measles cases were reported in 22 states (Figure 1); the highest number of weekly cases (87) were reported during the week ending March 23 (Figure 2). Median patient age was 5 years (interquartile range = 1 year to 18.5 years); 25 (4%) patients were aged <6 months, 68 (10%) 6–11 months, 76 (11%) 12–15 months, 167 (24%) 16 months–4 years, 203 (29%) 5–19 years, 138 (20%) 20–49 years, and 27 (4%) ≥50 years (Table). Among all measles patients, 503 (71%) were unvaccinated, 76 (11%) were vaccinated (received ≥1 measles, mumps, and rubella (MMR) vaccine), and the vaccination status of 125 (18%) was unknown. Overall, 66 (9%) patients were hospitalized, and 24 (3%) had pneumonia. No deaths or cases of encephalitis were reported to CDC.
Of the 704 total cases, 663 (94%) were associated with outbreaks; 13 outbreaks have been reported in 2019. Outbreak-related cases have been reported in 12 states† and New York City; multistate transmission was documented in four outbreaks. Six outbreaks were associated with underimmunized close-knit communities and accounted for 88% of all cases. New York state and New York City accounted for 474 (67%) of all cases reported in 2019 and have had ongoing transmission since October 2018.
Among the 704 cases, 689 (98%) occurred in U.S. residents. Forty-four cases were directly imported from other countries, including 34 (77%) that occurred in U.S. residents; 23 imports resulted in no known secondary cases. Among the 44 internationally imported measles cases, 40 (91%) were in unvaccinated persons or persons whose vaccination status was unknown; all 40 were age-eligible for vaccination, including two infant travelers aged 6–11 months. Source countries included Philippines (14 cases), Ukraine (8), Israel (5), Thailand (3), Vietnam (2), Germany (2), and one importation each from Algeria, France, India, Lithuania, Russia, and the United Kingdom. Four travelers went to multiple countries during their exposure period, including Italy/Singapore, Thailand/Cambodia, Ukraine/Israel, and Cambodia/Thailand/China/Singapore. Among 245 (35%) cases for which molecular sequencing was performed, B3 and D8 were the only genotypes identified, which were the most commonly detected genotypes worldwide in the past 12 months.
Discussion
Before 2019, the highest number of measles cases following elimination in the United States occurred in 2014, when 667 cases were reported; 383 (57%) of those cases were associated with an outbreak in an underimmunized Amish community in Ohio (6). Worldwide, 7 million measles cases are estimated to occur annually, and since 2016, measles incidence has increased in five of the six World Health Organization regions (7), contributing to increased opportunities for measles importations into the United States. Fortunately, the mjority of importations do not lead to outbreaks because of rapid implementation of control measures by state and local health departments. Additionally, the United States benefits from a long-standing vaccination program, with overall measles vaccination coverage of >91% in children aged 19–35 months (8). However, unimmunized or underimmunized subpopulations within U.S. communities are at risk for large outbreaks of long duration that are resource intensive to control (9). Recent outbreaks have been driven by misinformation about measles and MMR vaccine, which has led to undervaccination in vulnerable communities.
Unvaccinated U.S. residents traveling internationally are at risk for acquiring measles. Health care providers should vaccinate persons without contraindications and without acceptable evidence of immunity to measles before travel to any country outside the United States. Only written (not self-report) documentation of age-appropriate vaccination, laboratory evidence of immunity, laboratory confirmation of disease, or birth before 1957 is considered acceptable presumptive evidence of immunity. In addition to routine recommendations for MMR vaccination (3), infants aged 6–11 months should receive 1 dose of MMR vaccine, and adults should receive a second dose before international travel (3); infants who receive MMR vaccine before their first birthday should receive 2 additional doses (1 dose at age 12–15 months and another dose at least 28 days after the first dose). Measles is a nationally notifiable disease in the United States; health care providers should rapidly report all cases of suspected measles to public health authorities to ensure that timely control measures are implemented. High coverage with MMR vaccine is the most effective strategy to limit transmission and maintain elimination of measles in the United States.
Corresponding author: Manisha Patel, ncirddvdmmrhp@cdc.gov, 404-718-5440.
