Reduce Risk from Water
From Plumbing to Patients
Water is the foundation of life; because of that, wet environments pose a particular hazard of infection, promoting microbial growth and serving as a source for antibiotic resistant pathogens, and healthcare-associated infections.
Tap water meets stringent safety standards in the United States, but it is not sterile. Certain numbers and types of bacteria and other microbes may be present when water leaves the tap. For typical household uses such as washing, bathing, drinking and food preparation, these microbes rarely pose a serious health risk.
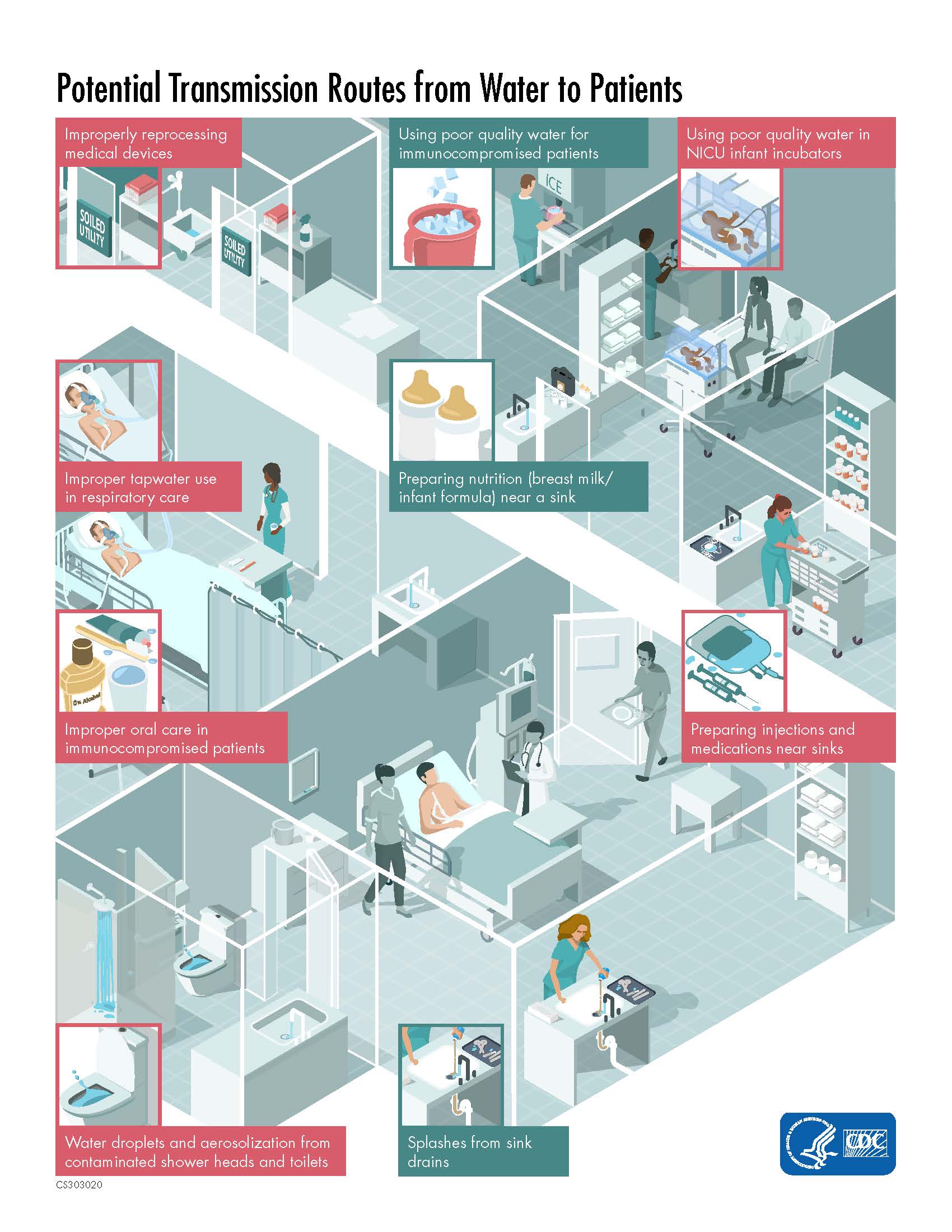
In contrast, in healthcare settings, the ways we use water are more varied and patients might be more vulnerable to infection. Certain conditions within healthcare plumbing systems can even encourage microbial growth. This can lead to dangerously high levels of potential pathogens. Moreover, the risk does not stop at the tap—every use of water in patient care settings must be scrutinized and evaluated for its risk to harbor and transmit healthcare-associated pathogens. Even hospital sink drains and toilets can pose a risk for harboring antibiotic resistant pathogens that can spread to patients and cause harm.
