Diagnoses of HIV Infection in the United States and Dependent Areas, 2018: Figures
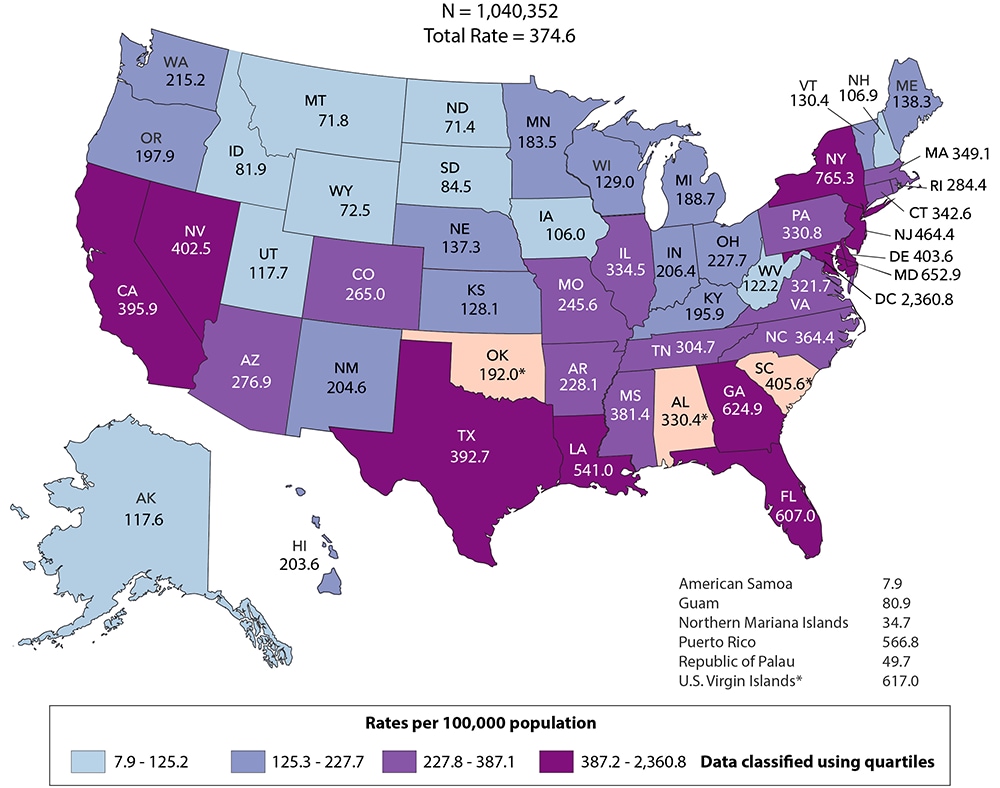
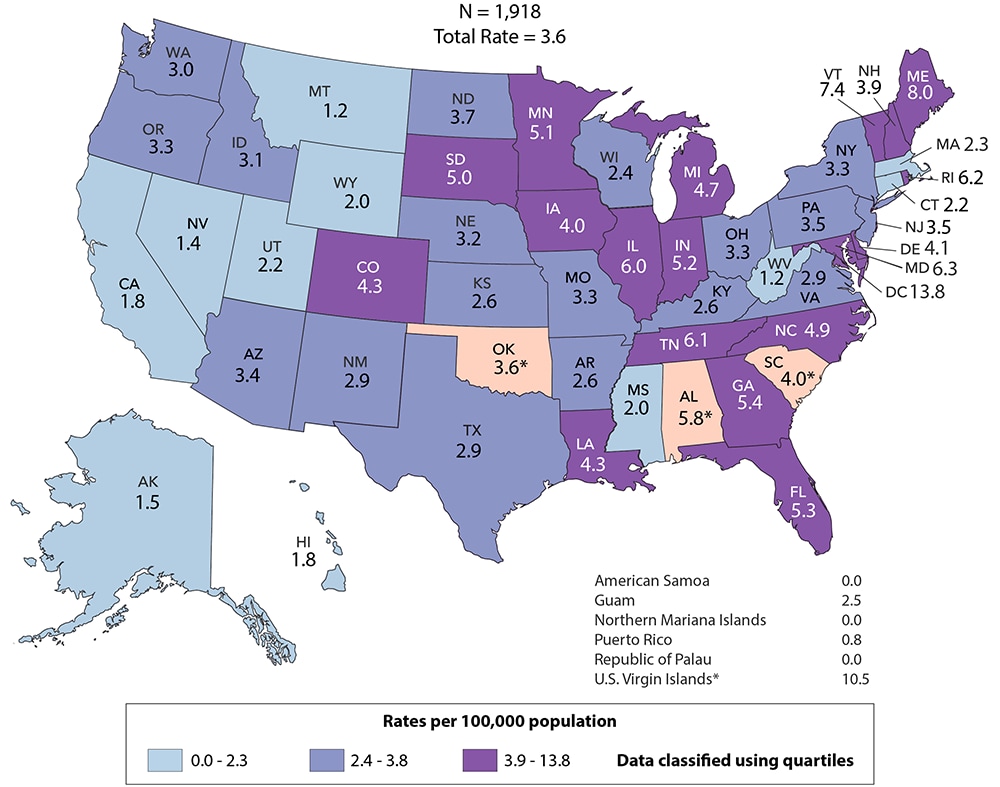
Figure 1. Rates of Diagnoses of HIV Infection among Adults and Adolescents, 2018—United States and 6 Dependent Areas
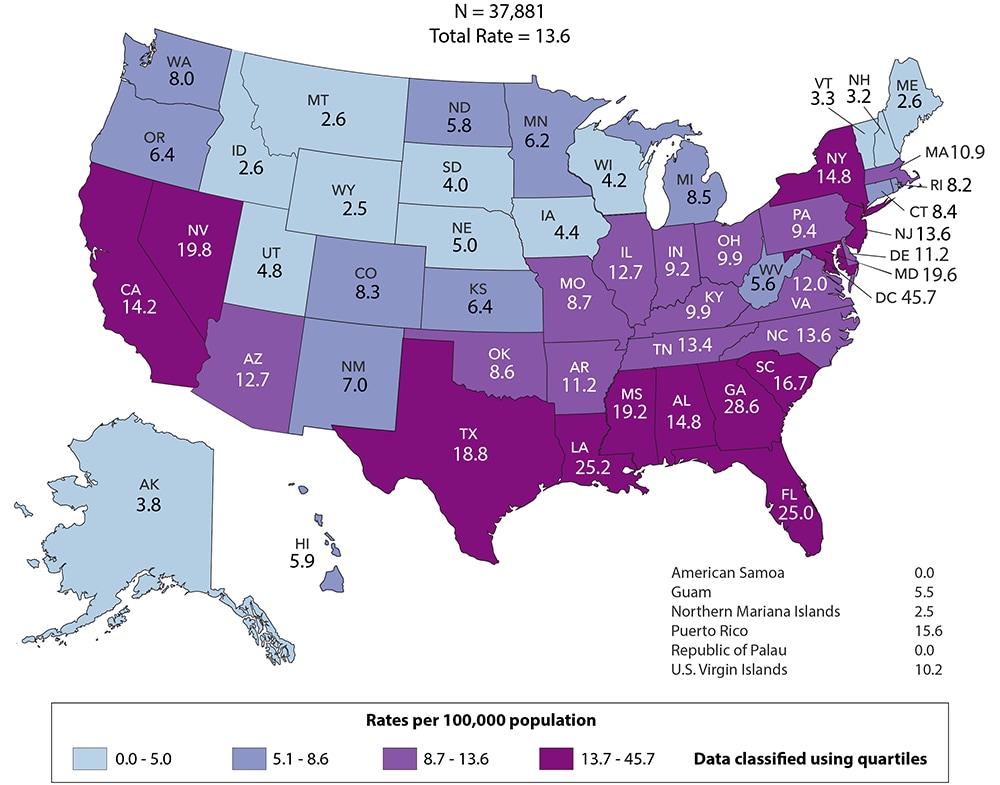
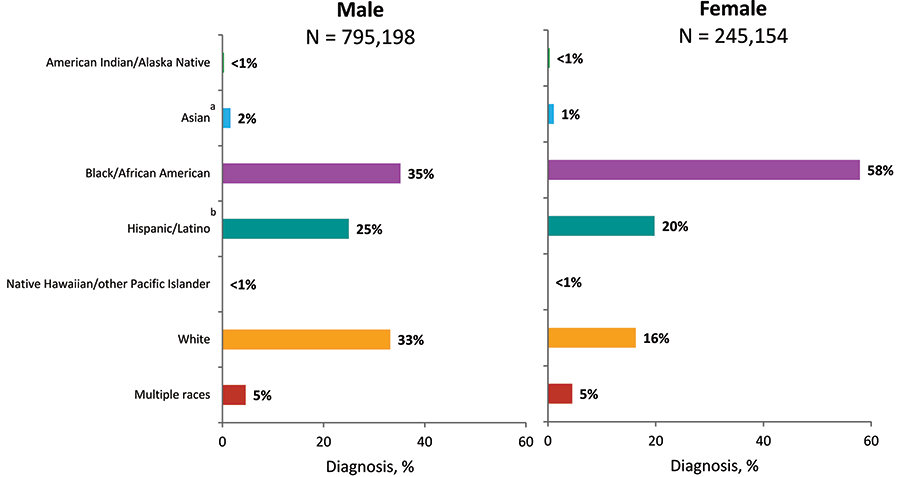
Figure 2. Diagnoses of HIV Infection among Adults and Adolescents, by Gender, 2014–2018—United States and 6 Dependent Areas
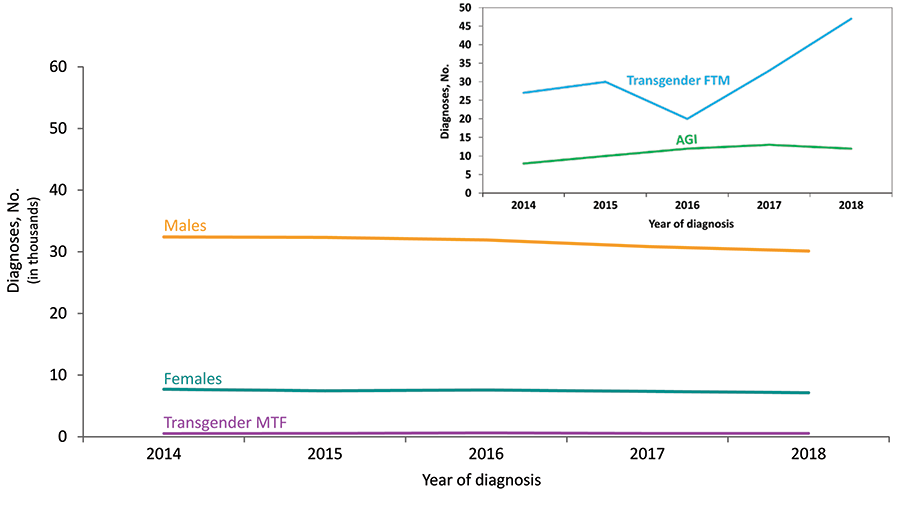
Note: See Data Tables, Definitions, and Acronyms for more information on gender.
