Diagnoses of HIV Infection in the United States and Dependent Areas, 2018: Deaths

All rates are per 100,000 population. The standard used for reporting trends in numbers and rates is an increase or a decrease of 5% or more during the specified time frame (e.g., when comparing 2014 and 2018). The exceptions to this standard are where numbers were small (i.e., less than 12) or rates were based on small numbers.
Please read all titles and footnotes carefully to ensure a complete understanding of the displayed data.
Figure 7. Rates of Deaths of Adults and Adolescents with Diagnosed HIV Infection, 2018—United States and 6 Dependent Areas
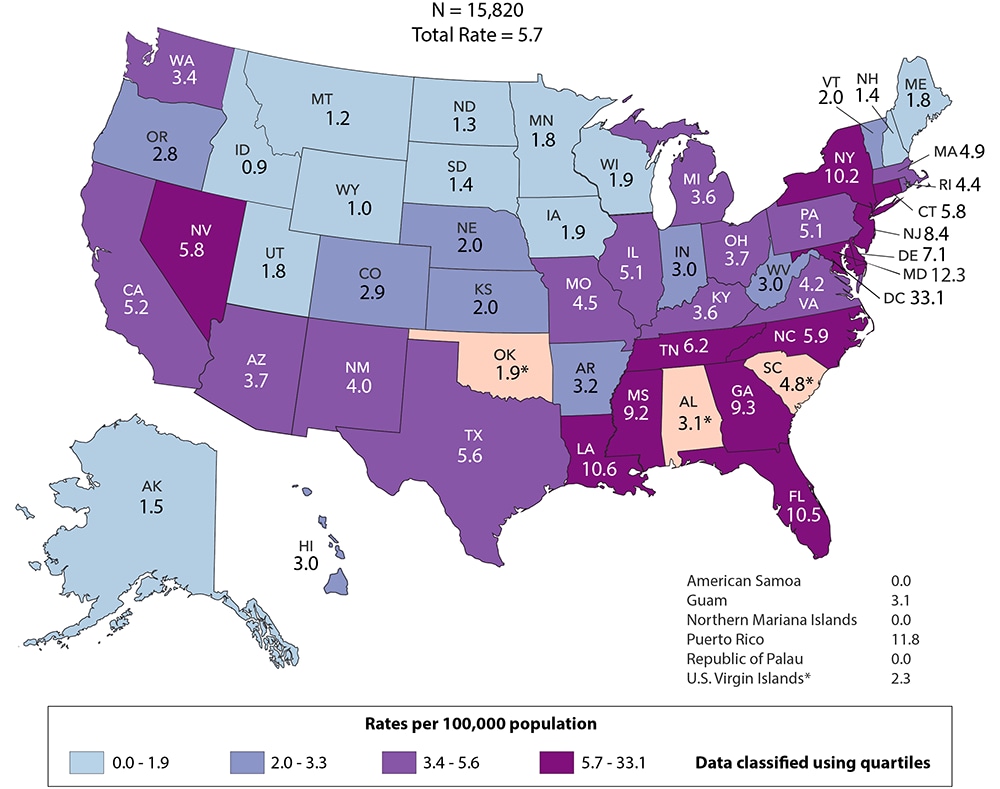
Note: Data for the year 2018 are preliminary and based on deaths reported to CDC as of December 2019. Data are based on address of residence at death. Asterisk (*) indicates incomplete reporting. See Data Tables, Definitions, and Acronyms for more information on deaths.
From 2014 through 2018 in the United States and 6 dependent areas, the rate of deaths of persons with diagnosed HIV infection decreased; the number of deaths remained stable (Table 10b). In 2018 in the United States and 6 dependent areas, the rate of deaths of adults and adolescents with diagnosed HIV infection was 5.7 (Figure 7). By region, the rate of deaths in the Northeast and South decreased (Table 10b). The rates of deaths in the Midwest and West remained stable. In 2018, rates were 6.1 in the Northeast, 5.9 in the South, 3.5 in the West, and 2.8 in the Midwest (Table 10b). Deaths of persons with diagnosed HIV infection may be due to any cause (i.e., may or may not be related to HIV infection). Data for the year 2018 are preliminary and based on deaths reported to CDC through December 2019.
