Reducing the Risk of SARS-CoV-2 Spreading between People and Wildlife
What You Need to Know
- These recommendations may make it less likely for the virus that causes COVID-19 to spread between people and wildlife. This can protect human and animal health.
- Some species of wildlife can be infected with SARS-CoV-2, and there is evidence that some free-ranging wildlife have been infected in the United States. However, the risk of getting COVID-19 from animals in the United States, including wildlife, is low.
- We are still learning about this virus, but we know that it can spread from people to susceptible animal species, including wildlife, in some situations, especially after close contact with a person who has COVID-19. For this reason, the virus may threaten the health and welfare of wildlife and could negatively impact conservation efforts.
- Anyone who comes in close contact with wildlife should consider the information below to minimize the spread of SARS-CoV-2 between people and wildlife.
Overview
Many studies have been done to learn about how SARS-CoV-2 can affect different animals. Based on these studies, we know that only mammals are susceptible to SARS-CoV-2 infection. Natural infections in wild mammals have been confirmed in white-tailed deer, mule deer, and wild mink. This guidance therefore uses the term “wildlife” in reference to mammalian wildlife.
The risk of getting COVID-19 from animals in the United States, including wildlife, is low. More studies are needed to understand how the virus can spread in wildlife.
Considerations for Members of the Public
Because wildlife can carry multiple zoonotic diseases, even without looking sick, it is always important to enjoy wildlife from a distance.
To prevent getting sick from wildlife in the United States:
- Keep your family, including pets, a safe distance away from wildlife.
- Do not feed wildlife or touch wildlife droppings.
- Keep pets away from wildlife and their droppings.
- Always wash your hands and supervise children washing their hands after working or playing outside.
- Leave young animals alone. Often, the parents are close by and will return for their young.
- Do not approach or touch a sick or dead animal – contact your state wildlife agency
- Consult your state wildlife agency’s guidance if you are preparing or consuming legally harvested game meat.
Considerations for Hunters
There is currently no evidence that you can get COVID-19 by preparing or eating food, including wild hunted game meat in the United States. However, hunters should practice good hygiene and follow these recommendations to prevent getting sick:
- Do not allow contact between wildlife and domestic animals, including pets and hunting dogs.
- Do not harvest animals that appear sick or are found dead.
- Keep game meat clean and cool the meat down as soon as possible after harvesting the animal.
These safety practices can reduce risk when handling and cleaning game, and are especially important for people who hunt deer:
- Wear a mask to reduce your risk of coming into contact with germs spread through respiratory droplets. Preparing a carcass may make aerosols (small droplets and particles in the air) which could contain the virus.
- Wear rubber or disposable gloves.
- Do not eat, drink, or smoke when handling and cleaning game.
- Avoid cutting through the backbone and spinal tissues and do not eat the brains of wildlife.
- When finished handling and cleaning game:
- Wash your hands thoroughly with soap and water.
- Do not touch your eyes, nose, or mouth with unwashed hands.
- Clean knives, equipment, and surfaces that were in contact with game meat with soap and water and then disinfect them.
- Cook all game meat thoroughly (to an internal temperature of 165°F or higher).
- Check with your state wildlife agency about testing requirements for other diseases and for specific instructions on preparing, transporting, and eating game meat.
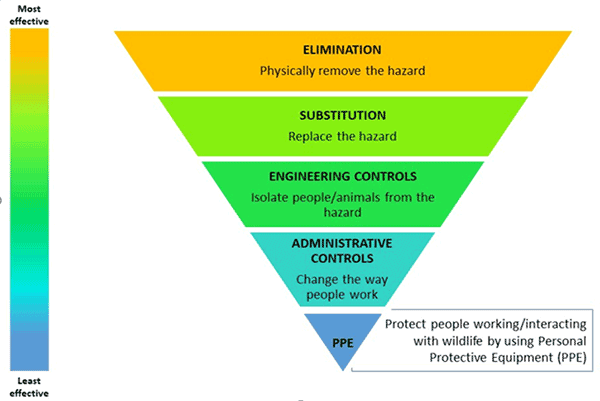
Hierarchy of Controls to Lower the Risk of the Virus that Causes COVID-19 Spreading between People and Wildlife
The Hierarchy of Controls is a standard tool applied in occupational safety and health practices to minimize exposure to hazards by using effective control solutions. The Hierarchy of Controls approach is used in the following sections to provide context for minimizing disease spread between people and wildlife.