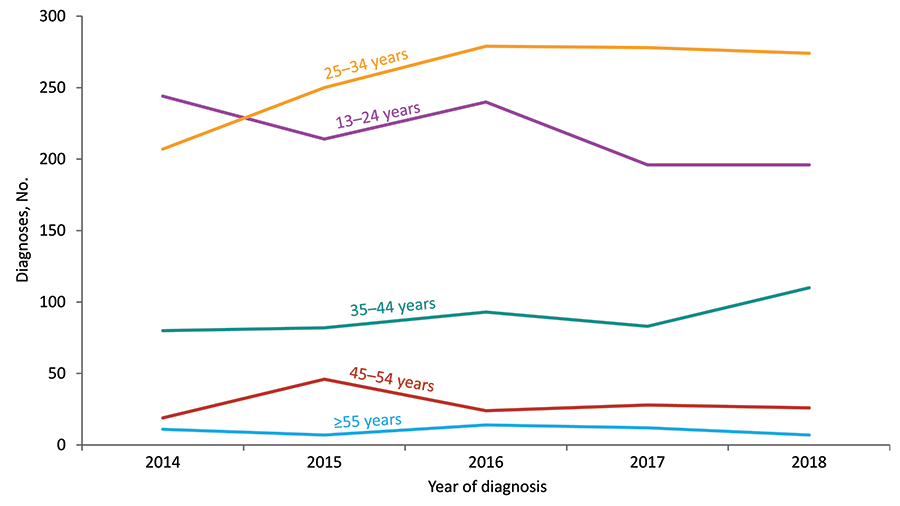
Figure 3. Rates of Diagnoses of HIV Infection among Adults and Adolescents, by Age at Diagnosis, 2014–2018—United States
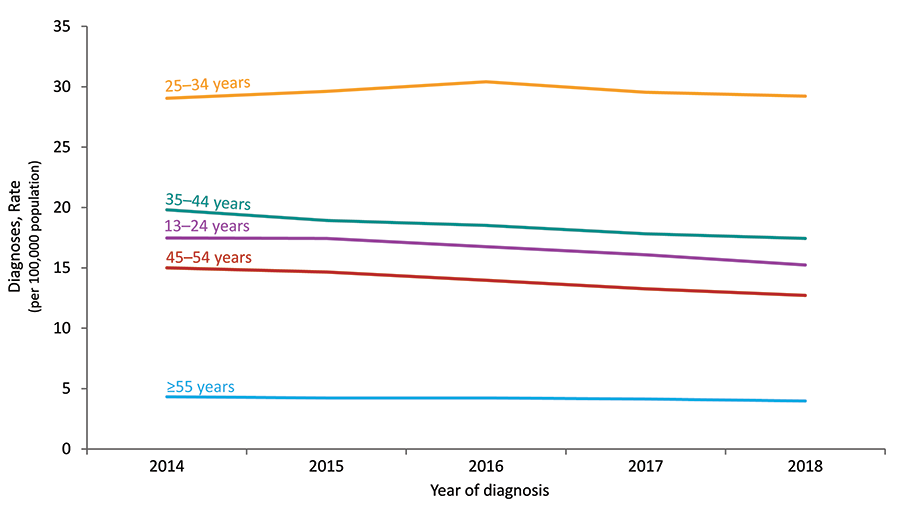
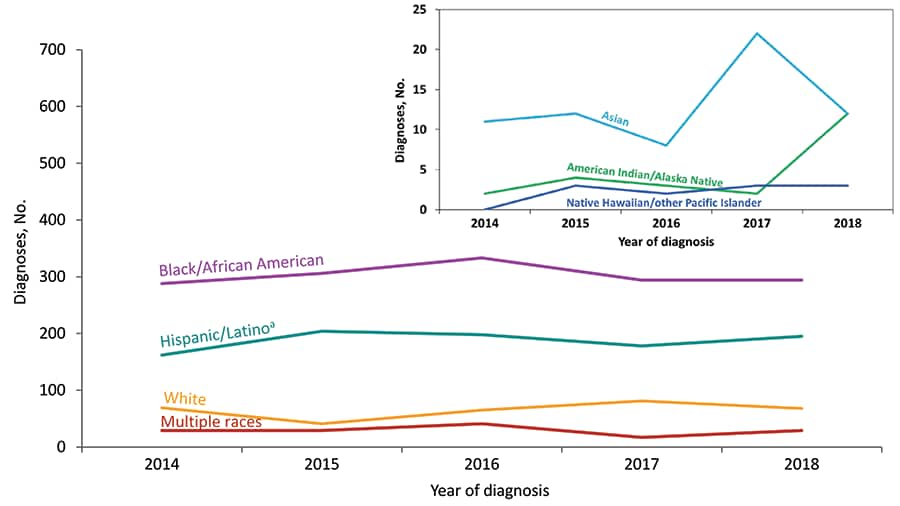
Figure 4. Rates of Diagnoses of HIV Infection among Adults and Adolescents, by Race/Ethnicity, 2014–2018—United States
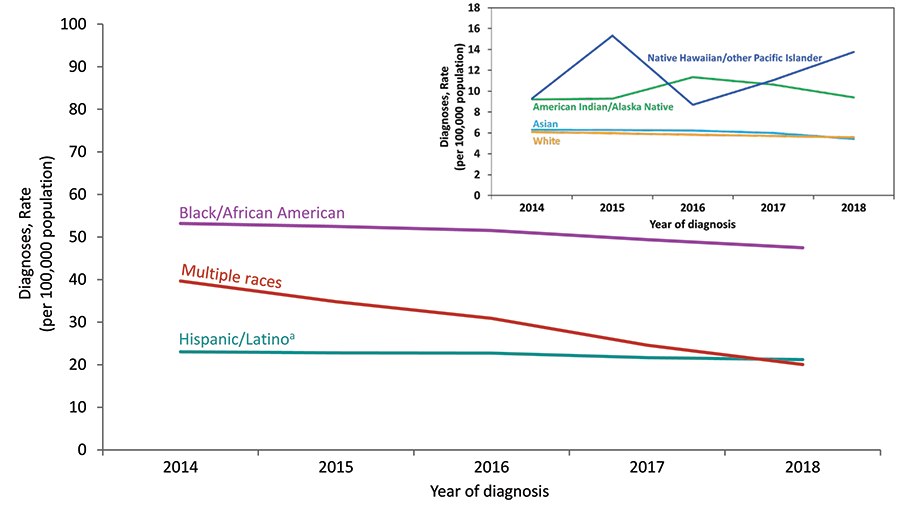
Note: See Data Tables, Definitions, and Acronyms for more information on race/ethnicity.
a Hispanics/Latinos can be of any race.
