Geographic Variation in Pediatric Cancer Incidence — United States, 2003–2014
Weekly / June 29, 2018 / 67(25);707–713
David A. Siegel, MD1,2; Jun Li, MD, PhD2; S. Jane Henley, MSPH2; Reda J. Wilson, MPH2; Natasha Buchanan Lunsford, PhD2; Eric Tai, MD2; Elizabeth A. Van Dyne, MD1,2 (View author affiliations)
View suggested citationSummary
What is already known about this topic?
Past research on nationwide pediatric cancer incidence described differences by U.S. Census region but did not provide state-level estimates.
What is added by this report?
During 2003–2014, the pediatric cancer rate was highest in the Northeast, lowest in the South, and highest in metropolitan areas with populations ≥1 million and counties in the top 25% economic status. Incidence rates by state ranged from 145 to 206 per million and were highest in New Hampshire, the District of Columbia, and New Jersey. The highest rate of leukemia was in the West; the highest rates of lymphoma and brain cancer were in the Northeast.
What are the implications for public health practice?
Knowledge of these geographic differences in childhood cancer incidence can be used to enhance provider awareness, treatment capacity, survivorship care, and cancer surveillance.
Altmetric:
Approximately 15,000 persons aged <20 years receive a cancer diagnosis each year in the United States (1). National surveillance data could provide understanding of geographic variation in occurrence of new cases to guide public health planning and investigation (2,3). Past research on pediatric cancer incidence described differences by U.S. Census region but did not provide state-level estimates (4). To adequately describe geographic variation in cancer incidence among persons aged <20 years in the United States, CDC analyzed data from United States Cancer Statistics (USCS) during 2003–2014 and identified 171,432 cases of pediatric cancer during this period (incidence = 173.7 cases per 1 million persons). The cancer types with the highest incidence rates were leukemias (45.7), brain tumors (30.9), and lymphomas (26.2). By U.S. Census region, pediatric cancer incidence was highest in the Northeast (188.0) and lowest in the South (168.0), whereas by state (including the District of Columbia [DC]), rates were highest in New Hampshire, DC, and New Jersey. Among non-Hispanic whites (whites) and non-Hispanic blacks (blacks), pediatric cancer incidence was highest in the Northeast, and the highest rates among Hispanics were in the South. The highest rates of leukemia were in the West, and the highest rates of lymphoma and brain tumors were in the Northeast. State-based differences in pediatric cancer incidence could guide interventions related to accessing care (e.g., in states with large distances to pediatric oncology centers), clinical trial enrollment, and state or regional studies designed to further explore variations in cancer incidence.
USCS includes incidence data from CDC’s National Program of Cancer Registries (NPCR) and the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) program (1). Data on new cases of cancer diagnosed during 2003–2014 were obtained from population-based cancer registries affiliated with NPCR and SEER programs in all U.S. states and DC. This study included incidence data for all registries that met USCS publication criteria* during 2003–2014, which represented >99% of the U.S. population, excluding data only from Nevada, which did not meet criteria in 2011. This report includes all cases of malignant† cancer diagnosed among persons aged <20 years; it includes first primary cases only and excludes recurrent cases. Diagnosis histology and primary site were grouped according to the International Classification of Childhood Cancer (ICCC).§
Pediatric cancer rates were expressed per 1 million persons and were age-adjusted to the 2000 U.S. standard population.¶ Rates were estimated by sex, age group, race/ethnicity, state, U.S. Census region,** county-level economic status, county-level rural/urban classification, and ICCC group.
During 2003–2014, CDC identified 171,432 new cases of pediatric cancer (Table 1). Overall incidence was 173.7 cases per 1 million population. The cancer types with the highest incidence rates were leukemias (45.7 per 1 million), brain tumors (30.9), and lymphomas (26.2). Rates were higher in males (181.5) than in females (165.5) and in persons aged 0–4 years (228.9) and 15–19 years (213.3) than in persons aged 5–9 years (122.6) and 10–14 years (133.0). Among all racial/ethnic groups, the highest incidence rate was among whites (184.4), and the lowest was among blacks (133.3).