Water can harbor germs that threaten the safety of patients and spread antibiotic resistant pathogens or healthcare-associated infections (HAIs). Water management programs in healthcare facilities are an important way to help protect vulnerable patient populations as well as staff and visitors.
Patient safety depends on assuring that:
- Water entering a healthcare facility meets all applicable quality standards
- Premise plumbing (i.e. a building’s hot and cold water piping systems) is designed and maintained in a way that minimizes growth and spread of waterborne pathogens in both the supply and waste sides
- Exposure to infection risks from water sources is minimized
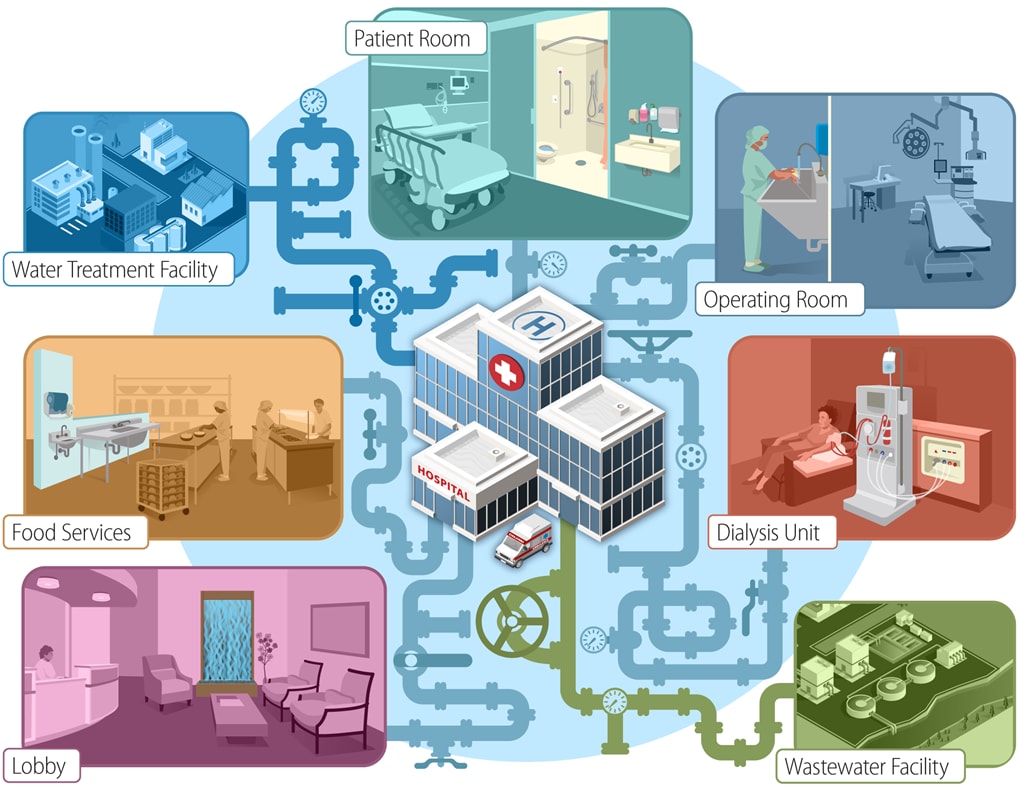
Healthcare facilities can have large complex water systems that promote growth of pathogenic organisms if not properly maintained. For this reason, the Centers for Medicare & Medicaid Services (CMS) and CDC consider it essential that hospitals and nursing homes have a water management program that is effective in limiting Legionella and other opportunistic pathogens of premise plumbing from growing and spreading in their facility.
A healthcare water management program identifies both hazardous conditions and corrective actions that can minimize the growth and spread of waterborne pathogens. Programs such as Developing a Water Management Program to Reduce Legionella Growth and Spread in Buildings: A Practical Guide to Implementing Industry Standards 13.2 are designed, implemented, and regularly reviewed by multidisciplinary teams that include facility managers, infection prevention professionals, clinicians, and administrators.
On the “upstream” side, system disruptions or pressure drops, loss of disinfection residual (e.g. low chlorine levels), and main breaks are all factors that can impact the quality of water within a healthcare system. Thus, engagement with representatives from the local water utility is encouraged; hospitals and healthcare systems are often among a water utility’s largest customers. Water utilities represent important stakeholders in the effort to assure patient safety.
