How Does Routine HIV Screening Benefit My Patients?
- HIV screening is the first step in CDC’s status-neutral approach to prevention and care.
- Patients at risk for HIV who test negative can access prevention tools, such as condoms and pre-exposure prophylaxis (PrEP).
- Patients who test positive for HIV can be linked to HIV care to reduce HIV-associated morbidity and mortality and prevent transmission to their partners.
It all starts with an HIV test, but routine HIV screening is only the first step. To improve their health outcomes, all people with HIV must have access to the full continuum of HIV prevention and care.
Linking your patients to prevention and care services is essential.1 The HIV prevention and care continuum is an ongoing, lifelong process that encompasses HIV testing, prevention, and care. CDC’s status-neutral approach to HIV prevention and care ensures that all patients can benefit from quality HIV prevention and care, regardless of their HIV status.
- Patients who have negative HIV tests should be offered prevention tools.
- Patients who have positive HIV tests should be linked to HIV treatment and care.
CDC’s status-neutral approach is shown in more detail in the graphic below.2
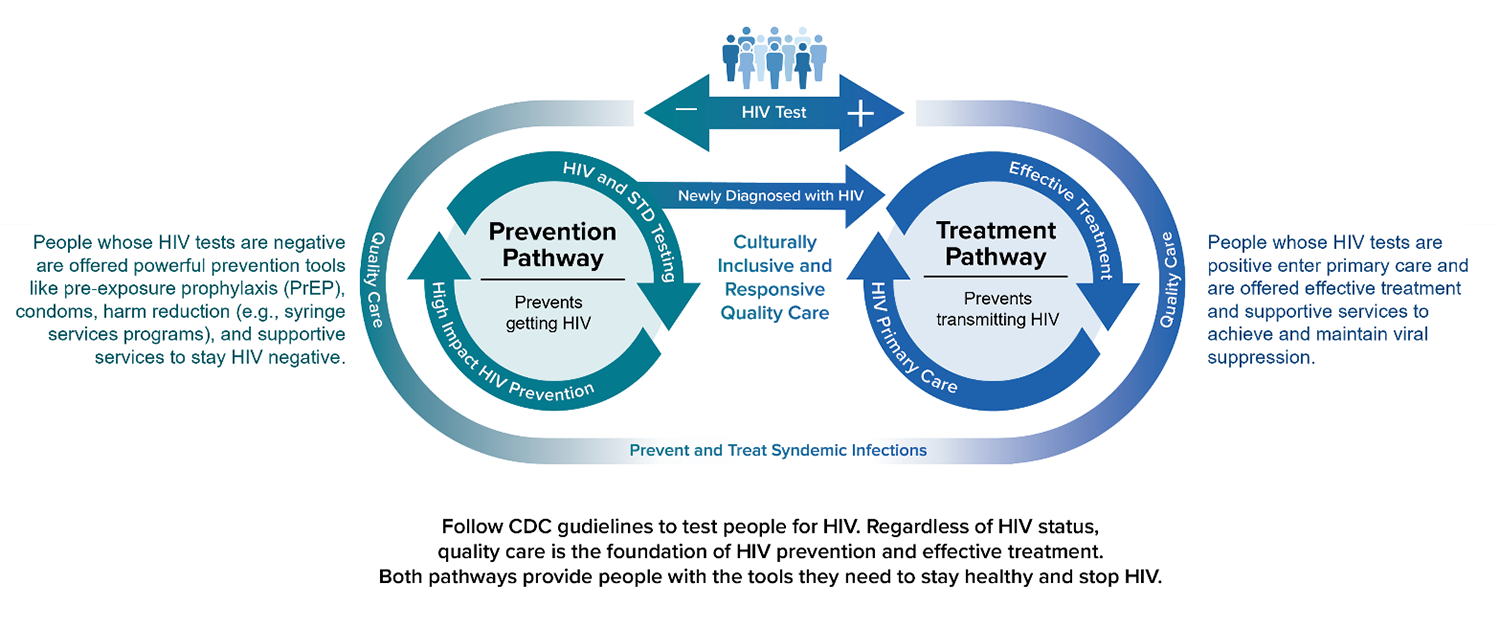
Using the status-neutral approach, any HIV test result, positive or negative, should support the same goal: keeping patients and their partners healthy.
