How Does Treatment as Prevention Benefit My Patients with HIV?
- Taking HIV treatment prevents sexual transmission of HIV.
- Treatment as prevention helps people with HIV stay healthy and avoid transmitting HIV to others.
- Health care providers who treat patients with HIV have an important role in supporting HIV prevention.
- Help your patients overcome common challenges to maximize the benefits of treatment as prevention.
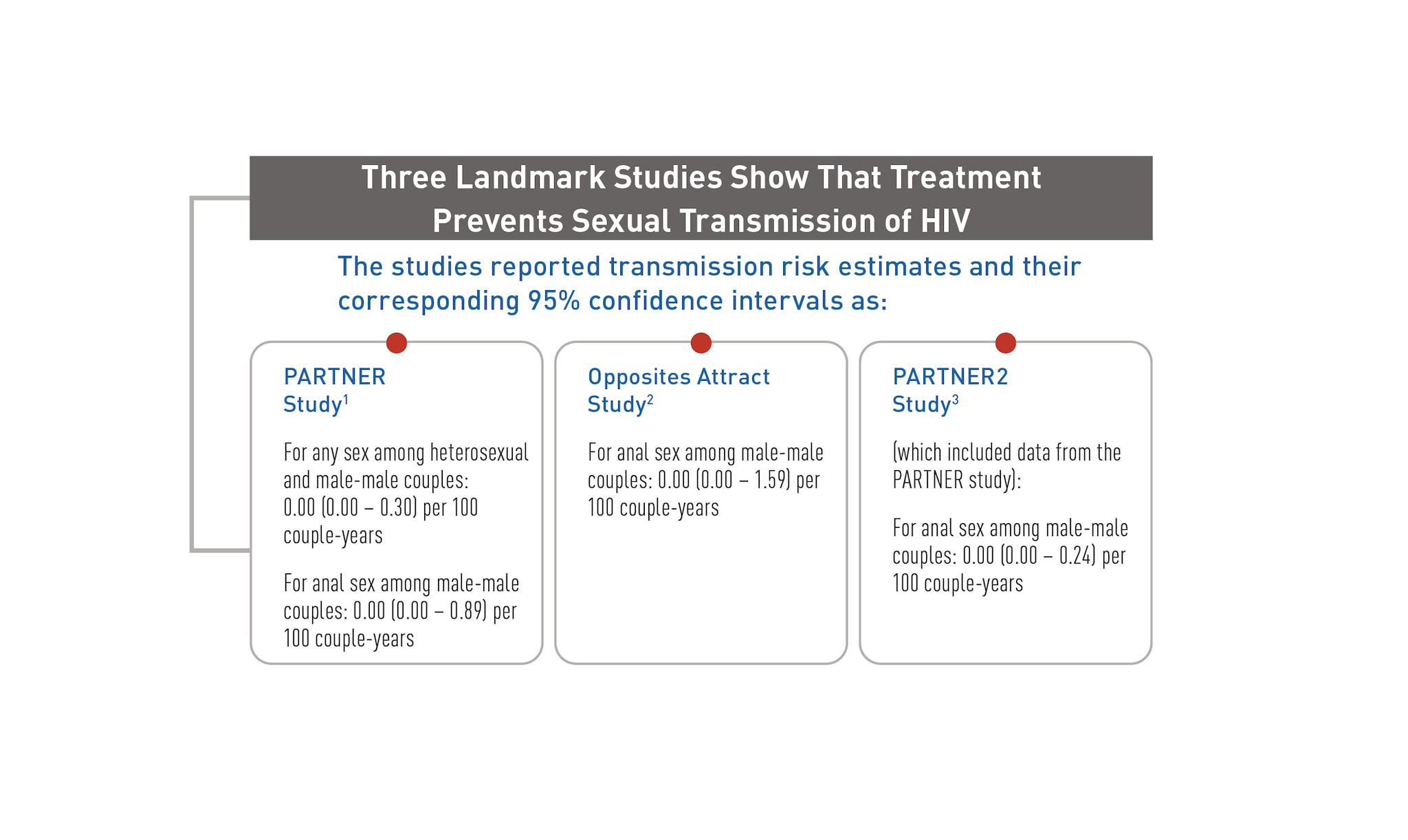
Three landmark studies have shown that treatment prevents sexual transmission of HIV.1-3 Across all three studies, no linked HIV transmissions were observed between mixed-HIV-status partners when the partner with HIV was virally suppressed (defined in these studies as having a plasma HIV RNA viral load less than either 200 or 400 copies/mL).