Similarly, moving “midstream,” water management programs should carefully assess their facility’s premise plumbing. This includes examining factors such as: the age and overall design of the system; additions, renovations and other modifications; water age (i.e. how long water might be held in the piping system); and assuring that there are no ‘dead ends’ where water can stagnate.
Finally, when focusing “downstream,” water management programs should consider the various pathways that might lead to patients becoming exposed to waterborne pathogens, in relation to ingestion, diet, hygiene, and clinical care. This is particularly important for patient populations whose ‘immune system might be compromised as a result of an underlying condition (e.g., cancer patients, premature infants) or in relation to invasive procedures such as surgery or the use of medical devices.
Recent evidence indicates sinks and other drains, such as toilets or hoppers, in healthcare facilities can become contaminated with multidrug-resistant organisms (MDROs). These pathogens can stick to the pipes to form biofilms, which allow the organisms to persist in drains for long periods of time and are often difficult to impossible to fully remove. Because different types of bacteria may contaminate the same drain, drains can serve as sites where antibiotic resistant genes are transferred between bacterial species.
Patients may be exposed to organisms in drains when water splashes from the drain. Splashes may occur when water flow hits the contaminated drain cover or when a toilet or hopper is flushed. Splashes can lead to dissemination of MDRO-containing droplets, which in turn may contaminate the local environment or the skin of nearby healthcare personnel and patients.
- Water Infection Control Risk Assessment (WICRA) for Healthcare Settings [PDF – 5 pages]
- Tap Water Quality and Infrastructure Discussion Guide for Investigation of Potential Water-Associated Infections in Healthcare Facilities [PDF – 5 pages]
- Healthcare Facility Water Management Program Checklist [PDF – 4 pages]
- Infection Control Assessment Tools
The following measures can reduce the risk of these events from occurring in healthcare facilities:
- Clean and disinfect surfaces near the drain, including the sink basin, faucet, faucet handles, and surrounding counter top at least daily.
- Avoid placement of patient care items or personal items on counters next to sinks. While assuring that handwashing sinks are located close by and accessible to personnel responsible for preparing patient medications, avoid locating sinks adjacent to medication preparation areas unless barriers are in place to prevent splashing in medication preparation areas.
- Prevent faucets from discharging directly above the drain as this causes splashing (i.e., angle water away from the drain or offset the faucet from the drain). When installing new sinks, consider selecting designs that prevent splashing. (Reference FGI Guideline for Hospitals A2.1-8.4.3.2 (1) a.)
- Use sinks in patient care areas with adequate depth and the maximum water flow as regulated to prevent splashing (FGI Guideline for Hospitals A2.1-8.4.3.2 (1) a., b., c. and A2.1-8.4.3.2 (2) (5), (6) and Gestrich, Donskey et al ICHE 2018 A multicenter investigation to characterize the risk for pathogen transmission from healthcare facility sinks.)
- Install and utilize hopper and toilet covers. These covers should be closed before flushing. If such covers are not available or are prohibited due to local plumbing or building code, close any door that separates the hopper or toilet from other patient care areas before flushing to contain any resulting environmental contamination. (Reference Mathers et al. Clinical Infectious Diseases 2018 Intensive Care Unit Wastewater Interventions to Prevent Transmission of Multispecies Klebsiella pneumoniae Carbapenemase-Producing Organisms.)
- Do not discard patient waste down sinks and minimize discarding liquid nutritional supplements or other beverages down sinks or toilets.
Multiple interventions have been attempted to reduce the burden of pathogens in contaminated drains. In general, biofilms are difficult to completely remove despite chemical interventions; EPA recently approved products to clean and disinfect bacteria in healthcare facility wastewater drain biofilms. Some chemical interventions may reduce the amount of contaminated splashing that may occur from the drains and may have been useful in responding to outbreaks, but the most appropriate method remains unclear (The Hospital Water Environment as a Reservoir for Carbapenem-Resistant Organisms Causing Hospital-Acquired Infections-A Systematic Review of the Literature.)
Research
At the intersection of research and innovation, the Division of Healthcare Quality Promotion (DHQP) researchers have designed and built a dedicated sink gallery for further defined study of intentionally contaminated plumbing to develop sampling schemes and understand factors affecting persistence, biofilm development, and remediation.
Collaboration is essential to advance public health research. DHQP areas of study include:
DHQP is collaborating with the University of Virginia Health System to study dispersal mechanisms from contaminated sinks. Results of this study, Droplet- Rather than Aerosol-Mediated Dispersion Is the Primary Mechanism of Bacterial Transmission from Contaminated Hand-Washing Sink Traps, suggest that microorganisms will disperse from contaminated sink bowl and drain surfaces primarily as large droplets that are generated during faucet usage.