Using controls near the top of the hierarchy leads to an inherently safer approach than using only controls near the bottom. Levels of control are not mutually exclusive and can be combined as needed.
Considerations for Agencies or Programs Conducting Wildlife Research, Wildlife Management, and Wildlife Control Activities
Activities that involve being close to or directly handling wildlife can increase the chances that people with COVID-19 could spread the virus to people or animals. Federal, state, tribal, local, and territorial wildlife agencies may consider additional restrictions or other measures to reduce the possibility that:
- Susceptible wildlife are exposed to the virus by people who are infected;
- Infected wildlife spread the virus;
- Infected wildlife spread the virus back to people in the future.
The Association of Fish and Wildlife Agencies (AFWA) Fish and Wildlife Health Committee [PDF – 2 pages]provides potential risk mitigation strategies for wildlife scientists, biologists, hunters, trappers, and wildlife control operators that come in direct contact with wildlife.
Wildlife Research and Management/Control Activities: Hierarchy of controls to lower the risk of the virus that causes COVID-19 spreading between people and wildlife
Elimination Controls
- N/A
Substitution Controls
- Substitute animal capture or close proximity with remote monitoring methods.
- For example, acoustic monitoring (for animals like bats), game cameras, or environmental sample collection (such as feces or hair) may be sufficient to replace capture and animal handling.
Engineering Controls
- Maintain a log of personnel that have conducted fieldwork that involves direct contact with wildlife that are known or suspected to be susceptible to the virus that causes COVID-19. At minimum, logs should include personnel names, date(s) of field activities, species they interacted with, and duration of interaction.
- Consider using flexible, non-punitive sick leave policies that help encourage sick employees to stay home.
- If animal capture or close contact is essential, select capture methods that maximize distance between people and wildlife and minimize the duration of time people are in direct contact with animals. For example, culvert traps can be used instead of snares for bear capture.
- Develop and adhere to a standard protocol for handling and sampling wild animals.
- Develop and institute training for personnel conducting fieldwork on risk mitigation measures that reduce the risk of transmission between people or people and wildlife.
Administrative Controls
- Recommend that all staff and volunteers get a COVID-19 vaccine.
- Follow public health recommendations to prevent getting sick and to protect others, including staying up to date with COVID-19 vaccines.
- Perform regular symptom and temperature checks of personnel and consider requiring COVID-19 testing before field work where direct contact with other personnel or wildlife is necessary.
- Limit the number of personnel to the minimum necessary to safely complete the task and minimize the number of personnel who have direct contact with wildlife.
- Maintain the same capture team for the duration of the operation to minimize the number of people contacting other people and animals.
- Keep animals separate from each other to the greatest extent possible during capture and handling.
- Clean and disinfect all field gear and equipment that may come in contact with wildlife before starting the work, between animals (if warranted), and after finishing the work.
Personal Protective Equipment (PPE)
- Follow appropriate guidance from the state public health and wildlife authorities, CDC, and the US Geological Survey (USGS)pdf [PDF – 34 pages]on the use of PPE when handling or working with susceptible wildlife.
- Wear PPE appropriate for the role and associated risk based on guidance from CDC and USGS to best protect the health of people and animals.
- If the animal being handled is suspected or known to be positive for the virus that causes COVID-19, or if there is a risk of aerosols being created by a task or procedure, wear a respirator to prevent nose and mouth exposure to respiratory droplets and sprays and to prevent inhalation of small particles.