1Division of Viral Diseases, National Center for Immunization and Respiratory Diseases, CDC; 2Office of the Director, National Center for Immunization and Respiratory Diseases, CDC.
All authors have completed and submitted the ICMJE form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
* Defined as absence of sustained measles transmission that is continuous for ≥12 months in a defined geographic area.
† California, Connecticut, Georgia, Illinois, Maryland, Michigan, Missouri, New Jersey, New York, Oregon, Texas, and Washington.
References
- Clemmons NS, Wallace GS, Patel M, Gastañaduy PA. Incidence of measles in the United States, 2001–2015. JAMA 2017;318:1279–81. CrossRef PubMed
- CDC. National Notifiable Diseases Surveillance System (NNDSS). Atlanta, GA: US Department of Health and Human Services, CDC; 2019. https://wwwn.cdc.gov/nndss/default.aspx
- McLean HQ, Fiebelkorn AP, Temte JL, Wallace GS. Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: summary recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2013;62(No. RR-4). PubMed
- Lee AD, Clemmons NS, Patel M, Gastañaduy PA. International importations of measles virus into the United States during the postelimination era, 2001–2016. J Infect Dis 2019;219:1616–23. CrossRef PubMed
- CDC. National Notifiable Diseases Surveillance System (NNDSS). Measles/rubeola 2013 case definition. Atlanta, GA: US Department of Health and Human Services, CDC; 2019. https://wwwn.cdc.gov/nndss/conditions/measles/case-definition/2013/
- Gastañaduy PA, Budd J, Fisher N, et al. A measles outbreak in an underimmunized Amish community in Ohio. N Engl J Med 2016;375:1343–54. CrossRef PubMed
- Dabbagh A, Laws RL, Steulet C, et al. Progress toward regional measles elimination—worldwide, 2000–2017. MMWR Morb Mortal Wkly Rep 2018;67:1323–9. CrossRef PubMed
- Hill HA, Elam-Evans LD, Yankey D, Singleton JA, Kang Y. Vaccination coverage among children aged 19–35 months—United States, 2017. MMWR Morb Mortal Wkly Rep 2018;67:1123–8. CrossRef PubMed
- CDC. Measles cases and outbreaks: measles cases in 2019. Atlanta, GA: US Department of Health and Human Services, CDC; 2019. https://www.cdc.gov/measles/cases-outbreaks.html
 FIGURE 1. Number of reported measles cases (N = 704) — United States, January 1–April 26, 2019*
FIGURE 1. Number of reported measles cases (N = 704) — United States, January 1–April 26, 2019*
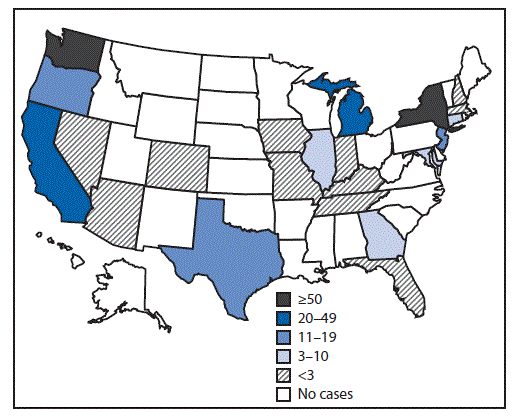
* Data are preliminary as of April 26, 2019.
 FIGURE 2. Number of reported measles cases (N = 704), by week of rash onset — United States, January 1–April 26, 2019*
FIGURE 2. Number of reported measles cases (N = 704), by week of rash onset — United States, January 1–April 26, 2019*
* Data are preliminary as of April 26, 2019. Data for the week ending April 27 are for a partial week.
* Data are preliminary as of April 26, 2019.
† Percentages are of all 44 international importations.
Suggested citation for this article: Patel M, Lee AD, Redd SB, et al. Increase in Measles Cases — United States, January 1–April 26, 2019. MMWR Morb Mortal Wkly Rep 2019;68:402–404. DOI: http://dx.doi.org/10.15585/mmwr.mm6817e1.
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (https://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.