DHQP-funded research has demonstrated that carbapenemase-producing strains of bacteria will colonize microbial biofilm communities in laboratory model systems simulating a sink drain P-trap (a section of pipe that holds water). These antibiotic-resistant organisms do not appear to amplify unless supplemented with liquid wastes containing microbial nutrients, including but not limited to soft drink products, intravenous fluids, or nutritional shakes.
DHQP researchers study non-traditional treatment strategies for the remediation of resistant organisms in contaminated handwashing sinks and plumbing systems in healthcare facilities involving use of lytic bacteriophages (bacterial viruses) with or without nonionic surfactants.
DHQP researchers are collaborating with the University of Utah on a research study to elucidate variables most critical to survival and amplification of antimicrobial resistant-gram negative bacteria and healthcare-associated pathogens in the healthcare environment.
- Pseudomonas aeruginosa
- Pseudomonas putida-P. fluorescens
- Burkholderia cepcia complex (B. cepacia, B. cenocepacia, at least 8 other genomospecies)
- Cupriavidus (Ralstonia) pauculus
- Herbaspirillium
- Methylobacterium spp
- Ralstonia pickettii, Ralstonia mannitolilytica
- Sphingomonas paucimobilis, Sphingomonas mucosissima, other Sphingomonas spp
- Stenotrophomonas maltophilia
- Acinetobacter baumannii, complex A. calcoaceticus
- Alcaligenes xylosoxidans, A. faecalis
- Aeromonas hydrophila, Aeromonas spp
- Elizabethkingia anophelis, E. meningosepticum
- Legionella pneumophila
- Enterobacter cloacae
- Klebsiella spp
- Pantoae aggloerans
- Rahnella aquatilis
- Serratia liquifaciens, Serratia marcescens
- Mycobacterium. abscessus clade (M. abscessus, M. bolettii, M. massiliense)
- M. chelonae
- M. mucogenicum clade (M. mucogenicum, M. phociacum)
- M. fortuitum clade (M. fortuitum, M. cosmeticum, mageritiense, M. porcinum, M. septicum)
- M. immunogenum
- M. smegmatis clade (M. goodii, M. wolinskyi)
- M. aurum
- M. simiae
- M. avium complex (M. avium, M. intracellulare, M. chimaera, M avium ss hominissuis, M. columbiense)
- M. scrofulacuemA. calcoaceticus
- M parascrofulaceum
- M. xenopi
- M. arupense
- M. kansasii
- M. haemophilum
- M. nonchromogenicum clade (M. nonchromogenicum, M. triviale, M. terrae)
- M. gordonae (only among patients with severe immune deficiency)
- Microbacterium spp
- Tsukamurella spp
- Rhodococcus equi, Rhodococcus spp
- Gordonae spp
- Yeasts (eg. Candida parapsilosis, C. tropicalis)
- Aspergillus fumigatus, A. niger
- Fusarium spp
- Exophiala spp
- Acanthamoeba spp
- Vermamoeba vermiformis
- Naegleria spp
Further Reading
Commentary and International Guidance
Arduino MJ. Tap Water Avoidance Decreases Rates of Hospital-onset Pulmonary Nontuberculous Mycobacteria: A Call for Water Management in Healthcare. Clin Infect Dis. 2021;73(3):528-530.
Bartram J, Cotruvo J, Exner M, Fricker C, Glasmacher A. Heterotrophic plate count measurement in drinking water safety management: Report of an Expert Meeting Geneva, 24–25 April 2002. Int J Food Microbiol 2004; 92(3):241-7
Department of Health. Health Technical Memorandum 04-01: Safe water in Healthcare Premises, Part A-Design, installation and Commissioning [PDF – 94 pages], Crown Publishing, The National Archives, Kew, London, UK, 2016
Department of Health. Health Technical Memorandum 04-0, Part B- Operational Management [PDF – 98 pages], Crown Publishing, The National Archives, Kew, London, UK, 2016
Department of Health. Health Technical Memorandum 04-01, Part C: Pseudomonas aeruginosa, advice for augmented care units [PDF – 20 pages], Crown Publishing, The National Archives, Kew, London, UK, 2016
SAC. Guidelines for the Prevention and Control of Infection from Water Systems in Healthcare Facilities [PDF – 100 pages], Health Protection Surveillance Centre, Health Service Executive, Dublin, Ireland, 2017
WHO. Water safety in buildings [PDF – 164 pages], WHO, Geneva, 2011.