Figure 5. Percentages of Diagnoses of HIV Infection among Adults and Adolescents, by Transmission Category, 2014–2018—United States and 6 Dependent Areas
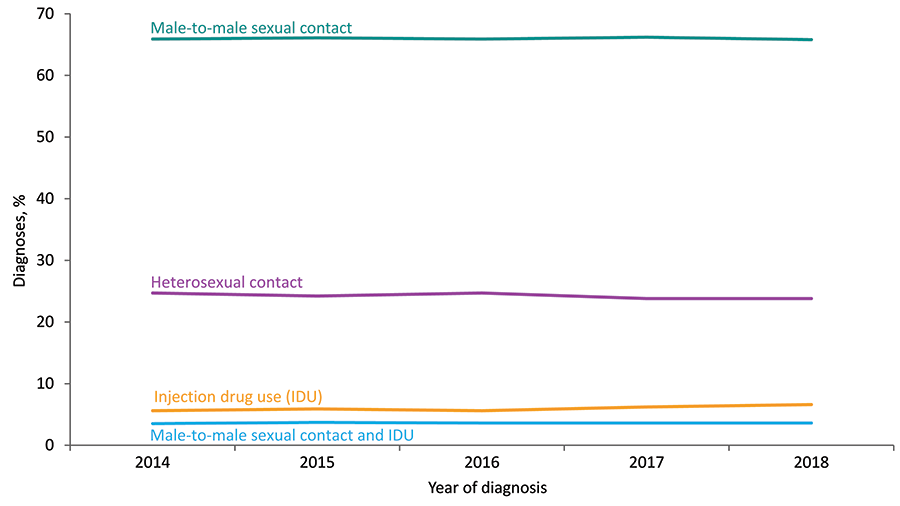
Note: Data have been statistically adjusted to account for missing transmission category. See Data Tables, Definitions, and Acronyms for more information on transmission categories.
Figure 6. Percentages of Diagnoses of HIV Infection among Adults and Adolescents, by Transmission Category, 2018—United States and 6 Dependent Areas
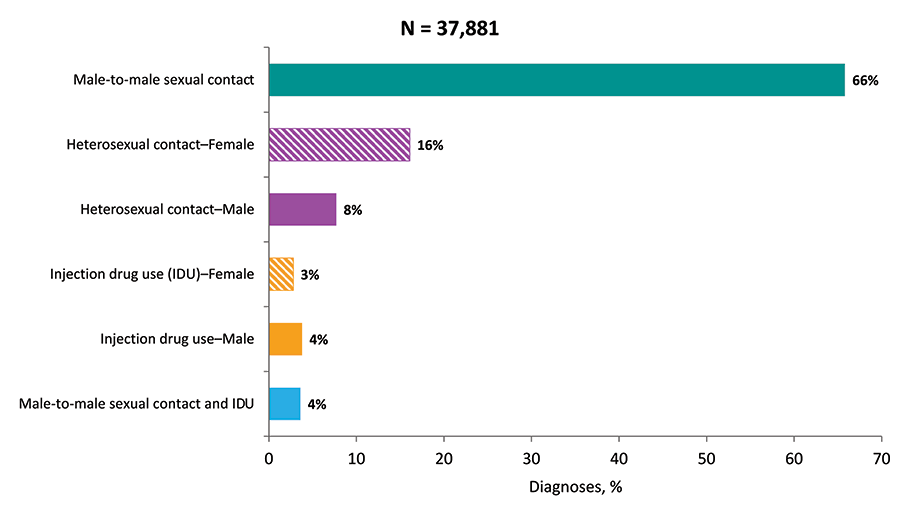
Note: Data have been statistically adjusted to account for missing transmission category. Total N includes perinatal and other transmissions among adults and adolescents. See Data Tables, Definitions, and Acronyms for more information on transmission categories.
Figure 7. Rates of Deaths of Adults and Adolescents with Diagnosed HIV Infection, 2018—United States and 6 Dependent Areas
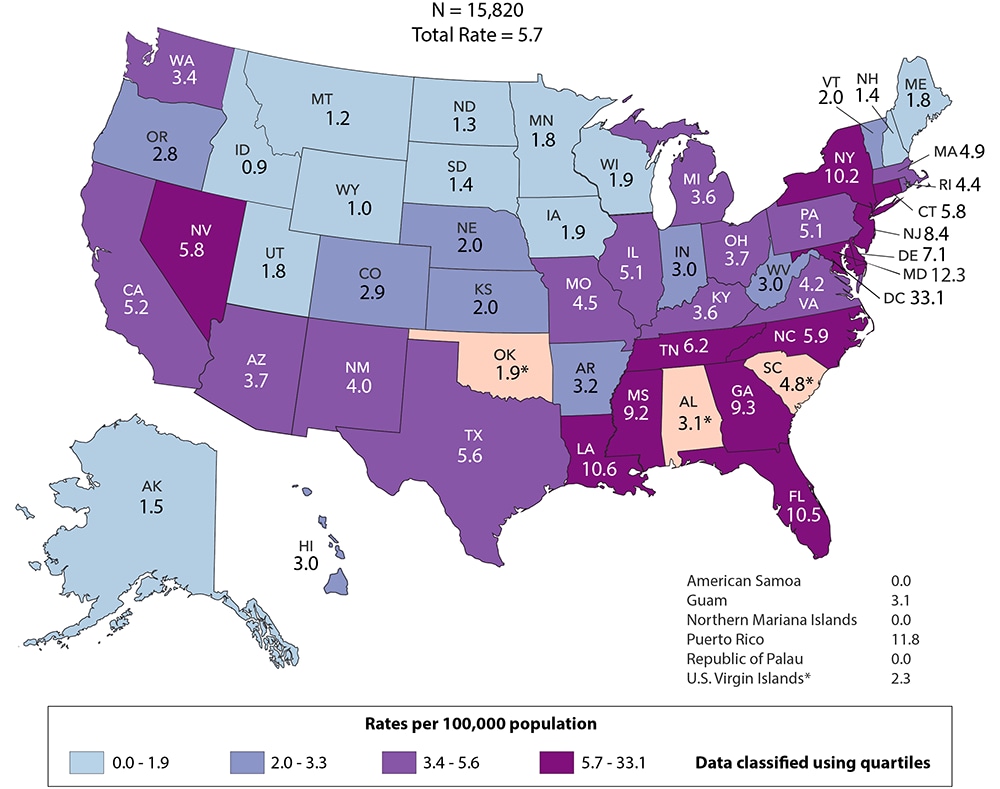
Note: Data for the year 2018 are preliminary and based on deaths reported to CDC as of December 2019. Data are based on address of residence at death. Asterisk (*) indicates incomplete reporting. See Data Tables, Definitions, and Acronyms for more information on deaths.
Figure 8. Rates of Deaths for Persons with Diagnosed HIV Infection, by Race/Ethnicity, 2014–2018—United States
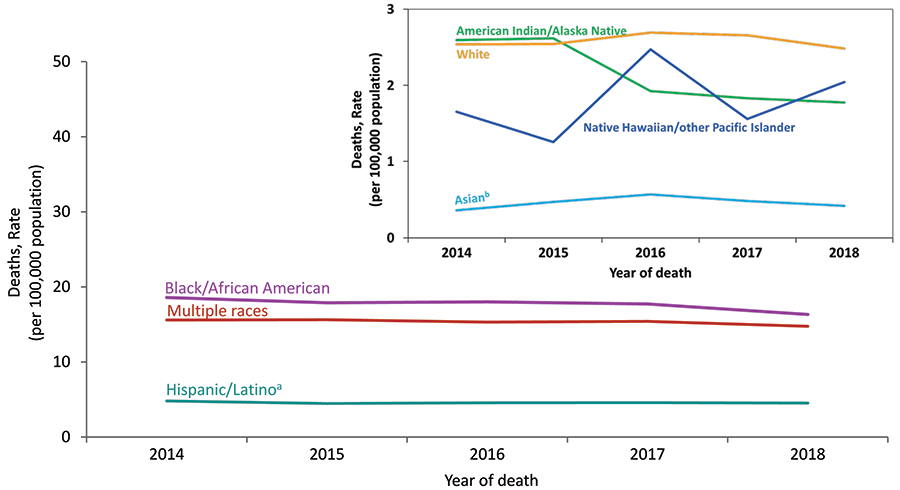
Note: Data for the year 2018 are preliminary and based on deaths reported to CDC as of December 2019. See Data Tables, Definitions, and Acronyms for more information on deaths and race/ethnicity.
a Hispanics/Latinos can be of any race.
b Includes Asian/Pacific Islander legacy cases.
