Notes from the Field: Measles Outbreak in an Era of Stricter Immunization Requirements — California, March 2018
Weekly / March 1, 2019 / 68(8);201–202
George Han, MD1; Neale Batra, MSc1,2; Alvin Vallejo1; Robert Schechter, MD3; Jennifer Zipprich, PhD3; Kathleen Harriman, PhD3 (View author affiliations)
View suggested citationAltmetric:
On March 4, 2018, an unvaccinated adolescent boy (patient A, aged 15 years) who had recently returned from England and Wales, where measles outbreaks were occurring, was evaluated by a physician for fever, cough, coryza, conjunctivitis, Koplik spots, and rash. Measles virus nucleic acid was detected in an oropharyngeal swab and in urine tested at the Santa Clara County (California) Public Health Department (SCCPHD). Nineteen days later, on March 23, measles was reported in an unvaccinated adolescent boy (patient B, aged 16 years) who had been at a scouting event with patient A (Figure). Patient B was not contacted during public health investigation because patient A had not reported attending this event. On March 24, an unvaccinated male classmate of patient A’s (patient C, aged 15 years) developed measles while in quarantine. On April 2, a man (patient D, aged 21 years) who had received 2 doses of measles, mumps, and rubella (MMR) vaccine and who had attended a different scouting event in Santa Clara County with patient B before returning to college in Nevada was reported as a measles patient to the Washoe County (Nevada) Health District.
On April 3, the Alameda County (California) Public Health Department received a report of measles in an unvaccinated man (patient E, aged 33 years). He identified his nephew (patient F, aged 7 years) as the source of his illness but declined to provide contact information. SCCPHD eventually confirmed his nephew’s presence at a tutoring center attended by patient A. The nephew’s parents could not be reached by phone; his mother was interviewed at their home. She acknowledged that her son was not vaccinated and revealed that both he and his unvaccinated brother (patient G, aged 4 years) had experienced recent illnesses consistent with measles. Hundreds of contacts of these seven patients were traced across 10 counties in California and Nevada.
Although patient A’s parents had chosen not to vaccinate him, his immunocompromised brother, an organ transplant recipient, had received intravenous immunoglobulin to protect him against measles before traveling overseas. When patient A’s illness was reported, SCCPHD recommended that his brother receive additional intravenous immunoglobulin and be quarantined 7 additional days; the family followed both recommendations. Patient C’s unvaccinated sister, aged 17 years, received parental permission to choose to receive MMR vaccine when her brother was quarantined; she opted to receive the vaccine. Patient D, who had received 2 doses of MMR vaccine, exhibited mild symptoms consistent with modified measles (1). None of his many contacts at a large university developed measles.
MMR vaccine is recommended for all persons born in the United States since 1957 who do not have a contraindication for the vaccine.* In this outbreak, the six unvaccinated patients with measles all had parents who had chosen not to vaccinate them during childhood. Since California Senate Bill 277 (SB277) went into effect in 2016, children entering school in California may no longer receive exemptions from immunization requirements based on parental personal beliefs.† However, medical exemptions for reasons determined by individual physicians, including family medical history, rather than a uniform standard (i.e., a medical contraindication to vaccination), remain permitted (2). Interviews with local health authorities suggest that some students without contraindications to vaccination have received medical exemptions (3). Patients F and G received identical broad medical exemptions to all vaccines from a physician located several hundred miles away from the patients’ residence. Patients E and G represent the first documented cases of measles in California infected by a child with a medical exemption since SB277 became law; had SCCPHD received accurate information about patient F’s immunization status, these two illnesses might have been prevented, and the expenditure of resources to investigate their contacts might have been avoided. Prompt public health action and continued maintenance of a high level of population immunity to measles likely averted a larger outbreak.
Acknowledgments
Brandon Bonin, Rebecca Quenelle, Santa Clara County Public Health Department, San Jose, California; Sandra Huang, Alameda County Public Health Department, Oakland, California; Cora Hoover, San Francisco Department of Public Health, San Francisco, California; Heather Holmstadt, Washoe County Health District, Reno, Nevada; Alex Espinosa, Rosie Glenn-Finer, Jill Hacker, California Department of Public Health.
Corresponding author: George Han, george.han@phd.sccgov.org.
1Santa Clara County Public Health Department, San Jose, California; 2California Epidemiologic Investigation Service; 3California Department of Public Health.
All authors have completed and submitted the ICMJE form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
References
- Rota JS, Hickman CJ, Sowers SB, Rota PA, Mercader S, Bellini WJ. Two case studies of modified measles in vaccinated physicians exposed to primary measles cases: high risk of infection but low risk of transmission. J Infect Dis 2011;204(Suppl 1):S559–63. CrossRef PubMed
- Delamater PL, Leslie TF, Yang YT. Change in medical exemptions from immunization in California after elimination of personal belief exemptions. JAMA 2017;318:863–4. CrossRef PubMed
- Mohanty S, Buttenheim AM, Joyce CM, Howa AC, Salmon D, Omer SB. Experiences with medical exemptions after a change in vaccine exemption policy in California. Pediatrics 2018;142:e20181051. CrossRef PubMed
 FIGURE. Measles transmission associated with community exposures to persons who had not received measles, mumps, and rubella vaccine, by date of rash onset — California, March 2018*,†
FIGURE. Measles transmission associated with community exposures to persons who had not received measles, mumps, and rubella vaccine, by date of rash onset — California, March 2018*,†
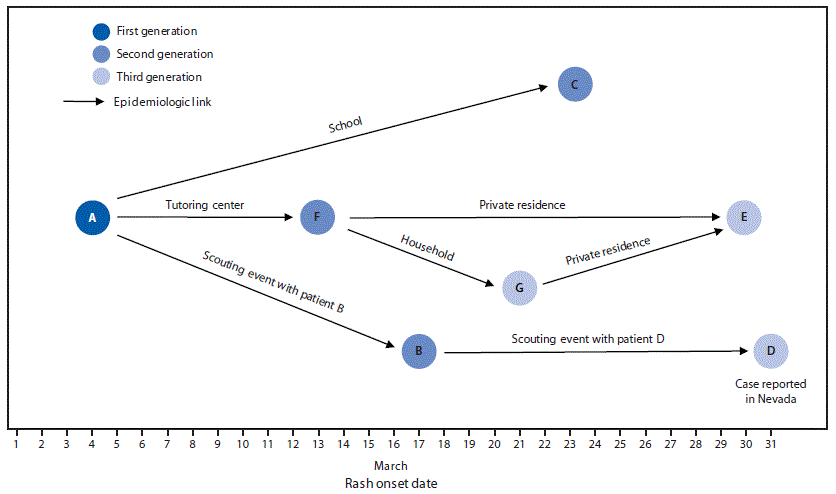
* Patients A–E had measles genotype D8. The parents of patients F and G did not consent to laboratory testing.
† Patient E could have been infected by either patient F or patient G during a visit to their home on March 17.
Suggested citation for this article: Han G, Batra N, Vallejo A, Schechter R, Zipprich J, Harriman K. Notes from the Field: Measles Outbreak in an Era of Stricter Immunization Requirements — California, March 2018. MMWR Morb Mortal Wkly Rep 2019;68:201–202. DOI: http://dx.doi.org/10.15585/mmwr.mm6808a3.
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (https://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.