Rates were highest in the Northeast U.S. Census region, followed by the Midwest, the West, and the South. Rates were highest in the Northeast across all age groups and among whites and blacks. Among Hispanics, rates were highest in the South. Pediatric cancer incidence rates were highest in the 25% of counties with the highest economic status and were higher in metropolitan areas with populations ≥1 million than in nonmetropolitan areas.
By state, pediatric cancer incidence rates ranged from 145.2–205.5 per 1 million. Rates were highest in New Hampshire (205.5), DC (194.0), and New Jersey (192.3) and lowest in South Carolina (149.3) and Mississippi (145.2) (Table 2). Incidence among whites ranged from 157.0 in Montana to 255.2 in Hawaii; among blacks, from 105.8 in Rhode Island to 161.3 in Nebraska; and among Hispanics, from 75.0 in Hawaii to 191.8 in Florida.†† Although incidence rates were highest among children aged 0–4 years overall, in some states (e.g., New Jersey, New York, and Illinois), the highest rates were among persons aged 15–19 years (Supplementary Table 1, https://stacks.cdc.gov/view/cdc/53585).
Pediatric cancer incidence rates varied by state within each cancer type (Figure). Incidence rates were highest in the West for leukemias, myeloproliferative diseases, and myelodysplastic diseases (ICCC group I) and in the Northeast for lymphomas and reticuloendothelial neoplasms (group II) and central nervous system cancers (group III). Rates were also highest in the Northeast for neuroblastoma, retinoblastoma, bone tumors, soft tissue sarcomas, and thyroid cancer (Supplementary Table 2, https://stacks.cdc.gov/view/cdc/53586). Renal cancer rates were highest in the Northeast and South; hepatic tumor rates were highest in the Northeast and West. Germ cell tumor rates were highest in the West (Supplementary Table 2, https://stacks.cdc.gov/view/cdc/53586).
Discussion
This study used recent data with greater population coverage than past studies (4,5) to document geographic variation in pediatric cancer incidence rates by sex, age, type, and race/ethnicity. Consistent with past reports (1,4,5), pediatric cancer rates were highest in males, persons aged 0–4 years and 15–19 years, whites, and the Northeast U.S. Census region. Rates were highest in metropolitan areas with populations ≥1 million; state-based rates were highest in New Hampshire, DC, and New Jersey.
A strength of this report is the use of extensive population-based surveillance data (>99% coverage§§), which permits a detailed description of state-based cancer incidence variation. Geographic variation in rates might account for differences in results from previous studies that were based on different populations such as state data (2,3), SEER registries (which cover 9%–28% of the U.S. population),¶¶ or other large data sets (6). A 2016 study specific to Delaware assessed pediatric cancer incidence by demographic group and ZIP Code; the study commented on local environmental exposures and possible incidence disparities based upon sex, age, race/ethnicity, geographic location, and economic status (2). USCS data provide states with a standardized way to gauge whether local pediatric cancer incidence rates differ relative to other states and might prompt states to conduct investigations similar to the one performed in Delaware.
Geographic variation in pediatric cancer incidence might be influenced by several factors.*** First, variation in childhood cancer incidence might be related to differences in exposures to carcinogenic chemicals (e.g., air pollution, secondhand smoke, food, or drinking water) or radiation (7). Second, genetic variation in certain populations (e.g., prevalence of cancer predisposition genes) (2,4,5) might contribute to geographic differences in cancer incidence. Third, the rates of certain cancer types might vary by race/ethnicity. For example, Hispanic children have the highest rate of the most common type of leukemia, pediatric acute lymphoblastic leukemia, and states with a higher proportion of Hispanics might have higher rates of acute lymphoblastic leukemia (8). Fourth, incidence of some types of cancer (e.g., thyroid carcinoma) might be related to enhanced detection and access to care, which can vary by geographic location (5,9).
In addition, geographic variation might be affected by age, economic status, or rural/urban classification (4,8,10). Similar to the findings from this report, recent data detailing adult cancers also indicate that the highest cancer incidence rates are in the Northeast (10). Rates of cancer types mostly affecting adults also varied by rural/urban status; some of these differences in adults might be related to factors such as obesity or smoking (10), which might or might not also explain rural/urban variation in pediatric cancer.