These data provide conclusive evidence of the power of viral suppression in preventing HIV transmission. Although statistically, a non-zero risk estimate can never be completely ruled out in a mathematical sense, despite the number of observations, the data tell us that the best estimate for the transmission risk is zero and that future HIV transmissions are not expected when people with HIV remain virally suppressed.
Based on the evidence, people with HIV who take HIV medicine as prescribed and get and keep an undetectable viral load (or stay virally suppressed) won’t transmit HIV to their HIV-negative sexual partners.
If taken as prescribed, antiretroviral therapy (ART) reduces the amount of HIV in the body (viral load) to a very low level, which keeps the immune system working and prevents illness. This is called viral suppression—defined as having less than 200 copies of HIV per milliliter of blood. HIV medicine can even make the viral load so low that a test can’t detect it. This is called an undetectable viral load.
Getting and keeping an undetectable viral load by taking ART is the best thing your patients with HIV can do to stay healthy and prevent transmission of HIV to others through sex. This is sometimes referred to as treatment as prevention (TasP). Your patients may also refer to treatment as prevention as Undetectable = Untransmittable or U=U. The U=U campaign was developed by members of the HIV community to increase awareness about the relationship between viral suppression and the prevention of sexual transmission of HIV.
There is strong evidence about treatment as prevention for preventing HIV transmission through sex, but more research is needed for other ways, including breast/chestfeeding and injection drug use.
Treatment as prevention is one of the most powerful tools we have to stop the sexual transmission of HIV. Adopting HIV treatment as prevention as an intervention strategy is one of the best things you can do for your patients’ health. Motivate your patients with HIV to live longer, healthier lives by talking with them about the benefits of viral suppression and the prevention steps they are taking.
Health care providers who treat patients with HIV have an important role in supporting HIV prevention. Talking to your patients with HIV about treatment as prevention is one of the best things you can do for their overall health and to stop HIV transmission. Because a patient’s needs may change over time, engage each patient in brief conversations at every visit to discuss the prevention steps they are taking and whether treatment as prevention is right for them. These conversations can help you become more familiar with each patient, including their adherence and transmission risk. In addition, these conversations can normalize discussions about factors that may affect your patients’ health, such as sex, substance use, and mental health disorders.
Use the following tips and conversation starters to support your patients with HIV:
- Share information with your patients about the research on treatment as prevention and then ask them open-ended questions to start the conversation.
- Talk about the benefits of achieving and maintaining an undetectable viral load, including not being able to sexually transmit HIV to others.
- Emphasize that while treatment as prevention is a highly effective prevention strategy, its success depends on achieving and maintaining an undetectable viral load. Note that if a patient’s viral load increases, so does their risk of transmitting HIV to their HIV-negative partners through sex.
- Discuss the prevention steps your patients are taking to help them adhere to their treatment regimen and maintain an undetectable viral load.
- Use the information your patients share with you to identify barriers they may have to adhering to ART and regular, ongoing care that may make it difficult for them to achieve and maintain viral suppression.
Your patients with HIV who use or want to use ART as their primary means of prevention may benefit from additional prevention methods if either partner desires added security for HIV protection or is concerned about sexually transmitted infections (STIs). These methods could include pre-exposure prophylaxis (PrEP) and/or condoms. Using multiple HIV prevention methods is especially important if the person with HIV has trouble with adhering to ART, has taken ART for less than 6 months, or has not yet achieved or maintained viral suppression.