Gender
From 2014 through 2018 in the United States and 6 dependent areas, the number of deaths for transgender MTF adults and adolescents with diagnosed HIV infection increased (Table 10b). The number of deaths for female adults and adolescents decreased. The number of deaths for male adults and adolescents remained stable. Please use caution when interpreting data for transgender FTM and AGI: the numbers are small.
Age Group
From 2014 through 2018 in the United States and 6 dependent areas, the rate of deaths for persons aged 65 years and older increased (Table 10b). The rates of deaths for persons aged 20–24, 30–34, 35–39, 40–44, 45–49, 50–54, and 55–59 years decreased. The rates of deaths for persons aged 25–29 and 60–64 years remained stable. Please use caution when interpreting data for children (aged less than 13 years at death) and persons aged 13–14 and 15–19 years: the numbers are small.
Figure 8. Rates of Deaths for Persons with Diagnosed HIV Infection, by Race/Ethnicity, 2014–2018—United States
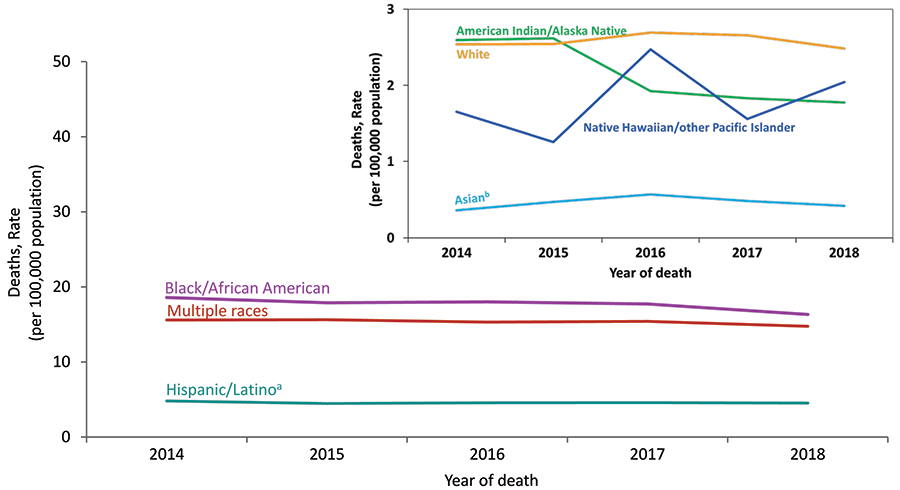
Note: Data for the year 2018 are preliminary and based on deaths reported to CDC as of December 2019. See Data Tables, Definitions, and Acronyms for more information on deaths and race/ethnicity.
a Hispanics/Latinos can be of any race.
b Includes Asian/Pacific Islander legacy cases.
From 2014 through 2018 in the United States, the rates of deaths for American Indians/Alaska Natives, blacks/African Americans, Hispanics/Latinos and persons of multiple races decreased (Figure 8 and Table 10a). The rates for Asians and whites remained stable. In 2018, the highest rate of deaths (16.3) was for blacks/African Americans (Table 10a). Please use caution when interpreting data for Native Hawaiians/other Pacific Islanders: the numbers are small.