The findings in this report are subject to at least three limitations. First, Nevada was excluded because data for 2011 did not meet quality criteria, which limits the representativeness of the findings. Second, differences in diagnosis and cancer reporting among states might contribute to variation in cancer incidence rates (8). For example, states that were early adopters of electronic pathology reporting might report increased rates because of increased case ascertainment compared with other states. Finally, misrepresentation of race and ethnicity might exist; rate numerators might underestimate American Indians, Alaska Natives, and Hispanics, which could artificially lower rates among these groups; and U.S. Census populations used in rate denominators might undercount children and Hispanics, which could artificially increase rates in these populations (8).†††
Knowledge of pediatric cancer incidence variation by state and cancer type can prompt local and state cancer registries to evaluate reporting and diagnostic standards. Understanding geographic variation in incidence rates can help cancer control planners and clinicians address obstacles in access to care, which is especially relevant to states with large distances to pediatric oncology centers (3). Because 5-year pediatric cancer survival is >80%, and most cancer survivors require close monitoring by specialists throughout life (5), state-specific data by cancer type and patient age might help public health planners address ongoing chronic care needs. In addition, state-specific data by cancer type and patient age might help clinical trial organizers predict patient accrual. Finally, health care practitioners and researchers can use these data to guide investigations related to causes of pediatric cancer incidence variation (2,3). Continued surveillance will be needed to further validate findings and track geographic incidence patterns over time.
Conflict of Interest
No conflicts of interest were reported.
Corresponding author: David A. Siegel, dsiegel@cdc.gov, 770-488-4426.
1Epidemic Intelligence Service, CDC; 2Division of Cancer Prevention and Control, National Center for Chronic Disease Prevention and Health Promotion, CDC.
* Cancer registries’ incidence data met the following five USCS criteria: 1) ≤5% of cases ascertained solely on the basis of death certificate; 2) ≤3% of cases missing information on sex; 3) ≤3% of cases missing information on age; 4) ≤5% of cases missing information on race; and 5) ≥97% of registry’s records passed a set of single-field and interfield computerized edits that test the validity and logic of data components. https://nccd.cdc.gov/uscs/.
† Used behavior code = 3. https://seer.cancer.gov/behavrecode/.
§ https://seer.cancer.gov/iccc/iccc-who2008.html and https://onlinelibrary.wiley.com/doi/full/10.1002/cncr.20910. The ICCC applies the rules and nomenclature of the International Classification of Diseases for Oncology, Third Edition: http://codes.iarc.fr/.
¶ Population estimates incorporate bridged single-race estimates derived from the original multiple race categories in the 2010 U.S. Census. https://seer.cancer.gov/popdata.
** https://www.census.gov/geo/reference/gtc/gtc_census_divreg.html.
†† State-specific rate ranges by race/ethnicity do not include data suppressed for states that elected to be excluded from race/ethnicity analysis.
§§ https://www.cdc.gov/cancer/npcr/uscs/pdf/uscs-2014-technical-notes.pdf.
¶¶ https://seer.cancer.gov/registries/data.html.
*** https://www.cdc.gov/cancer/npcr/uscs/data/00_guidance_include.htm.
††† https://www.cdc.gov/cancer/npcr/uscs/technical_notes/interpreting/race.htm.