Figure 9. Rates of Adults and Adolescents Living with Diagnosed HIV Infection, Year-end 2018—United States and 6 Dependent Areas
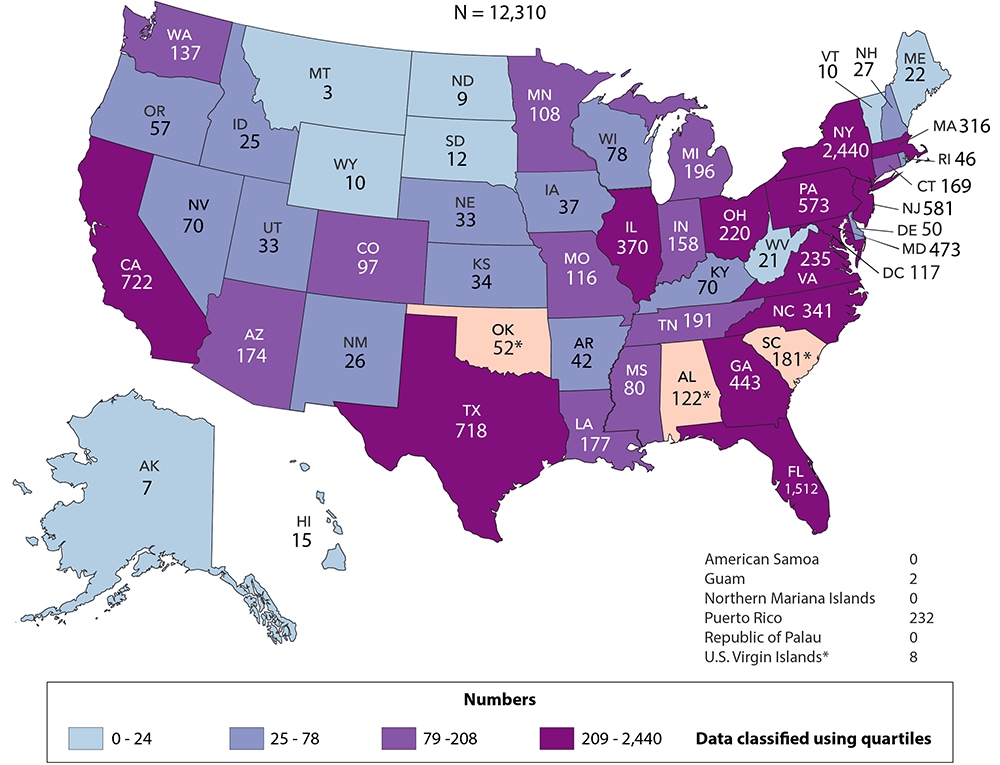
Note: Data for the year 2018 are preliminary and based on deaths reported to CDC as of December 2019. Data are based on address of residence as of December 31, 2018 (i.e., most recent known address). Asterisk (*) indicates incomplete reporting. See Data Tables, Definitions, and Acronyms for more information on prevalence.
Figure 10. Adults and Adolescents Living with Diagnosed HIV Infection, by Sex at Birth and Race/Ethnicity, Year-end 2018—United States and 6 Dependent Areas
Note: Data for the year 2018 are preliminary and based on deaths reported to CDC as of December 2019. See Data Tables, Definitions, and Acronyms for more information on prevalence and race/ethnicity.
a Includes Asian/Pacific Islander legacy cases.
b Hispanics/Latinos can be of any race.
Figure 11. Diagnoses of HIV Infection among Transgender Adults and Adolescents, by Age at Diagnosis, 2014–2018—United States and 6 Dependent Areas
Note: See Data Tables, Definitions, and Acronyms for more information on gender.
Figure 12. Diagnoses of HIV Infection among Transgender Adults and Adolescents, by Race/Ethnicity, 2014–2018—United States and 6 Dependent Areas
Note: See Data Tables, Definitions, and Acronyms for more information on race/ethnicity.
a Hispanics/Latinos can be of any race.
Figure 13. Percentages of Diagnoses of HIV Infection among Transgender Adults and Adolescents, by Gender and Race/Ethnicity, 2018—United States and 6 Dependent Areas
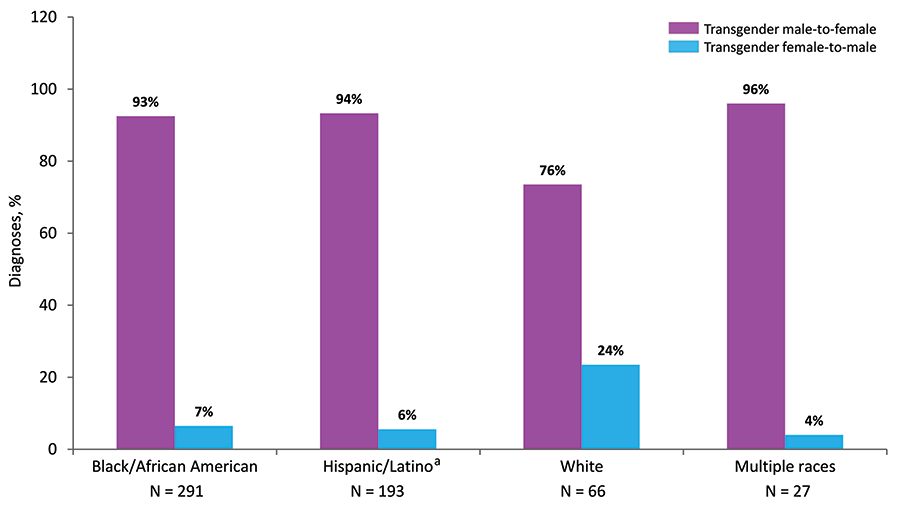
Note: See Data Tables, Definitions, and Acronyms for more information on gender and race/ethnicity.
a Hispanics/Latinos can be of any race.
Figure 14. Diagnoses of HIV Infection among Men Who Have Sex with Men, by Age at Diagnosis, 2014–2018—United States and 6 Dependent Areas
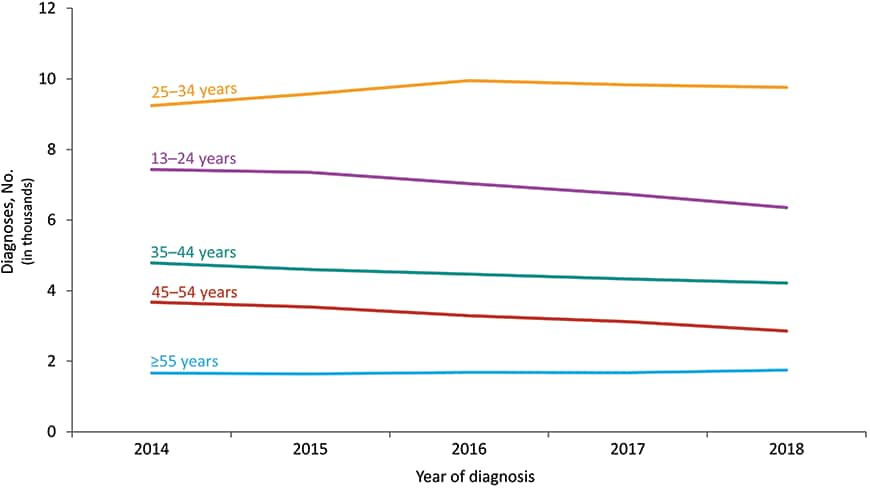
Note: Data have been statistically adjusted to account for missing transmission category. See Data Tables, Definitions, and Acronyms for more information on transmission categories.