Sex (at Birth) and Transmission Category
From 2014 through 2018 in the United States and 6 dependent areas, the overall rate of death among male adults and adolescents with diagnosed HIV infection, decreased (Table 10b). The number of deaths among males with HIV attributed to perinatal transmission increased. The number of deaths among males with HIV attributed to IDU decreased. The number of deaths among males with HIV attributed to male-to-male sexual contact, male-to-male sexual contact and IDU, or heterosexual contact remained stable. The perinatal and “Other” transmission categories accounted for less than 1% of cases. Overall, the rate of deaths for female adults and adolescents decreased. The number of deaths among females with infection attributed to perinatal transmission increased. The number of deaths among females with infection attributed to IDU and heterosexual contact decreased. The “Other” transmission category accounted for less than 1% of cases.
| 2014 | 2015 | 2016 | 2017 | 2018 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | Ratea | No. | Ratea | No. | Ratea | No. | Ratea | No. | Ratea | |
| Gender | ||||||||||
| Male | 11,882 | — | 11,858 | — | 12,255 | — | 12,257 | — | 11,595 | — |
| Female | 4,177 | — | 3,892 | — | 4,019 | — | 3,995 | — | 3,775 | — |
| Transgender male-to-femaleb | 84 | — | 108 | — | 121 | — | 103 | — | 110 | — |
| Transgender female-to-maleb | 3 | — | 5 | — | 2 | — | 4 | — | 3 | — |
| Additional gender identityc | 0 | — | 1 | — | 0 | — | 1 | — | 1 | — |
| Age at death (yr) | ||||||||||
| <13 | 1 | 0.0 | 4 | 0.0 | 2 | 0.0 | 2 | 0.0 | 1 | 0.0 |
| 13–14 | 2 | 0.0 | 0 | 0.0 | 1 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| 15–19 | 13 | 0.1 | 11 | 0.1 | 10 | 0.0 | 7 | 0.0 | 9 | 0.0 |
| 20–24 | 171 | 0.7 | 150 | 0.7 | 156 | 0.7 | 144 | 0.7 | 117 | 0.5 |
| 25–29 | 362 | 1.6 | 399 | 1.8 | 446 | 1.9 | 445 | 1.9 | 396 | 1.7 |
| 30–34 | 634 | 2.9 | 591 | 2.7 | 660 | 3.0 | 603 | 2.7 | 572 | 2.6 |
| 35–39 | 885 | 4.5 | 816 | 4.0 | 836 | 4.0 | 869 | 4.1 | 772 | 3.6 |
| 40–44 | 1,359 | 6.6 | 1,227 | 6.1 | 1,130 | 5.7 | 969 | 4.9 | 907 | 4.6 |
| 45–49 | 2,199 | 10.6 | 2,001 | 9.6 | 1,807 | 8.6 | 1,736 | 8.3 | 1,524 | 7.3 |
| 50–54 | 2,959 | 13.1 | 2,945 | 13.2 | 2,847 | 13.1 | 2,734 | 12.8 | 2,482 | 11.9 |
| 55–59 | 2,905 | 13.5 | 2,841 | 13.1 | 2,999 | 13.7 | 2,970 | 13.5 | 2,777 | 12.7 |
| 60–64 | 2,202 | 11.9 | 2,156 | 11.3 | 2,418 | 12.4 | 2,493 | 12.5 | 2,422 | 11.9 |
| ≥65 | 2,454 | 5.3 | 2,723 | 5.7 | 3,085 | 6.3 | 3,388 | 6.7 | 3,505 | 6.7 |