References
- US Cancer Statistics Working Group. United States cancer statistics: 1999–2014 incidence and mortality web-based report. Atlanta, GA: US Department of Health and Human Services, CDC; National Cancer Institute; 2017. https://www.cdc.gov/cancer/npcr/uscs/index.htm
- Holmes L, Vandenberg J, McClarin L, Dabney K. Epidemiologic, racial and healthographic mapping of Delaware pediatric cancer: 2004–2014. Int J Environ Res Public Health 2015;13(1),49. http://www.mdpi.com/1660-4601/13/1/49 PubMed
- Farazi PA, Watanabe-Galloway S, Westman L, et al. Temporal and geospatial trends of pediatric cancer incidence in Nebraska over a 24-year period. Cancer Epidemiol 2018;52:83–90. CrossRef PubMed
- Li J, Thompson TD, Miller JW, Pollack LA, Stewart SL. Cancer incidence among children and adolescents in the United States, 2001–2003. Pediatrics 2008;121:e1470–7. CrossRef PubMed
- Ward E, DeSantis C, Robbins A, Kohler B, Jemal A. Childhood and adolescent cancer statistics, 2014. CA Cancer J Clin 2014;64:83–103. CrossRef PubMed
- Musselman JR, Spector LG, Krailo MD, et al. The Children’s Oncology Group Childhood Cancer Research Network (CCRN): case catchment in the United States. Cancer 2014;120:3007–15. CrossRef PubMed
- Carpenter DO, Bushkin-Bedient S. Exposure to chemicals and radiation during childhood and risk for cancer later in life. J Adolesc Health 2013;52(Suppl):S21–9. CrossRef PubMed
- Siegel DA, Henley SJ, Li J, Pollack LA, Van Dyne EA, White A. Rates and trends of pediatric acute lymphoblastic leukemia—United States, 2001–2014. MMWR Morb Mortal Wkly Rep 2017;66:950–4. CrossRef PubMed
- Li N, Du XL, Reitzel LR, Xu L, Sturgis EM. Impact of enhanced detection on the increase in thyroid cancer incidence in the United States: review of incidence trends by socioeconomic status within the Surveillance, Epidemiology, and End Results Registry, 1980–2008. Thyroid 2013;23:103–10. CrossRef PubMed
- Zahnd WE, James AS, Jenkins WD, et al. Rural-urban differences in cancer incidence and trends in the United States. Cancer Epidemiol Biomarkers Prev 2017. CrossRef PubMed
Sources: CDC’s National Program of Cancer Registries; National Cancer Institute’s Surveillance, Epidemiology, and End Results Program.
Abbreviations: AI/AN = American Indian/Alaska Native; API = Asian/Pacific Islander; CI = confidence interval.
* Rates are per 1 million persons and age-adjusted to the 2000 U.S. standard population.
† Cases included all malignant cancers (with behavior code = 3) as grouped by the International Classification of Childhood Cancer.
§ Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont. Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin. South: Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia. West: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming.
¶ Incidence data are compiled from cancer registries that meet the data quality criteria for all years 2003–2014 (covering >99% of the U.S. population). Nevada is excluded. Registry-specific data quality information is available at https://www.cdc.gov/cancer/npcr/uscs/pdf/uscs-2014-technical-notes.pdf. Characteristic values with other, missing, or blank results are not included in this table.
** White, black, AI/AN, and API persons are non-Hispanic. Hispanic persons might be of any race. Counts exclude unspecified or unknown race/ethnicity.
†† Excludes Kansas, Minnesota, and Nevada.
Sources: CDC’s National Program of Cancer Registries; National Cancer Institute’s Surveillance, Epidemiology, and End Results Program.
Abbreviations: AI/AN = American Indian/Alaska Native; API = Asian/Pacific Islander; CI = confidence interval.
* Rates are per 1 million persons and age-adjusted to the 2000 U.S. standard population.
† Cases included all malignant cancers (with behavior code = 3) as grouped by the International Classification of Childhood Cancer.
§ Incidence data are compiled from cancer registries that meet the data quality criteria for all years 2003–2014 (covering >99% of the U.S. population). Nevada is excluded. Registry-specific data quality information is available at https://www.cdc.gov/cancer/npcr/uscs/pdf/uscs-2014-technical-notes.pdf.
¶ White, black, AI/AN, and API are non-Hispanic. Hispanic persons might be of any race. Counts exclude unspecified or unknown race/ethnicity; the counts in the total column may not equal the sum of the individual race/ethnicity columns.
** States are grouped by U.S. Census region.
†† Case counts <16 are suppressed.
§§ Race/ethnicity data was suppressed for states that elected to be excluded from race/ethnicity analysis.