Health care providers who routinely screen for HIV play a key role in improving outcomes at each step of the HIV prevention and care continuum.3 For patients with a negative HIV result, assess their needs and risk and link them to prevention tools, such as PrEP, condoms, and risk-reduction counseling. Retain these patients in ongoing prevention services and re-test them for HIV as long as they remain at risk for HIV infection.
Not all people with HIV are getting the care and treatment they need. For those with a positive HIV test result, studies have demonstrated the benefits of early HIV diagnosis in terms of patients’ health outcomes.4,5 Link patients newly diagnosed with HIV to treatment and care services so that they can start antiretroviral therapy (ART).6
ART reduces HIV-associated morbidity and mortality. The Centers for Disease Control and Prevention (CDC) recommends that people start treatment as soon as possible after diagnosis to gain maximum benefit from ART. Evidence suggests that starting ART before advanced immunodeficiency is one of several interventions that reduces the risk of serious non-AIDS events, such as cardiovascular disease, renal disease, hepatic disease, and cancer, as well as lowers the risk of mortality.7 Untreated HIV replication increases risk of serious non-AIDS events.7-9
- Reduces HIV-associated morbidity and mortality
- Greatly decreases HIV transmission to others
- May reduce the risk of serious non-AIDS-related diseases
1 Branson B, Handsfield HH, Lampe MA, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health care settings. MMWR Morb Mortal Wkly Rep. 2006;55(RR14):1-17. https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5514a1.htm
2 The White House. National HIV/AIDS strategy for the United States 2022–2025. Published 2021. Accessed February 2, 2022. https://www.whitehouse.gov/wp-content/uploads/2021/11/National-HIV-AIDS-Strategy.pdf
3 Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data: United States and 6 dependent areas, 2019. HIV Surveillance Report: Supplemental Report. 2021;26(2). https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-vol-26-no-2.pdf
4 Bavinton B, Grinsztejn B, Phanuphak N, et al, for the Opposites Attract Study Group. HIV treatment prevents HIV transmission in male serodiscordant couples in Australia, Thailand and Brazil. Presented at the 9th IAS Conference on HIV Science; July 25, 2017; Paris, France. http://programme.ias2017.org/abstract/abstract/5469
5 Rodger AJ, Cambiano V, Bruun T, et al., for the PARTNER Study Group. Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. JAMA. 2016;316(2):171-181. https://jamanetwork.com/journals/jama/article-abstract/2533066?casa_token=u5s_q-3M5V4AAAAA:TwYakEQkz2vyYx-8ufv29tS2W79hw4L8IBgqETWU1wIdG_oiVTS_gvtnNo0wYEAEFnXtlnAxTw
6 Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Department of Health and Human Services. Accessed November 17, 2020. https://clinicalinfo.hiv.gov/sites/default/files/guidelines/documents/adult-adolescent-arv/guidelines-adult-adolescent-arv.pdf
7 Hsu, D, Sereti I, Ananworanich J. Serious non-AIDS events: Immunopathogenesis and interventional strategies. AIDS Res Ther. 2013;10(29):217. https://link.springer.com/article/10.1186/1742-6405-10-29
8 Triant VA. HIV infection and coronary heart disease: an intersection of epidemics. J Infect Dis. 2012;205:S355-S3618. https://academic.oup.com/jid/article/205/suppl_3/S355/937817?login=true
9 Wyatt CM. Kidney disease and HIV infection. Top Antivir Med. 2017;25(1):13-16. https://pubmed.ncbi.nlm.nih.gov/28402929/