Figure 15. Percentages of Diagnoses of HIV Infection among Men Who Have Sex with Men, by Race/Ethnicity, 2014–2018—United States and 6 Dependent Areas
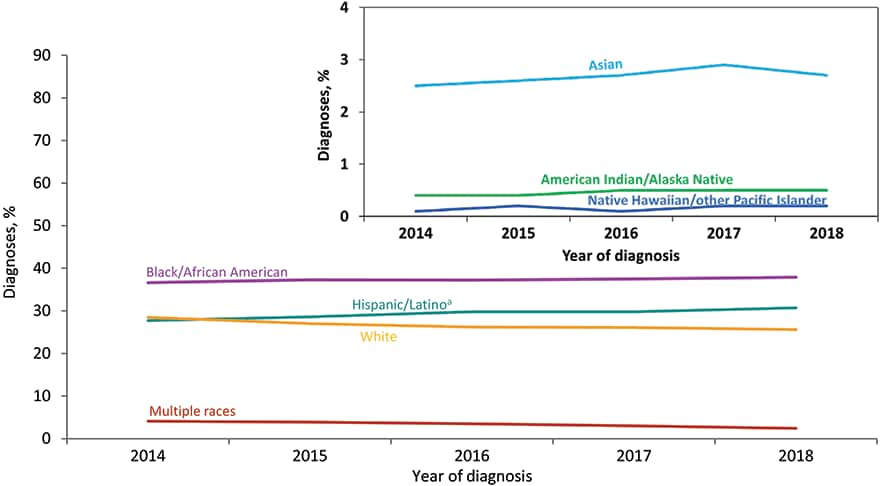
Note: Data have been statistically adjusted to account for missing transmission category. See Data Tables, Definitions, and Acronyms for more information on race/ethnicity and transmission categories.
a Hispanics/Latinos can be of any race.
Figure 16. Diagnoses of HIV Infection among Men Who Have Sex with Men, by Age Group and Race/Ethnicity, 2018—United States and 6 Dependent Areas
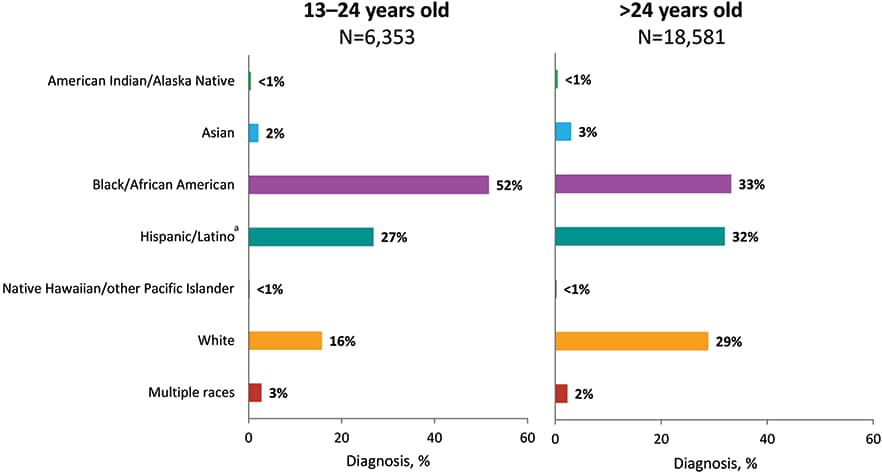
Note: Data have been statistically adjusted to account for missing transmission category. See Data Tables, Definitions, and Acronyms for more information on race/ethnicity and transmission categories.
a Hispanics/Latinos can be of any race.
Figure 17. Diagnoses of HIV Infection among Men Who Have Sex with Men, by Region of Residence and Race/Ethnicity, 2018—United States and 6 Dependent Areas
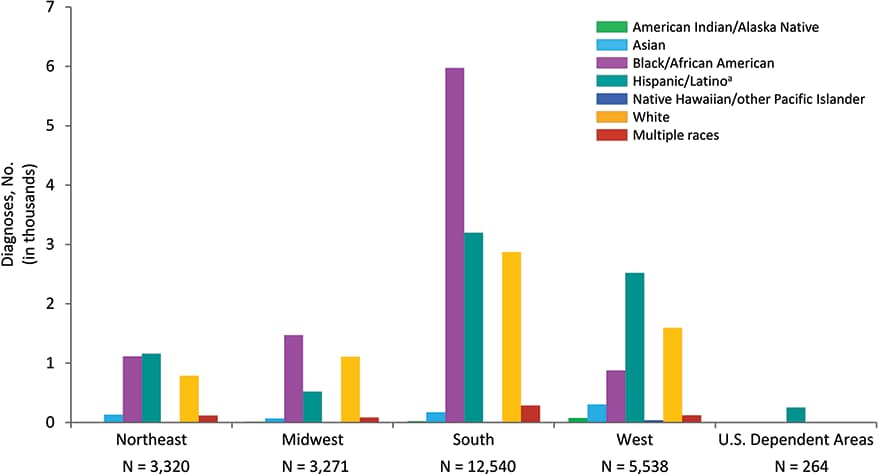
Note: Data have been statistically adjusted to account for missing transmission category. See Data Tables, Definitions, and Acronyms for more information on interpreting numbers, race/ethnicity, transmission categories, and U.S. Census Regions.
a Hispanics/Latinos can be of any race.
Figure 18. Diagnoses of HIV Infection among Persons Who Inject Drugs, by Sex at Birth and Race/Ethnicity, 2018—United States and 6 Dependent Areas
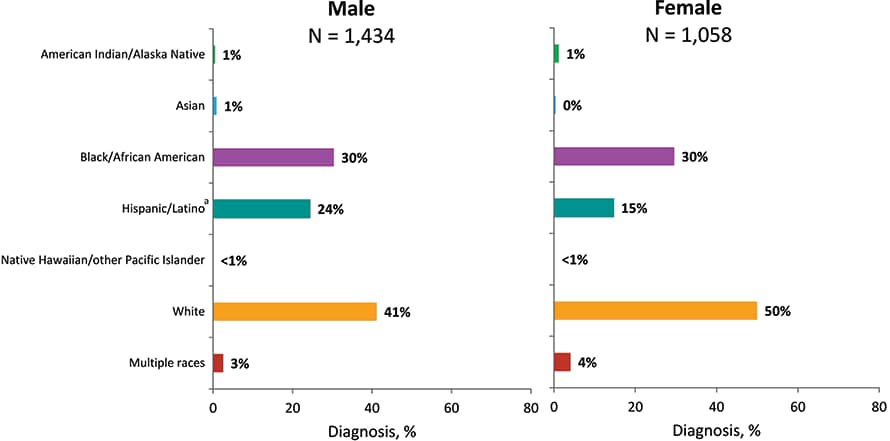
Note: Data have been statistically adjusted to account for missing transmission category. See Data Tables, Definitions, and Acronyms for more information on race/ethnicity and transmission categories.
a Hispanics/Latinos can be of any race.
Figure 19. Diagnoses of HIV Infection among Persons Who Inject Drugs, by Region and Race/Ethnicity, 2018—United States and 6 Dependent Areas
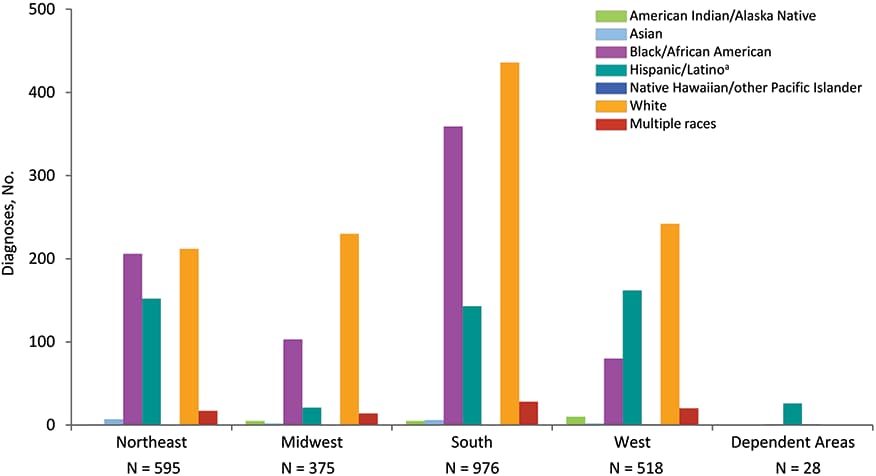
Note: Data have been statistically adjusted to account for missing transmission category. See Data Tables, Definitions, and Acronyms for more information on race/ethnicity, transmission categories, and U.S. Census Regions.
a Hispanics/Latinos can be of any race.