| Race/ethnicity | ||||||||||
| American Indian/Alaska Native | 61 | 2.6 | 62 | 2.6 | 46 | 1.9 | 44 | 1.8 | 43 | 1.8 |
| Asiand | 60 | 0.4 | 81 | 0.5 | 101 | 0.6 | 88 | 0.5 | 79 | 0.4 |
| Black/African American | 7,339 | 18.6 | 7,132 | 17.9 | 7,245 | 18.0 | 7,198 | 17.7 | 6,679 | 16.3 |
| Hispanic/Latinoe | 2,657 | 4.8 | 2,516 | 4.5 | 2,631 | 4.6 | 2,694 | 4.6 | 2,712 | 4.5 |
| Native Hawaiian/other Pacific Islander | 9 | 1.7 | 7 | 1.3 | 14 | 2.5 | 9 | 1.6 | 12 | 2.0 |
| White | 5,022 | 2.5 | 5,035 | 2.5 | 5,324 | 2.7 | 5,256 | 2.7 | 4,909 | 2.5 |
| Multiple races | 994 | 15.6 | 1,025 | 15.6 | 1,033 | 15.3 | 1,069 | 15.4 | 1,050 | 14.8 |
| Transmission categoryf | ||||||||||
| Male adult or adolescentg | ||||||||||
| Male-to-male sexual contact | 6,536 | — | 6,588 | — | 6,913 | — | 7,010 | — | 6,578 | — |
| Injection drug use | 2,413 | — | 2,283 | — | 2,284 | — | 2,168 | — | 2,114 | — |
| Male-to-male sexual contact and injection drug use | 1,344 | — | 1,398 | — | 1,390 | — | 1,373 | — | 1,378 | — |
| Heterosexual contacth | 1,581 | — | 1,588 | — | 1,686 | — | 1,705 | — | 1,528 | — |
| Perinatali | 32 | — | 28 | — | 39 | — | 41 | — | 50 | — |
| Otherj | 60 | — | 79 | — | 63 | — | 63 | — | 57 | — |
| Subtotal | 11,966 | 9.2 | 11,964 | 9.1 | 12,375 | 9.4 | 12,360 | 9.3 | 11,705 | 8.7 |
| Female adult or adolescentg | ||||||||||
| Injection drug use | 1,460 | — | 1,351 | — | 1,384 | — | 1,373 | — | 1,260 | — |
| Heterosexual contacth | 2,659 | — | 2,472 | — | 2,563 | — | 2,553 | — | 2,457 | — |
| Perinatali | 30 | — | 46 | — | 47 | — | 42 | — | 35 | — |
| Otherj | 29 | — | 27 | — | 26 | — | 29 | — | 26 | — |
| Subtotal | 4,179 | 3.1 | 3,896 | 2.8 | 4,020 | 2.9 | 3,998 | 2.9 | 3,778 | 2.7 |
| Child (<13 yrs at death) | ||||||||||
| Perinatal | 1 | — | 2 | — | 1 | — | 2 | — | 1 | — |
| Otherj | 0 | — | 2 | — | 1 | — | 0 | — | 0 | — |
| Subtotal | 1 | 0.0 | 4 | 0.0 | 2 | 0.0 | 2 | 0.0 | 1 | 0.0 |
| Region of residencek | ||||||||||
| Northeast | 3,732 | 6.7 | 3,588 | 6.4 | 3,705 | 6.6 | 3,689 | 6.6 | 3,450 | 6.1 |
| Midwest | 1,845 | 2.7 | 1,808 | 2.7 | 1,847 | 2.7 | 1,902 | 2.8 | 1,930 | 2.8 |
| South | 7,984 | 6.7 | 7,862 | 6.5 | 8,088 | 6.6 | 8,041 | 6.5 | 7,383 | 5.9 |
| West | 2,585 | 3.4 | 2,606 | 3.4 | 2,757 | 3.6 | 2,728 | 3.5 | 2,721 | 3.5 |
| Totall | 16,146 | 5.1 | 15,864 | 4.9 | 16,397 | 5.1 | 16,360 | 5.0 | 15,484 | 4.7 |
Note: Deaths of persons with a diagnosis of HIV infection may be due to any cause. Data for the year 2018 are preliminary and based on deaths reported to CDC as of December 2019.