Sinks, Drains and Wastewater
Carlin PC. Wastewater drains: epidemiology and interventions in 23 carbapenem-resistant organism outbreaks. Infect Control Hosp Epi 2018; ahead of print; doi:10.1017/ice.2018.18.
Constantinides B, Chau KK, Quan TP, Rodger G, Andersson MI, Jeffery K, Lipworth S, Gweon HS, Peniket A, Pike G, Millo J, Byukusenge M, Holdaway M, Gibbons C, Mathers AJ, Crook DW, Peto TEA, Walker AS, Stoesser N. Genomic surveillance of Escherichia coli and Klebsiella spp. in hospital sink drains and patients. Microb Genom. 2020 Jul;6(7):mgen000391. doi: 10.1099/mgen.0.000391. PMID: 32553019; PMCID: PMC7478627.
Decraene, V., Phan, H. T. T., George, R., et al. A Large, Refractory Nosocomial Outbreak of Klebsiella pneumoniae Carbapenemase-Producing Escherichia coli Demonstrates Carbapenemase Gene Outbreaks Involving Sink Sites Require Novel Approaches to Infection Control. American Society for Microbiology. 2018; 62(12). https://doi.org/10.1128/AAC.01689-18
Heireman L, Hamerlinck H, Vandendriessche S, Boelens J, Coorevits L, de Brabandere E, et al. Toilet drain water as a potential source of hospital room-to-room transmission of carbapenemase-producing Klebsiella pneumoniae. J Hosp Infect 2020; 106(2):232-9
Hopman J, Tostmann A, Wertheim H, Bos M, et al. Reduced rate of intensive care unit acquired gram-negative bacilli after removal of sinks and introduction of ‘water-free’ patient care. Antimicrob Resist Infect Control 2017;6:59.
Mathers AJ, Vegesana K, German Mesner I, Barry KE, Pannone A, Baumann J, Crook DW, Stoesser N, Kotay S, Carroll J, Sifri CD. Intensive Care Unit Wastewater Interventions to Prevent Transmission of Multispecies Klebsiella pneumoniae Carbapenemase-Producing Organisms. Clin Infect Dis. 2018 Jul 2;67(2):171-178. doi: 10.1093/cid/ciy052. PMID: 29409044.
Park SC, Parikh H, Vegesana K, Stoesser N, Barry KE, Kotay SM, Dudley S, Peto TEA, Crook DW, Walker AS, Mathers AJ. Risk Factors Associated with Carbapenemase-Producing Enterobacterales (CPE) Positivity in the Hospital Wastewater Environment. Appl Environ Microbiol. 2020 Nov 24;86(24):e01715-20. doi: 10.1128/AEM.01715-20. PMID: 32917755; PMCID: PMC7688209.
Shaw E, Gavaldà L, Càmara J, Gasull R, Gallego S, et al. Control of endemic multidrug-resistant Gram-negative bacteria after removal of sinks and implementing a new water-safe policy in an intensive care unit. J Hosp Infect. 2018;98(3):275-281. doi: 10.1016/j.jhin.2017.10.025.
Volling, C., Ahangari, N., Bartoszko, J. J., et al. (2020). Are Sink Drainage Systems a Reservoir for Hospital-Acquired Gammaproteobacteria Colonization and Infection? A Systematic Review. Open forum infectious diseases, 8(2), ofaa590. https://doi.org/10.1093/ofid/ofaa590
Weinbren M, Inkster T, Lafferty F. Drains and the periphery of the water system – what do you do when the guidance is outdated? Infect Prev Pract 2021;3(4):100179
Weingarten, R., Johnson, R. C., Conlan, S. et al. Genomic Analysis of Hospital Plumbing Reveals Diverse Reservoir of Bacterial Plasmids Conferring Carbapenem Resistance. mBio. 2018;9(1). https://doi.org/10.1128/mBio.02011-17
Healthcare Water Management
Meeting water quality standards, limiting infection risks from water sources, and designing and maintaining premise plumbing to minimize the growth and spread of pathogens are vital components of a water management program. </p>
The following resources provide examples of the role of waterborne pathogens in healthcare.
- Baker AW, Stout JE, Anderson DJ, Sexton DJ, Smith B, Moehring RW, Huslage K, Hostler CJ, Lewis SS. Tap Water Avoidance Decreases Rates of Hospital-onset Pulmonary Nontuberculous Mycobacteria. Clin Infect Dis. 2021;73(3):524-527
- Bancroft J, Shih D, Cassidy PM, et al. (2018). Standardized case definition for extrapulmonary nontuberculous mycobacteria infections [PDF – 13 pages]. Council of State and Territorial Epidemiologists, April 2018,
- Bédard E, Prévost M, Déziel E. Pseudomonas aeruginosa in premise plumbing of large buildings [PDF – 20 pages] Microbiology Open 2016;5(6):937-956.