To help all people with HIV and their partners get maximal benefit from treatment as prevention as an intervention strategy, it is important for providers, people with HIV, and their partners to have clear information regarding the benefits of and the challenges with achieving and maintaining viral suppression. Some challenges are further detailed in the text boxes below.
Most people will achieve an undetectable viral load within 6 months of starting ART. Many will become undetectable very quickly, but it could take more time for some.
Regular viral load testing is critical to confirm that an individual has achieved and is maintaining an undetectable viral load. Data show a discordance between some people’s self-report of their viral load status and laboratory measurements, suggesting that people may not know or be able to accurately report their viral load level.4 It is not known if viral load testing should be conducted more frequently than currently recommended for treatment if someone is relying on treatment and viral suppression as a prevention strategy.
Taking HIV medicine and achieving and maintaining an undetectable viral load do not protect either partner from getting other STIs. Other prevention strategies are needed to provide protection from STIs.
Knowledge of the prevention benefits of viral suppression may help motivate people with HIV and their partners to adopt this strategy. Studies have shown that a significant proportion of people do not know or do not believe that viral suppression works for prevention.
For example, message testing conducted by the Centers for Disease Control and Prevention (CDC) found that many participants did not believe information about the prevention benefits of viral suppression. And a survey among over 12,000 men who have sex with men showed that the majority of participants who were HIV negative and nearly one-third of participants with HIV thought that a message about the prevention benefits of having an undetectable viral load was inaccurate.5
Furthermore, even when individuals understand that having an undetectable viral load protects against HIV transmission, they still tend to estimate the risk of transmission as being far higher than is accurate.6
1 Rodger AJ, Cambiano V, Bruun T, et al. Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. JAMA. 2016;316(2):171-181. https://jamanetwork.com/journals/jama/article-abstract/2533066?casa_token=PPyQ-13D4D4AAAAA:zp67b1UMYY7vWhYBD7tz9sdsZeeDsf-kXacq123SlcZLMRACiyKCdCQVwNNLIOnYEhucliS6mQ
2 Bavinton BR, Pinto AN, Phanuphak N, et al. Viral suppression and HIV transmission in serodiscordant male couples: an international, prospective, observational, cohort study. Lancet HIV. 2018;5(8):e438-e447. https://www.sciencedirect.com/science/article/abs/pii/S2352301818301322
3 Rodger AJ, Cambiano V, Bruun T, et al. Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): final results of a multicentre, prospective, observational study. Lancet. 2019;393(10189):2428-2438. https://www.sciencedirect.com/science/article/pii/S0140673619304180
4 Mustanski B, Ryan DT, Remble TA, D’Aquila RT, Newcomb ME, Morgan E. Discordance of self-report and laboratory measures of HIV viral load among young men who have sex with men and transgender women in Chicago: implications for epidemiology, care, and prevention. AIDS Behav. 2018;22(7):2360-2367. https://link.springer.com/article/10.1007/s10461-018-2112-7
5 Rendina HJ, Parsons JT. Factors associated with perceived accuracy of the Undetectable = Untransmittable slogan among men who have sex with men: implications for messaging scale-up and implementation. J Int AIDS Soc. 2018;21(1):e25055. https://onlinelibrary.wiley.com/doi/full/10.1002/jia2.25055
6 Rendina HJ, Cienfuegos-Szalay J, Talan A, Jones SS, Jimenez RH. Growing acceptability of Undetectable = Untransmittable but widespread misunderstandings of transmission risk: findings from a very large sample of sexual minority men in the United States. J Acquir Immune Defic Syndr. 2020;83(3):215-222. https://journals.lww.com/jaids/Fulltext/2020/03010/Growing_Acceptability_of_Undetectable__.4.aspx