Figure 20. Rates of Diagnoses of HIV Infection among Female Adults and Adolescents, 2018—United States and 6 Dependent Areas

Figure 21. Percentages of Diagnoses of HIV Infection and Population among Female Adults and Adolescents, by Race/Ethnicity, 2018—United States
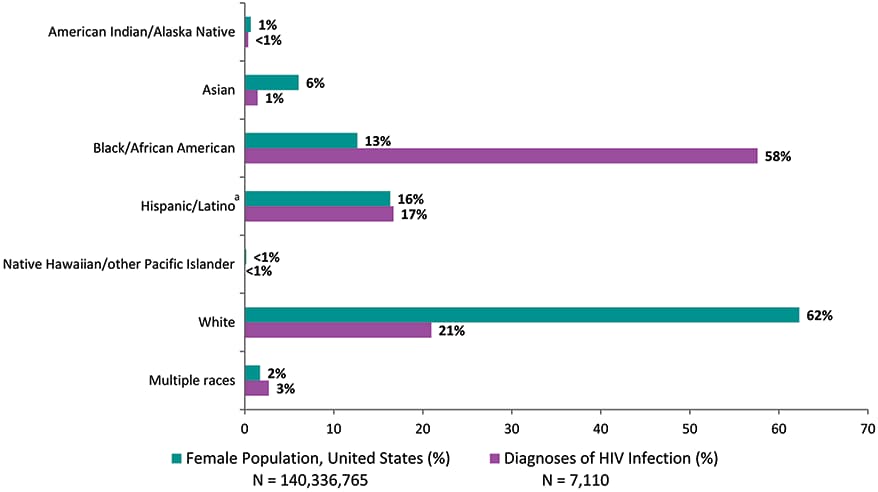
Note: See Data Tables, Definitions, and Acronyms for more information on race/ethnicity.
a Hispanics/Latinos can be of any race.
Figure 22. Diagnoses of HIV Infection among Female Adults and Adolescents, by Race/Ethnicity, 2014–2018—United States and 6 Dependent Areas
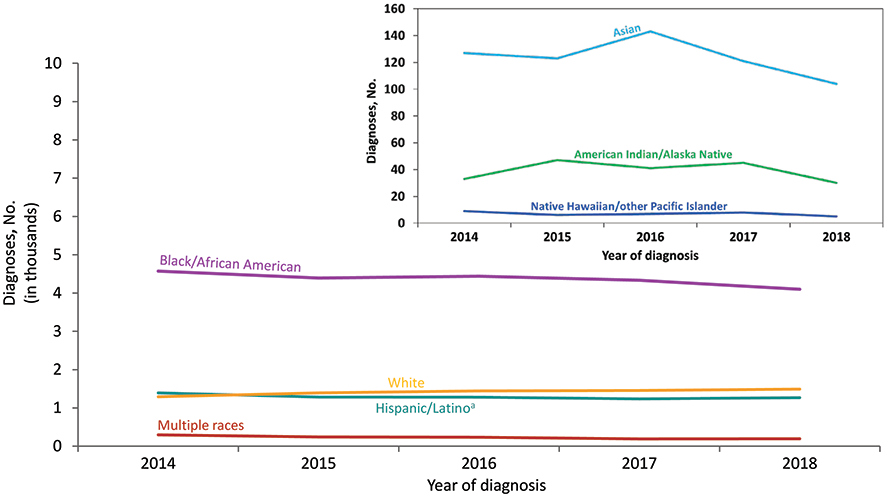
Note: See Data Tables, Definitions, and Acronyms for more information on race/ethnicity.
a Hispanics/Latinos can be of any race.
Figure 23. Percentages of Diagnoses of HIV Infection among Female Adults and Adolescents, by Race/Ethnicity and Transmission Category, 2018—United States and 6 Dependent Areas
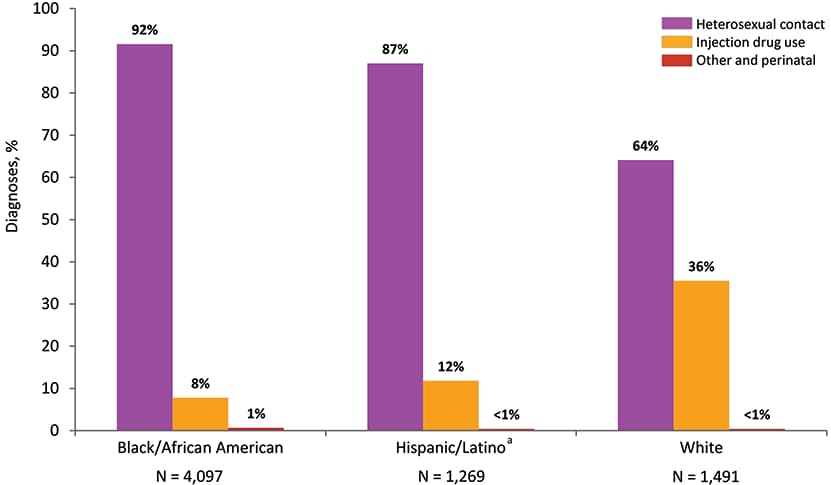
Note. Data have been statistically adjusted to account for missing transmission category. See Data Tables, Definitions, and Acronyms for more information on race/ethnicity and transmission categories.
a Hispanics/Latinos can be of any race.
Figure 24. Rates of Diagnoses of HIV Infection among Female Adults and Adolescents, by Region and Race/Ethnicity, 2018—United States
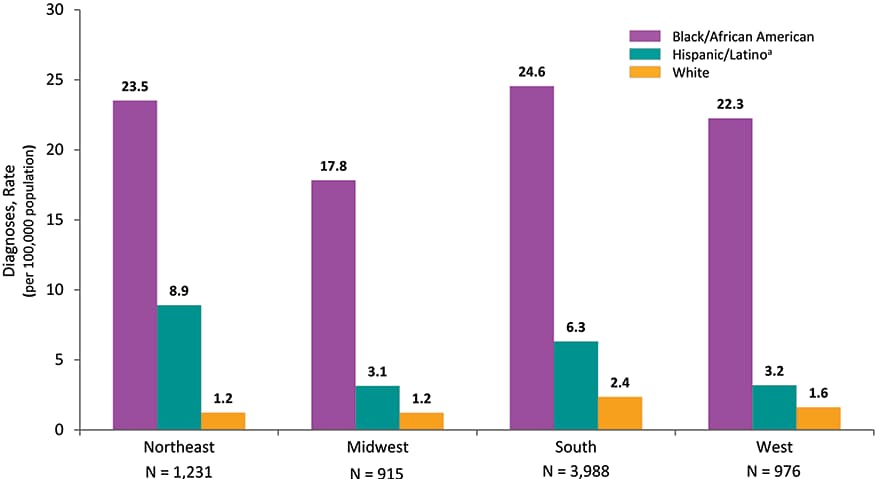
Note: See Data Tables, Definitions, and Acronyms for more information on race/ethnicity and U.S. Census Regions.
a Hispanics/Latinos can be of any race.