- Center for Clinical Standards and Quality/Survey & Certification Group, Centers for Medicare & Medicaid Services (June 9, 2017). Requirement to Reduce Legionella Risk in Healthcare Facility Water Systems to Prevent Cases and Outbreaks of Legionnaires’ Disease (LD) [Memorandum] [PDF – 4 pages].
- Crist MB, Perz JF. Modern healthcare versus nontuberculous mycobacteria: Who will have the upper hand? [PDF – 4 pages] Clin Infect Dis 2017;64(7):912-913.
- Danila RN, Koranteng N, Como-Sabetti KJ, Robinson TJ, Laine ES. Hospital water management programs for Legionella prevention, Minnesota, 2017. Infect Control Hosp Epidemiol 2018; 39:336-8.
- Decker BK, Palmore TN. The role of water in healthcare-associated infections [PDF – 13 pages] Current opinion in infectious diseases 2013;26:345-51.
- Dyck A, Exner M, Kramer A. Experimental based experiences with the introduction of a water safety plan for a multi-located university clinic and its efficacy according to WHO recommendations. BMC Public Health. 2007;7:34.
- Edwards M, Rhoads W, Pruden A, Pearce A, Falkinham JO. Green water systems and opportunistic premise plumbing pathogens. Plumb Eng 2014; 42:63-5.
- Ehret KM, Chamberlain AT, Berkelman RL, Fridkin SK. Preventing hospital-acquired Legionnaires’ disease: A snapshot of clinical practices and water management approaches in US acute-care hospitals. Infect Control Hosp Epidemiol 2018; 39(12):1470-1472.
- Falkinham JO III, Hillborn ED, Arduino MJ, Pruden A, Edwards MA. Epidemiology and ecology of opportunistic premise plumbing pathogens: Legionella pneumophila, Mycobacaterium avium, and Pseudomonas aeruginosa. Environ Health Perspect 2015; 123:749-58.
- Gamage SD, Ambrose M, Kralovic SM, Roselle GA. Water Safety and Health Care: Preventing Infections Caused by Opportunistic Premise Plumbing Pathogens. Infect Dis Clin North Am. 2021;35(3):667-695. https://doi.org/10.1016/j.idc.2021.04.007
- Geldrich E. Drinking water microbiology—new directions toward water quality enhancement. Int J food Microbiol 1989;9(4)295-312.
- Griffith C. HACCP and the management of healthcare associated infections: Are there lessons to be learnt from other industries? Int J Health Care Quality Assurance 2006;19(04):351-367.
- Hanlin JH, Myers ER. Healthcare plumbing systems are sources and vectors of infection for HAIs. Infection Control Today, March 1 2018.
- Henkle E, Hedberg K, Schafer SD, Winthop KL. Surveillance of Extrapulmonary Nontuberculous Mycobacteria Infections, Oregon, USA, 2007-2012 [PDF – 4 pages]. Emerg Infect Dis. 2017;23(10):1627-1630
- Inkster T, Wilson G, Black J, Mallon J, Connor M, Weinbren M. Cupriavidus spp and other waterborne organisms in healthcare water systems across the United Kingdom. J Hosp Infect. 2022 Feb 15:S0195-6701(22)00043-3. https://doi.org/10.1016/j.jhin.2022.02.003
- Kizny Gordon AE, Mathers AJ, Cheong EYL, et al. The hospital water environment as a reservoir for carbapenem-resistant organisms causing hospital-acquired infections – a systematic review of the literature. CID 2017; 64:1435-44.
- Krageschmidt DA, Kubly AF, Browning MS, et al. A comprehensive water management program for multicampus healthcare facilities. Infect Control Hosp Epidemiol 2014; 35:556-63.
- Lefebvre, A., Bertrand, X., Quantin, C., Vanhems, P., Lucet, J.-C., Nuemi, G., Astruc, V., Chavanet, P., Aho-Glélé, L.S. Association between Pseudomonas aeruginosa positive water samples and healthcare-associated cases: nine-year study at one university hospital. Journal of Hospital Infection. Volume 96, Issue 3. 2017. Pages 238-243. ISSN 0195-6701. https://doi.org/10.1016/j.jhin.2016.12.007.