Numbers less than 12, and rates and trends based on these numbers, should be interpreted with caution.
aRates are per 100,000 population. Rates are not calculated by gender or transmission category because of the lack of denominator data.
b“Transgender male-to-female” includes individuals who were assigned “male” sex at birth but have ever identified as “female” gender. “Transgender female-to-male” includes individuals who were assigned “female” sex at birth but have ever identified as “male” gender.
cAdditional gender identity examples include “bigender,” “gender queer,” and “two-spirit.”
dIncludes Asian/Pacific Islander legacy cases (see Technical Notes).
eHispanics/Latinos can be of any race.
fData have been statistically adjusted to account for missing transmission category, therefore values may not sum to column subtotals and total.
gData presented based on sex at birth and includes transgender persons.
hHeterosexual contact with a person known to have, or to be at high risk for, HIV infection.
iIncludes individuals ≥13 years of age at time of diagnosis of HIV infection.
jIncludes hemophilia, blood transfusion, and risk factor not reported or not identified.
kData are based on residence at death. When information on residence at death was not available, state at death (where a person’s death occurred) was used.
lIncludes persons whose race/ethnicity is unknown.
| 2014 | 2015 | 2016 | 2017 | 2018 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | Ratea | No. | Ratea | No. | Ratea | No. | Ratea | No. | Ratea | |
| Gender | ||||||||||
| Male | 12,223 | — | 12,152 | — | 12,575 | — | 12,555 | — | 11,865 | — |
| Female | 4,309 | — | 3,998 | — | 4,114 | — | 4,103 | — | 3,842 | — |
| Transgender male-to-femaleb | 84 | — | 108 | — | 121 | — | 104 | — | 110 | — |
| Transgender female-to-maleb | 3 | — | 5 | — | 2 | — | 4 | — | 3 | — |
| Additional gender identityc | 0 | — | 1 | — | 0 | — | 1 | — | 1 | — |
| Age at death (yr) | ||||||||||
| <13 | 1 | 0.0 | 4 | 0.0 | 2 | 0.0 | 2 | 0.0 | 1 | 0.0 |
| 13–14 | 2 | 0.0 | 0 | 0.0 | 1 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| 15–19 | 13 | 0.1 | 11 | 0.1 | 11 | 0.1 | 7 | 0.0 | 9 | 0.0 |
| 20–24 | 173 | 0.7 | 152 | 0.7 | 160 | 0.7 | 146 | 0.7 | 120 | 0.5 |
| 25–29 | 369 | 1.7 | 404 | 1.8 | 453 | 2.0 | 452 | 1.9 | 403 | 1.7 |
| 30–34 | 650 | 3.0 | 612 | 2.8 | 668 | 3.0 | 617 | 2.8 | 584 | 2.6 |
| 35–39 | 906 | 4.5 | 836 | 4.1 | 868 | 4.1 | 884 | 4.1 | 787 | 3.6 |
| 40–44 | 1,396 | 6.7 | 1,262 | 6.2 | 1,161 | 5.8 | 1,004 | 5.1 | 934 | 4.7 |
| 45–49 | 2,263 | 10.7 | 2,052 | 9.8 | 1,858 | 8.8 | 1,789 | 8.5 | 1,558 | 7.4 |
| 50–54 | 3,056 | 13.4 | 3,040 | 13.5 | 2,918 | 13.2 | 2,808 | 13.0 | 2,531 | 12.0 |
| 55–59 | 2,992 | 13.8 | 2,906 | 13.2 | 3,074 | 13.8 | 3,051 | 13.7 | 2,842 | 12.8 |