Figure 25. Diagnoses of Perinatally Acquired HIV Infection among Children Born During 2017, by Area of Residence—United States and Puerto Rico
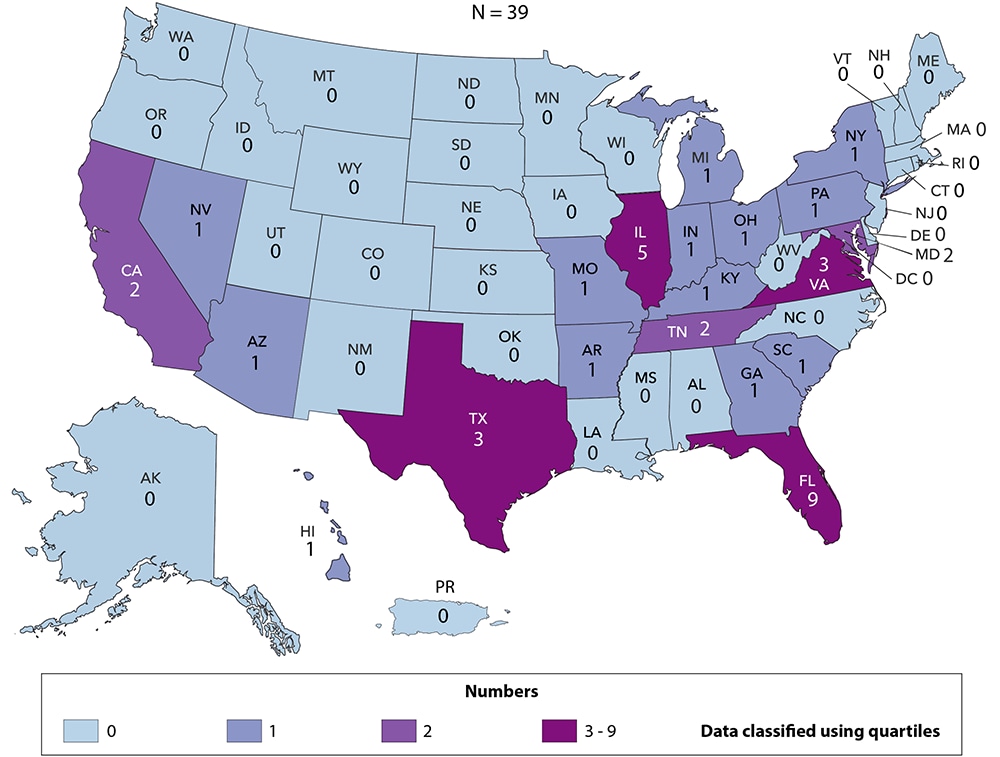
Figure 26. Diagnoses of HIV Infection among Children Aged <13 Years, by Age at Diagnosis, 2014–2018—United States and 6 Dependent Areas
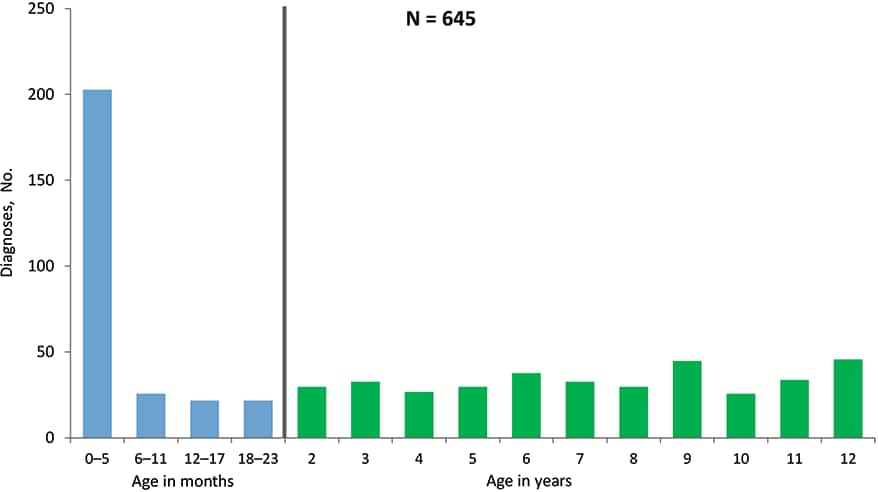
Figure 27. Time of Maternal HIV Testing among Children with Diagnosed Perinatally Acquired HIV Infection and Children Exposed to HIV, Birth Years 2014–2017—United States and Puerto Rico
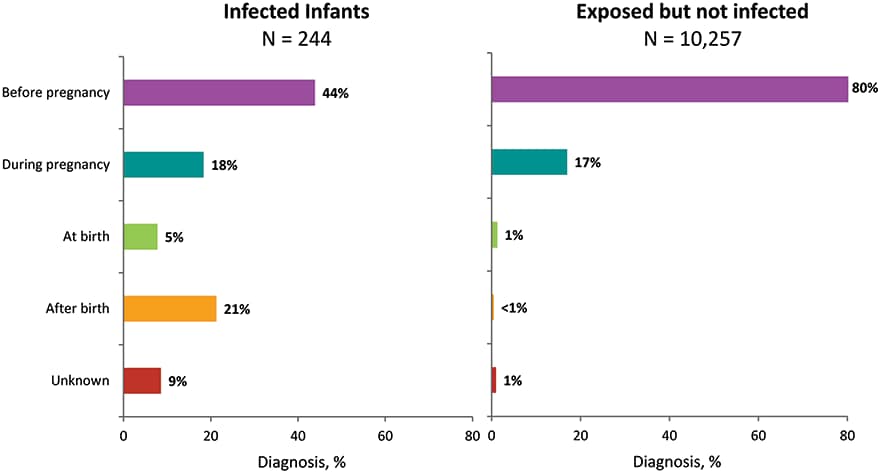
Figure 28. Percentages of Diagnoses of HIV Infection among Children Aged <13 Years, by Race/Ethnicity, 2014—2018—United States and 6 Dependent Areas
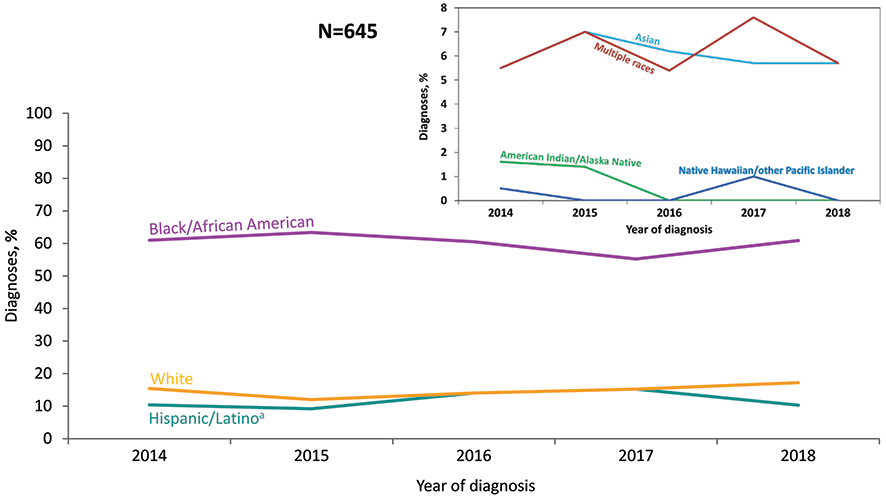
Note: See Data Tables, Definitions, and Acronyms for more information on race/ethnicity.
a Hispanics/Latinos can be of any race.
Figure 29. Percentages of Diagnoses of HIV Infection and Population in Children Aged <13 Years, by Race/Ethnicity, 2018—United States
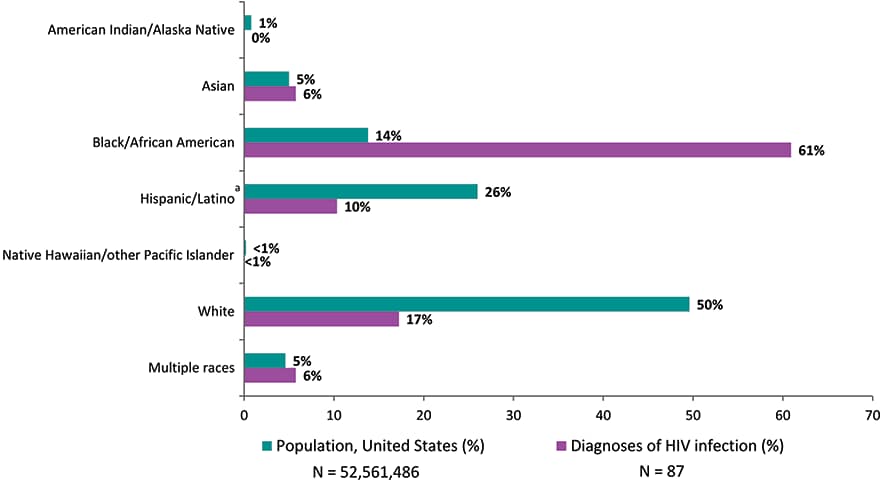
Note: See Data Tables, Definitions, and Acronyms for more information on race/ethnicity.
aHispanics/Latinos can be of any race.
Figure 30. Rates of Children Aged <13 Years Living with Diagnosed HIV Infection, Year-end 2018—United States and 6 Dependent Areas
Note: Data for the year 2018 are preliminary and based on deaths reported to CDC as of December 2019. Data are based on address of residence as of December 31, 2018 (i.e., most recent known address). Asterisk (*) indicates incomplete reporting. See Data Tables, Definitions, and Acronyms for more information on prevalence.
Figure 31. Persons Living with Diagnosed Perinatally Acquired HIV Infection, Year-end 2018—United States and 6 Dependent Areas
Note: Data for the year 2018 are preliminary and based on deaths reported to CDC as of December 2019. Data are based on address of residence as of December 31, 2018 (i.e., most recent known address). Asterisk (*) indicates incomplete reporting. See Data Tables, Definitions, and Acronyms for more information on prevalence.