- Li T, Abebe LS, Cronk R, Bartram J. A systematic review of waterborne infections from nontuberculous mycobacteria in health care facility water systems. Int J Hygiene Environ Health 2017; 220:611-20.
- Moffa M, Guo W, Li T, Cronk R, Abebe LS, Bartram J. A systematic review of nosocomial waterborne infections in neonates and mothers. Int J Hyg Environ Health 2017;220(8):1199-1206. doi: 10.1016/j.ijheh.2017.07.011.
- Rizzo K, Rosenberg J, Kim J. Water management program implementation in California hospitals following the Centers for Medicare and Medicaid Services requirement. Am J Infect Control. 2020;48(11):1399-1401. doi: 10.1016/j.ajic.2020.04.017
- Scanlon MM, Gordon JL, McCoy WF, Cain MF. Water Management for Construction: Evidence for Risk Characterization in Community and Healthcare Settings: A Systematic Review. Int J Environ Res Public Health. 2020 17(6):2168
- Shih DC, Cassidy PM, Perkins KM, Crist MB, Cieslak PR, Leman RL. Extrapulmonary nontuberculous mycobacterial disease surveillance – Oregon, 2014-2016. MMWR Morb Mortal Wkly Rep 2018; 67:854-7.
- Sood G, Parrish N. Outbreaks of nontuberculous mycobacteria. Curr Opin Infect Dis. 2017 Aug;30(4):404-409.
- Weinbren M, Inkster T. The hospital-built environment: biofilm, biodiversity and bias. J Hosp Infect 2021;111:50-52. doi:10.1016/j.jhin.2021.02.013
- Winthrop KL, Henkle E, Walker A, Cassidy M, Hedberg K, Schafer S. On the reportability of nontuberculous mycobacterial disease to public health authorities [PDF – 4 pages]. Ann Am Thorac Soc 2017; 14:314-7.
Outbreaks Involving Waterborne Pathogens
Outbreaks involving waterborne pathogens are one of the more common types of consultation requests that CDC/DHQP receives. The following resources provide examples of review papers, commentaries, and outbreak investigation summaries.
- Andrews V, Hasman H, Midttun M, Feldthaus MB, et al. A hospital outbreak of an NDM-producing ST167 Escherichia coli with a possible link to a toilet. J Hosp Infect 2021;117:186-187. doi: 10.1016/j.jhin.2021.08.023.
- Baker AW, Lewis SS, Alexander BD, et al. Two-phase hospital-associated outbreak of Mycobacterium abscessus: investigation and mitigation Clin Infect Dis 2017; 64(7):902-911.
- Beer KD, Gargano JW, Roberts VA, et al. Surveillance for waterborne disease outbreaks associated with drinking water—United States 2011-2012. MMWR Morb Mortal Wkly Rep 2015; 64(31):842-8.
- Block C, Ergaz-Shaltiel Z, Valinsky L, et al. Déjà vu: Ralstonia mannitolilytica infection associated with a humidifying respiratory therapy device, Israel, June to July 2011. Euro Surveill 2013; 18:20471.
- Brooks RB, Mitchell PK, Miller JR, et al. Multistate outbreak of Burkholderia cepacia complex bloodstream infections after exposure to contaminated saline flush syringes – United States, 2016—2017. CID 2018; Epub ahead of print.
- Brown-Elliott BA, Wallace RJ Jr, Tichindelean C. Five-year outbreak of community- and hospital-acquired Mycobacterium porcinum infections related to public water supplies J Clin Microbiol 2011; 49(12):4231-8.
- Catho G, Martischang R, Boroli F, Chraïti MN, et al. Outbreak of Pseudomonas aeruginosa producing VIM carbapenemase in an intensive care unit and its termination by implementation of waterless patient care. Crit Care 2021;19;25(1):301.
- CDC. Nosocomial Infection and Pseudoinfection from contaminated endoscopes and bronchoscopes – Wisconsin and Missouri MMWR Morb Mortal Wkly Rep 1991; 40(39);675-678.
- Conger NG, O’Connell RJ, Laurel VL, et al. Mycobacterium simae outbreak associated with a hospital water supply. Infect Control Hosp Epidemiol 2004; 25(12):1050-5.
- Edens C, Liebich L, Halpin AL, et al. Mycobacterium chelonae eye infections associated with humidifier use in an outpatient LASIK clinic–Ohio, 2015 MMWR Morb Mortal Wkly Rep 2015; 64(41):1177.