| 60–64 | 2,262 | 12.1 | 2,203 | 11.4 | 2,471 | 12.6 | 2,535 | 12.6 | 2,468 | 12.0 |
| ≥65 | 2,536 | 5.4 | 2,782 | 5.8 | 3,167 | 6.3 | 3,472 | 6.7 | 3,584 | 6.7 |
| Race/ethnicity | ||||||||||
| American Indian/Alaska Native | 61 | — | 62 | — | 46 | — | 44 | — | 43 | — |
| Asiand | 62 | — | 82 | — | 101 | — | 88 | — | 79 | — |
| Black/African American | 7,348 | — | 7,138 | — | 7,254 | — | 7,203 | — | 6,679 | — |
| Hispanic/Latinoe | 3,119 | — | 2,907 | — | 3,033 | — | 3,095 | — | 3,044 | — |
| Native Hawaiian/other Pacific Islander | 9 | — | 8 | — | 16 | — | 9 | — | 15 | — |
| White | 5,022 | — | 5,035 | — | 5,325 | — | 5,257 | — | 4,910 | — |
| Multiple races | 994 | — | 1,026 | — | 1,034 | — | 1,069 | — | 1,051 | — |
| Transmission categoryf | ||||||||||
| Male adult or adolescentg | ||||||||||
| Male-to-male sexual contact | 6,621 | — | 6,664 | — | 6,989 | — | 7,081 | — | 6,652 | — |
| Injection drug use | 2,558 | — | 2,415 | — | 2,413 | — | 2,299 | — | 2,224 | — |
| Male-to-male sexual contact and injection drug use |
1,371 | — | 1,424 | — | 1,421 | — | 1,397 | — | 1,397 | — |
| Heterosexual contacth | 1,663 | — | 1,647 | — | 1,762 | — | 1,777 | — | 1,592 | — |
| Perinatali | 32 | — | 29 | — | 45 | — | 42 | — | 53 | — |
| Otherj | 62 | — | 80 | — | 63 | — | 63 | — | 58 | — |
| Subtotal | 12,307 | 9.4 | 12,258 | 9.2 | 12,695 | 9.5 | 12,659 | 9.4 | 11,975 | 8.8 |
| Female adult or adolescentg | ||||||||||
| Injection drug use | 1,502 | — | 1,375 | — | 1,419 | — | 1,408 | — | 1,284 | — |
| Heterosexual contacth | 2,748 | — | 2,554 | — | 2,620 | — | 2,625 | — | 2,498 | — |
| Perinatali | 31 | — | 47 | — | 49 | — | 44 | — | 37 | — |
| Otherj | 29 | — | 27 | — | 27 | — | 29 | — | 26 | — |
| Subtotal | 4,311 | 3.1 | 4,002 | 2.9 | 4,115 | 2.9 | 4,106 | 2.9 | 3,845 | 2.7 |
| Child (<13 yrs at death) | ||||||||||
| Perinatal | 1 | — | 2 | — | 1 | — | 2 | — | 1 | — |
| Otherj | 0 | — | 2 | — | 1 | — | 0 | — | 0 | — |
| Subtotal | 1 | 0.0 | 4 | 0.0 | 2 | 0.0 | 2 | 0.0 | 1 | 0.0 |
| Region of residencek | ||||||||||
| Northeast | 3,732 | 6.7 | 3,588 | 6.4 | 3,705 | 6.6 | 3,689 | 6.6 | 3,450 | 6.1 |
| Midwest | 1,845 | 2.7 | 1,808 | 2.7 | 1,847 | 2.7 | 1,902 | 2.8 | 1,930 | 2.8 |
| South | 7,984 | 6.7 | 7,862 | 6.5 | 8,088 | 6.6 | 8,041 | 6.5 | 7,383 | 5.9 |
| West | 2,585 | 3.4 | 2,606 | 3.4 | 2,757 | 3.6 | 2,728 | 3.5 | 2,721 | 3.5 |
| U.S. dependent areas | 473 | 12.0 | 400 | 10.3 | 415 | 10.9 | 407 | 10.9 | 337 | 9.4 |
| Totall | 16,619 | 5.2 | 16,264 | 5.0 | 16,812 | 5.1 | 16,767 | 5.1 | 15,821 | 4.8 |
Note: Deaths of persons with a diagnosis of HIV infection may be due to any cause. Data for the year 2018 are preliminary and based on deaths reported to CDC as of December 2019.