The data in this report include information received by CDC through December 31, 2019. The data are organized into 2 sections: National Profile and Special Focus Profiles. For both the National and Special Focus Profiles, figures are presented. For the National Profile, tables are presented in the Tables section in 2 formats. Tables in the first format—labeled “a”—exclude data from the dependent areas (American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, the Republic of Palau, and the U.S. Virgin Islands). Tables in the second format—labeled “b”—include data from the dependent areas.
Please use caution when interpreting numbers less than 12, and rates and trends based on these numbers.
Persons reported to the National HIV Surveillance System are assumed alive unless their deaths have been reported to CDC. Death data include deaths of persons with diagnosed HIV infection (Figures 7 and 8; Tables 10a/b–13a/b) regardless of the cause of death. Death data are based on a 12-month reporting delay to allow data to be reported to CDC. For the death tables, region or area of residence is based on residence at death. When information on residence at death is not available, the state where a person’s death occurred is used. Data for the year 2018 are preliminary and based on death data received by CDC through December 2019. Trends through 2018 should be interpreted with caution. Due to incomplete reporting of deaths for the year 2018, death data for Alabama, Oklahoma, South Carolina, and the U.S. Virgin Islands should be interpreted with caution.
Prevalence trends and data reflect persons living with diagnosed HIV infection, regardless of stage of disease, (Figures 9, 10, 30, and 31; Tables 14a/b–17a/b, 19, 20, and A2) at the end of a given year during 2014–2018. Because of delays in the reporting of deaths, prevalence data are based on a 12-month reporting delay to allow data to be reported to CDC. For tables presenting prevalence data, region or area of residence is based on most recent known address as of the end of the specified year. Data for the year 2018 are preliminary and based on death data received by CDC through December 2019. Trends through 2018 should be interpreted with caution. Due to incomplete reporting of deaths for the year 2018, prevalence data for Alabama, Oklahoma, South Carolina, and the U.S. Virgin Islands should be interpreted with caution.
Gender identity refers to a person’s internal understanding of their own gender, or gender with which a person identifies. HIV surveillance personnel collect data on gender identity, when available, from sources such as case report forms submitted by health care or HIV testing providers and medical records, or by matching with other health department databases (e.g., Ryan White program data). In May 2013, CDC issued guidance to state and local programs on methods for collecting data on transgender persons and working with transgender-specific data. However, characterization of HIV infection among transgender persons may require supplemental data from special studies. A person’s transgender status in NHSS is determined based on two variables – sex assigned at birth and current gender identity. Both variables are examined, using a two-step approach, to assess transgender status. Although not used in this report, cisgender is a term used to indicate that a person’s sex assigned at birth and current gender identity are the same (i.e., a person assigned male at birth and who currently identifies as a man, is a cisgender male).
Categories
- Male: persons assigned “male” sex at birth and current gender identity is not “transgender male-to-female” or “additional gender identity” (current gender identity can be listed as “male,” “female,” “transgender female-to-male,” “unspecified,” or left blank).
- Female: persons assigned “female” sex at birth and current gender identity is not “transgender female-to-male” or “additional gender identity” (current gender identity can be listed as “male,” “female,” “transgender male-to-female,” “unspecified,” or left blank).
- Transgender male-to-female (transgender MTF): persons assigned “male” sex at birth and current gender identity is “transgender male-to-female.”
- Transgender female-to-male (transgender FTM): persons assigned “female” sex at birth and current gender identity is “transgender female-to-male.”
- Additional gender identity (AGI): persons assigned “male” or “female” sex at birth and current gender identity is “additional gender identity.” AGI includes “bigender,” “gender queer,” and “two-spirit.”
In the Federal Register [6] for October 30, 1997, the Office of Management and Budget (OMB) announced the Revisions to the Standards for the Classification of Federal Data on Race and Ethnicity. Implementation by January 1, 2003 was mandated. At a minimum, data on the following race categories should be collected:
- American Indian or Alaska Native
- Asian
- black or African American
- Native Hawaiian or other Pacific Islander
- white
Additionally, systems must be able to retain information when multiple race categories are reported. In addition to data on race, data on 2 categories of ethnicity should be collected:
- Hispanic or Latino
- not Hispanic or Latino
The Asian or Pacific Islander category displayed in annual surveillance reports published prior to the 2007 surveillance report was split into 2 categories: (1) Asian and (2) Native Hawaiian or other Pacific Islander. The Asian category (in tables where footnoted) includes the cases in Asians/Pacific Islanders (referred to as legacy cases) that were reported before the implementation of the new race categories in 2003 (e.g., cases of HIV infection that were diagnosed and reported to CDC before 2003 but that were classified as stage 3 [AIDS] after 2003) and a small percentage of cases that were reported after 2003 but that were reported according to the old race category (Asian/ Pacific Islander). In tables of diagnoses of HIV infection during 2014–2018, the Asian category does not include Asian/Pacific Islander cases because these cases were diagnosed after 2003 and were reported to CDC in accordance with OMB’s Revisions to the Standards for the Classification of Federal Data on Race and Ethnicity [6].
This report also presents data for persons for whom multiple race categories are reported. In this report, persons categorized by race were not Hispanic or Latino. The number of persons reported in each race category may, however, include persons whose ethnicity was not reported.
Transmission category is the term for the classification of cases that summarizes an adult’s or adolescent’s possible HIV risk factors; the summary classification results from selecting, from the presumed hierarchical order of probability, the 1 (single) risk factor most likely to have been responsible for transmission. For surveillance purposes, a diagnosis of HIV infection is counted only once in the hierarchy of transmission categories [7]. Adults or adolescents with more than 1 reported risk factor for HIV infection are classified in the transmission category listed first in the hierarchy. The exception is men who had sexual contact with other men and injected drugs; this group makes up a separate transmission category.
Hierarchical Categories:
- Male-to-male sexual contact: men who have had sexual contact with men (i.e., homosexual contact) and men who have had sexual contact with both men and women (i.e., bisexual contact)
- Injection drug use (IDU): persons who have injected non-prescription drugs
- Male-to-male sexual contact and injection drug use (male-to-male sexual contact and IDU): men who have had sexual contact with other men and injected non-prescription drugs
- Heterosexual contact: persons who have ever had heterosexual contact with a person known to have, or to be at high risk for, HIV infection
- Perinatal: persons infected through perinatal transmission but aged 13 years and older at time of diagnosis of HIV infection. Prevalence data and tables of death data includes persons infected through perinatal transmission but aged 13 years and older during the specified year or at death.
- Other: all other transmission categories (e.g., blood transfusion, hemophilia, risk factor not reported or not identified).
Cases of HIV infection reported without a risk factor listed in the hierarchy of transmission categories are classified as “no identified risk (NIR).” Cases classified as NIR include cases that are being followed up by local health department staff; cases in persons whose risk-factor information is missing because they died, declined to be interviewed, or were lost to follow-up; and cases in persons who were interviewed or for whom other follow-up information was available but for whom no risk factor was identified.
Because a substantial proportion of cases of HIV infection are reported to CDC without an identified risk factor, multiple imputation is used to assign a transmission category to these cases [7]. Multiple imputation is a statistical approach in which each missing transmission category is replaced with a set of plausible values that represent the uncertainty about the true, but missing, value [8]. Each resulting data set containing the plausible values is analyzed by using standard procedures, and the results from these analyses are then combined to produce the final results. In tables displaying transmission categories, multiple imputation was used for adults and adolescents, but not for children (because the number of cases in children is small, missing transmission categories were not imputed).
Data by region reflect the address at the time of diagnosis of HIV infection for figures and tables that present number of diagnoses (Figures 17, 19, 24; Tables 1a/b–7a/b). For tables presenting prevalence data (14a/b–17a/b), region is based on most recent known address as of the end of the specified year. For the death tables (10a/b–13a/b), region is based on residence at death. When information on residence at death is not available, the state where a person’s death occurred is used.
The 4 regions of residence and 6 dependent areas used in this report are defined by the U.S. Census Bureau as follows:
- Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont
- Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin
- South: Alabama, Arkansas, Delaware, District of Columbia (D.C.), Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia
- West: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming
- U.S. dependent areas: American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, the Republic of Palau, and the U.S. Virgin Islands
AGI: additional gender identity
AIDS: acquired immunodeficiency syndrome
CDC: Centers for Disease Control and Prevention
FTM: female-to-male
HIV: human immunodeficiency virus
IDU: injection drug use
MSA: metropolitan statistical area
MSM: gay, bisexual, and other men who have sex with men
MTF: male-to-female
NHSS: National HIV Surveillance System
NIR: no identified risk factor
OI: opportunistic illness
OMB: Office of Management and Budget
PrEP: preexposure prophylaxis
PWID: persons who inject drugs