- Respirator use should occur in the context of a complete respiratory protection program in accordance with OSHA Respiratory Protection standard (29 CFR 1910.134), which includes medical evaluations, training, and fit testing.
- N95 respirators with an exhalation valve and masks with vents should not be used when working with wildlife because they do not prevent the wearer’s droplets from being released into the immediate environment and may therefore expose animals being handled.
Considerations for Wildlife Rehabilitation Facilities
While wildlife rehabilitators should always follow permit conditions and implement general biosecurity measures in their facilities, it is essential that they follow additional precautionary measures, since the general stress in captured wildlife, prolonged interaction with humans during captivity, and the unknown health status of the public and other transporters bringing rescued wildlife to rehabilitation facilities may increase the risk of animal virus exposure and infection.
Developing Risk Mitigation Measures
In addition to using a Hierarchy of Controls approach to lower risk during the wildlife rehabilitation period, wildlife agencies working with their rehabilitators may consider developing criteria for release of any known or presumed susceptible wildlife. This should determine the animal’s basic fitness for independent survival in its native habitat, any risk of exposure to the virus, and if pre-release testing of the animal and/or its caretakers is warranted, practical, and/or feasible. Routine testing of animals for the virus that causes COVID-19 is not recommended. The decision to test an animal should be made collaboratively using a One Health approach between local, state, and/or federal public health and animal health officials.
Wildlife Rehabilitation Facilities: Hierarchy of Controls to Lower the Risk of the Virus that Causes COVID-19 Spreading between People and Wildlife
Elimination Controls
- N/A
Substitution Controls
- N/A
Engineering Controls
- Maintain a log of personnel that have direct contact with wildlife patients that are known or suspected to be susceptible to the virus that causes COVID-19. At minimum, logs should include personnel name, date(s) of contact, species they interacted with, and duration of interaction.
- Consider implementing flexible, non-punitive sick leave policies that help encourage sick employees to stay home.
- Follow CDC COVID-19 ventilation guidelines to improve ventilation in the facility.
- Minimize frequent human proximity to susceptible species by keeping patients of those species isolated in properly ventilated areas.
- Keep enclosures used for susceptible species as far apart as possible.The use of a solid barrier between enclosures (e.g., between open mesh style small cages) may also help to minimize transmission of virus through the air.
- Do not allow contact between wildlife, pests, and domestic animals and rehabilitation patients in outdoor cages; consider placement of a cover over cages or double fencing.
- Since the virus may be shed in feces, ensure regular removal of feces with proper disposal based on state/local ordinances.
- Use an EPA-listed disinfectant for use against the virus that causes COVID-19 on all non-disposable equipment used in the capture, handling, transport, rehabilitation, and husbandry of susceptible wildlife.
- Develop and institute training for personnel on measures that reduce the risk of transmission between people or people and wildlife patients.
Administrative Controls
- Recommend that all staff and volunteers get a COVID-19 vaccine.
- Follow public health recommendations to prevent getting sick and to protect others, including staying up to date with COVID-19 vaccines, improving ventilation, and getting tested for COVID-19 when needed.
- Develop and periodically update an emergency response plan to ensure continuity of operations during any type of emergency or disease outbreak. The plan should include contingencies for staff rotations or minimal dedicated staffing; animal care; food, water, and medical supplies; power and utilities supply; communications; and reporting human and animal health concerns to authorities. For COVID-19, this should include the facility policy for self-reporting of any COVID-19 positive staff and volunteers.
- Report to the state and/or federal wildlife agency any susceptible wildlife with possible exposure to a person with COVID-19, especially animals that are displaying clinical signs consistent with the virus that causes COVID-19.
- If possible, establish dedicated teams of staff and volunteers who work together in rotating work shifts (e.g., 1 week on /1 week off) to minimize the potential spread of COVID-19 between workers.
- Isolate animals with respiratory (coughing, sneezing, nasal discharge) or gastrointestinal signs (diarrhea, vomiting). Limit staff contact and use appropriate PPE. Contact a veterinarian to arrange care.