 FIGURE. Age-adjusted incidence* of cancer† among persons aged <20 years, by U.S. state and ICCC type§ — United States, 2003–2014¶
FIGURE. Age-adjusted incidence* of cancer† among persons aged <20 years, by U.S. state and ICCC type§ — United States, 2003–2014¶
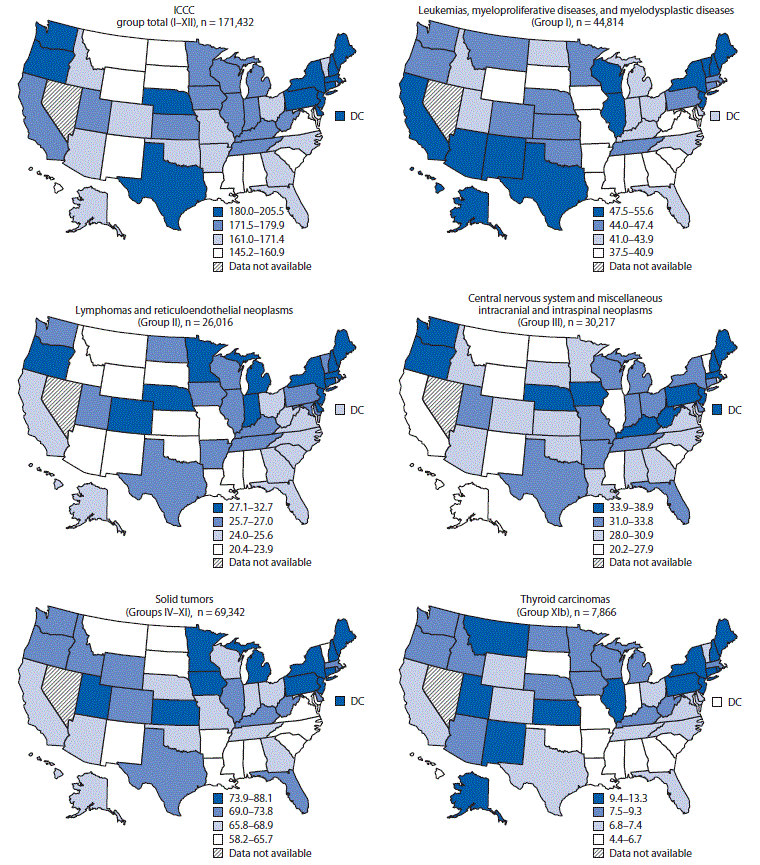
Sources: CDC’s National Program of Cancer Registries; National Cancer Institute’s Surveillance, Epidemiology, and End Results Program.
Abbreviation: ICCC = International Classification of Childhood Cancer.
* Rates are per 1 million persons and age-adjusted to the 2000 U.S. standard population.
† Cases included all malignant cancers (with behavior code = 3) as grouped by the ICCC.
§ Solid tumors (Groups IV–XI) include neuroblastoma and other peripheral nervous cell tumors, retinoblastoma, renal tumors, hepatic tumors, malignant bone tumors, soft tissue and other extraosseous sarcomas, germ cell and trophoblastic tumors and neoplasms of gonads, and other malignant epithelial neoplasms and melanomas. The ICCC group total map includes 258 cases not classified by ICCC.
¶ Incidence data are compiled from cancer registries that meet the data quality criteria for all years 2003–2014 (covering >99% of the U.S. population). Nevada is excluded. Registry-specific data quality information is available at https://www.cdc.gov/cancer/npcr/uscs/pdf/uscs-2014-technical-notes.pdf.
The figure above is a series of maps showing age-adjusted incidence rate of cancer among persons aged <20 years, by U.S. state and International Classification of Childhood Cancer type in the United States, during 2003–2014.
Suggested citation for this article: Siegel DA, Li J, Henley SJ, et al. Geographic Variation in Pediatric Cancer Incidence — United States, 2003–2014. MMWR Morb Mortal Wkly Rep 2018;67:707–713. DOI: http://dx.doi.org/10.15585/mmwr.mm6725a2.
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (https://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.