Vancomycin-resistant Enterococci (VRE) in Healthcare Settings
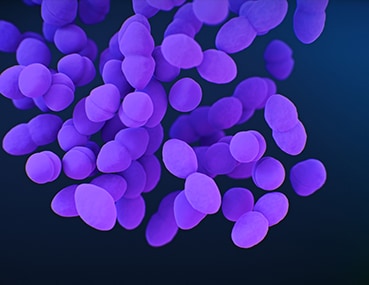
Enterococci are bacteria (germs) that are normally present in the human intestines and in the female genital tract, and are often found in the environment, like in soil and water. These bacteria can cause infections.
See CDC’s report
Antibiotic Resistance Threats in the United States, 2019
Enterococci bacteria are constantly finding new ways to avoid the effects of the antibiotics used to treat the infections they cause. Antibiotic resistance occurs when the germs no longer respond to the antibiotics designed to kill them. If these germs develop resistance to vancomycin, an antibiotic that is used to treat some drug-resistant infections, they become vancomycin-resistant enterococci (VRE).
How common are these infections?
In 2017, VRE caused an estimated 54,500 infections among hospitalized patients and 5,400 estimated deaths in the United States [Source: 2019 AR Threats Report].
Who is at risk?
Those most likely to be infected include:
- people who have been previously treated with antibiotics, including vancomycin, for long periods of time
- people who are hospitalized, have undergone surgical procedures, or have medical devices inserted in their bodies (such as catheters)
- people with weakened immune systems, such as patients in intensive care units, or in cancer or transplant wards
How is it spread?
VRE can spread from one person to another through contact with contaminated surfaces or equipment or through person to person spread, often via contaminated hands. It is not spread through the air by coughing or sneezing.
How can you avoid getting an infection?
If you or someone in your household has VRE, you can protect yourself by:
- keeping your hands clean to avoid getting sick and spreading germs that can cause infections
- patients and their caregivers should wash their hands with soap and water or use alcohol-based hand sanitizer, particularly:
- after using the bathroom
- before and after handling medical devices or caring for wounds
- before preparing food
- patients and their caregivers should wash their hands with soap and water or use alcohol-based hand sanitizer, particularly:
- frequently cleaning areas of the home, such as bathrooms, that may become contaminated with VRE
- wearing gloves if hands may come in contact with body fluids that may contain VRE, such as stool (poop) or bandages from infected wounds
- Always wash your hands after removing gloves.
- informing healthcare providers if you or someone you care for has VRE so that appropriate precautions can be taken to prevent spread
How are these infections treated?
When VRE infections do develop, they are generally treated with antibiotics other than vancomycin. In order to identify the best antibiotic to treat a specific infection, healthcare providers will send a specimen (often called a culture) to the laboratory and test any bacteria that grow against a set of antibiotics to determine which are active against the germ. The provider will then select an antibiotic based on the activity of the antibiotic and other factors like potential side effects or interactions with other drugs.
Some people will carry VRE on their body without it causing symptoms, which is called being colonized. People who are colonized do not require antibiotics.
What is CDC doing to address VRE infections?
CDC tracks VRE infections using data from several sources, including the National Healthcare Safety Network Patient Safety Component. This surveillance system collects reports of VRE from device-associated infections, such as central-line associated bloodstream infections.
CDC works with healthcare facilities and state and local health departments to control outbreaks of resistant germs like VRE and to help devise and implement prevention strategies for facilities with high numbers of VRE infections.