- Avoid unnecessary handling or other contact with susceptible species and limit the number of staff who handle members of these species.
- Implement a sequence for handling wildlife in rehabilitation:
- First: Handle or treat susceptible animals.
- Last: Handle or treat animals that have clinical signs of infection with the virus that causes COVID-19 in an isolated area.
- All other animals should be treated between these two groups, keeping in mind to handle younger animals before adult animals.
- Ideally, separate staff would be assigned to care for each group, or for limited staffing, handle/treat in the sequence listed.
- Pre-arrange backup caregivers for all animals undergoing rehabilitation.
- Follow guidelines in the NWRA/IWRC “Minimum Standards for Wildlife Rehabilitation, 4th edition [PDF – 128 pages]” to include daily cleaning and disinfection of the facility.
- Work with state wildlife health, animal health, and public health authorities to determine if samples should be collected from rehabilitated animals (if feasible) and submitted to designated veterinary diagnostic laboratories for testing.
- Have initial quarantine protocol and procedures in place for newly admitted patients as well as strict biosecurity protocols that can help to inform release criteria development.
- Conduct ‘just-in-time’ training for staff and volunteers on basic biosecurity principles and practices. At a minimum, those working in close contact with wildlife should understand potential risks and review the appropriate methods for donning and doffing PPE prior to working with the animals in rehabilitation facilities.
Personal Protective Equipment (PPE)
- Follow appropriate guidance from the state wildlife authority, CDC, and the US Geological Survey (USGS)pdf [PDF – 34 pages] on the use of PPE when handling or working with susceptible wildlife.
- Wear PPE appropriate for the role and associated risk based on guidance from CDC and other partners best protect the health of people and animals.
- If the animal being handled is suspected or known to be positive for the virus that causes COVID-19, or if there is a risk of aerosols being created by a task or procedure, wear a respirator to prevent nose and mouth exposure to droplets and sprays and to prevent inhalation of small particles.
- Respirator use should occur in the context of a complete respiratory protection program in accordance with OSHA Respiratory Protection standard (29 CFR 1910.134), which includes medical evaluations, training, and fit testing.
- N95 respirators with an exhalation valve and masks with vents should not be used when working with wildlife because they do not prevent the wearer’s droplets from being released into the immediate environment and may, therefore, expose animals being handled.
Federal Resources
- CDC: COVID-19 and Animals
- CDC: Evaluation for SARS-CoV-2 Testing in Animals
- USGS: Field Manual of Wildlife Diseases
- USGS: Assessing the Risks Posed by SARS-CoV-2 in and via North American Bats—Decision Framing and Rapid Risk Assessment [PDF – 54 pages]
Professional Organization Resources
- American Veterinary Medical Association: Disaster Preparedness Resources
- American Association of Wildlife Veterinarians: https://aawv.net/coronavirus-pandemic
- Association of Fish and Wildlife Agencies: COVID-19 and North American Species of Mustelidae, Felidae, and Canidae [PDF – 2 pages]
- IUCN: Guidelines for Working with Free-Ranging Wild Mammals in the Era of the COVID-19 Pandemic
- IUCN SSC Bat Specialist Group: recommendations to reduce the risk of transmission of SARS-CoV-2 from humans to bats in bat rescue and rehabilitation centers
- IUCN SSC Bat Specialist Group: Recommended Strategy for Researchers to Reduce the Risk of Transmission of SARS-CoV-2 from Humans to Bats
- The National Association of State Public Health Veterinarians: Compendium of Veterinary Standard Precautions for Zoonotic Disease Prevention in Veterinary Personnel [PDF – 27 pages]
- National Wildlife Rehabilitators Association: Home Page
- Wildlife Disease Association: COVID-19 Information
- Wildlife Health Australia: Bat Health Focus Group
- Zoo and Aquarium All Hazards Preparedness, Response, and Recovery (ZAHP) Fusion Center: Considerations for the management of non-domestic species in human care during COVID-19