Numbers less than 12, and rates and trends based on these numbers, should be interpreted with caution.
aRates are per 100,000 population. Rates are not calculated by gender or transmission category because of the lack of denominator data. Rates by race/ethnicity are not provided because U.S. census information is limited for U.S. dependent areas.
bTransgender male-to-female” includes individuals who were assigned “male” sex at birth but have ever identified as “female” gender. “Transgender female-to-male” includes individuals who were assigned “female” sex at birth but have ever identified as “male” gender.
cAdditional gender identity examples include “bigender,” “gender queer,” and “two-spirit.”
dIncludes Asian/Pacific Islander legacy cases (see Technical Notes).
eHispanics/Latinos can be of any race.
fData have been statistically adjusted to account for missing transmission category, therefore values may not sum to column subtotals and total.
gData presented based on sex at birth and includes transgender persons.
hHeterosexual contact with a person known to have, or to be at high risk for, HIV infection.
iIncludes individuals ≥13 years of age at time of diagnosis of HIV infection.
jIncludes hemophilia, blood transfusion, and risk factor not reported or not identified.
kData are based on residence at death. When information on residence at death was not available, state at death (where a person’s death occurred) was used.
lIncludes persons whose race/ethnicity is unknown.
Persons reported to the National HIV Surveillance System are assumed alive unless their deaths have been reported to CDC. Death data include deaths of persons with diagnosed HIV infection (Figures 7 and 8; Tables 10a/b–13a/b) regardless of the cause of death. Death data are based on a 12-month reporting delay to allow data to be reported to CDC. For the death tables, region or area of residence is based on residence at death. When information on residence at death is not available, the state where a person’s death occurred is used. Data for the year 2018 are preliminary and based on death data received by CDC through December 2019. Trends through 2018 should be interpreted with caution. Due to incomplete reporting of deaths for the year 2018, death data for Alabama, Oklahoma, South Carolina, and the U.S. Virgin Islands should be interpreted with caution.
In the Federal Register [6] for October 30, 1997, the Office of Management and Budget (OMB) announced the Revisions to the Standards for the Classification of Federal Data on Race and Ethnicity. Implementation by January 1, 2003 was mandated. At a minimum, data on the following race categories should be collected:
- American Indian or Alaska Native
- Asian
- black or African American
- Native Hawaiian or other Pacific Islander
- white
Additionally, systems must be able to retain information when multiple race categories are reported. In addition to data on race, data on 2 categories of ethnicity should be collected:
- Hispanic or Latino
- not Hispanic or Latino
The Asian or Pacific Islander category displayed in annual surveillance reports published prior to the 2007 surveillance report was split into 2 categories: (1) Asian and (2) Native Hawaiian or other Pacific Islander. The Asian category (in tables where footnoted) includes the cases in Asians/Pacific Islanders (referred to as legacy cases) that were reported before the implementation of the new race categories in 2003 (e.g., cases of HIV infection that were diagnosed and reported to CDC before 2003 but that were classified as stage 3 [AIDS] after 2003) and a small percentage of cases that were reported after 2003 but that were reported according to the old race category (Asian/ Pacific Islander). In tables of diagnoses of HIV infection during 2014–2018, the Asian category does not include Asian/Pacific Islander cases because these cases were diagnosed after 2003 and were reported to CDC in accordance with OMB’s Revisions to the Standards for the Classification of Federal Data on Race and Ethnicity [6].
This report also presents data for persons for whom multiple race categories are reported. In this report, persons categorized by race were not Hispanic or Latino. The number of persons reported in each race category may, however, include persons whose ethnicity was not reported.
AGI: additional gender identity
AIDS: acquired immunodeficiency syndrome
CDC: Centers for Disease Control and Prevention
FTM: female-to-male
HIV: human immunodeficiency virus
IDU: injection drug use
MSA: metropolitan statistical area
MSM: gay, bisexual, and other men who have sex with men
MTF: male-to-female
NHSS: National HIV Surveillance System
NIR: no identified risk factor
OI: opportunistic illness
OMB: Office of Management and Budget
PrEP: preexposure prophylaxis
PWID: persons who inject drugs