- Glowicz J, Crist M, Gould C, et al. A multistate investigation of healthcare-associated Burkholderia cepacia complex infections related to liquid docusate sodium contamination, January—October 2016 [PDF – 14 pages]. Am J Infect Control 2018; 45:649-55.
- Haller S, Höller C, Jacobshagen A, et al. Contamination during production of heater-cooler units by Mycobacterium chimaera potential cause for invasive cardiovascular infections: results of an outbreak investigation in Germany, April 2015 to February 2016. Euro Surveill 2016; 21:30215.
- Hatzenbuehler LA, Tobin-D’Angelo M, Drenzek C, et al. Pediatric dental clinic-associated outbreak of Mycobacterium abscessus J Pediatric Infect Dis Soc 2017; 6:e116-22.
- Inkster T, Peters C, Wafer T, Holloway D, Makin T. Investigation and control of an outbreak due to a contaminated hospital water system, identified following a rare case of Cupriavidus pauculus bacteraemia. J Hosp Infect 2021; 111:53-64
- Jhung MA, Sunenshine RH, Noble-Wang J, et al. A national outbreak of Ralstonia mannitolilytica associated with use of a contaminated oxygen-delivery device among pediatric patients. Pediatrics 2007; 119:1061-8.
- Johnson RC, Deming C, Conlan S, Zellmer CJ, Michelin AV, Lee-Lin S, Thomas PJ, Park M, Weingarten RA, Less J, Dekker JP. Investigation of a Cluster of Sphingomonas koreensis New Engl J Med 2018; 379(26):2529-39.
- Kanamori H, Weber DJ, Rutala WA. Healthcare outbreaks associated with a water reservoir and infection prevention strategies. CID 2016; 62:1423-35.
- Kinsey CB, Koirala S, Solomon B, et al. Pseudomonas aeruginosa outbreak in a neonatal intensive care unit attributed to hospital tap water Infect Control Hospital Epidemiol 2017; 38(7):801-808.
- Lee YL, Liu KM, Chang HL, Lin JS, Kung FY, Ho CM, Lin KH, Chen YT. A dominant strain of Elizabethkingia anophelis emerged from a hospital water system to cause a three-year outbreak in a respiratory care center. J Hosp Infect 2021;108:43-51.
- Loveday HP, Wilson JA, Kerr K, Pitchers R, Walker JT, Browne J. Association between healthcare water systems and Pseudomonas aeruginosa infections: a rapid systematic review J Hosp Infect 2014;86(1):7-15.
- Mainciu A, Popa M, Mitrea D, Căpăţînă D. Parameters Monitoring Solutions for the Quality Control of Water Used in Healthcare Units [PDF – 6 pages]. In 2006 IEEE International Conference on Automation, Quality and Testing, Robotics 2006 May 25 (Vol. 2, pp. 457-462). IEEE.
- Marra AR, Diekema DJ, Edmond MB. Mycobacterium chimaera infections associated with contaminated heater-cooler devices for cardiac surgery: outbreak management. CID 2017; 65:669-74.
- McCoy WF, Rosenblatt AA. HACCP-Based Programs for Preventing Disease and Injury from Premise Plumbing: A Building Consensus [PDF – 6 pages]. Pathogens 2015;4(3):513-528.
- Moore LS, Owens DS, Jepson A, et al. Waterborne Elizabethkingia meningoseptica in adult critical care Emerg Infect Dis 2016;22(1):9-17.
- Peralta G, Tobin-D’Angelo M, Parham A, et al. Notes from the Field. Mycobacterium abscessus infections among patients of a pediatric dentistry practice — Georgia, 2015 MMWR Morb Mortal Wkly Rep 2016; 65:355–356.
- Singh J, O’Donnell K, Nieves DJ, Adler-Shohet FC, et al. Invasive Mycobacterium abscessus Outbreak at a Pediatric Dental Clinic. Open Forum Infect Dis. 2021;8(6):ofab165
- Tofteland S, Naseer U, Lislevand JH, Sundsfjord A, Samuelsen O. A long-term low-frequency hospital outbreak of KPC-producing Klebsiella pneumoniae involving intergenus plasmid diffusion and a persisting environmental reservoir. PLoS One 2013; 8(3):e59015.
- Williams MM, Armbruster CR, Arduino MJ. Plumbing of hospital premises is a reservoir for opportunistically pathogenic microorganisms: a review Biofouling 2013;29:147-62.
- Yung CF, Maiwald M, Loo LH, Soong HY, Tan CB, et al. Elizabethkingia anophelis and Association with Tap Water and Handwashing, Singapore. Emerg Infect Dis 2018;24(9):1730-1733