Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Assisted Reproductive Technology Surveillance — United States, 2010
Corresponding author: Saswati Sunderam, PhD, Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. Telephone: 770-488-6356; E-mail: zga0@cdc.gov.
Abstract
Problem/Condition: Since the first U.S. infant conceived with Assisted Reproductive Technology (ART) was born in 1981, both the use of advanced technologies to overcome infertility and the number of fertility clinics providing ART services have increased steadily in the United States. ART includes fertility treatments in which both eggs and sperm are handled in the laboratory (i.e., in vitro fertilization [IVF] and related procedures). Women who undergo ART procedures are more likely to deliver multiple-birth infants than those who conceive naturally because more than one embryo might be transferred during a procedure. Multiple births pose substantial risks to both mothers and infants, including pregnancy complications, preterm delivery, and low birthweight infants. This report provides state-specific information on U.S. ART procedures performed in 2010 and compares infant outcomes that occurred in 2010 (resulting from procedures performed in 2009 and 2010) with outcomes for all infants born in the United States in 2010.
Reporting Period Covered: 2010.
Description of System: In 1996, CDC began collecting data on all ART procedures performed in fertility clinics in the United States and U.S. territories, as mandated by the Fertility Clinic Success Rate and Certification Act of 1992 (FCSRCA) (Public Law 102-493). Data are collected through the National ART Surveillance System (NASS), a web-based data collecting system developed by CDC.
Results: In 2010, a total of 147,260 ART procedures performed in 443 U.S. fertility clinics were reported to CDC. These procedures resulted in 47,090 live-birth deliveries and 61,564 infants. The largest numbers of ART procedures were performed among residents of six states: California (18,524), New York (excluding New York City) (14,212), Illinois (10,110), Massachusetts (9,854), New Jersey (8,783), and Texas (8,754). These six states also had the highest number of live-birth deliveries as a result of ART procedures and together accounted for 48.0% of all ART procedures performed, 45.0% of all infants born from ART, and 45.0% of all multiple live-birth deliveries but only 34.0% of all infants born in the United States and U.S. territories. Nationally, the average number of ART procedures performed per 1 million women of reproductive age (15–44 years), which is a proxy indicator of ART use, was 2,331. In 13 states (California, Connecticut, Delaware, Hawaii, Illinois, Maryland, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Virginia), this proxy measure was higher than the national rate, and in four states (Connecticut, Massachusetts, New Jersey, and New York) and the District of Columbia, it exceeded twice the national rate. Nationally, among cycles in which at least one embryo was transferred, the average number of embryos transferred increased with increasing age (2.0 among women aged <35 years, 2.4 among women aged 35–40 years, and 3.0 among women aged >40 years). Elective single-embryo transfer (eSET) rates decreased with increasing age (10.0% among women aged <35 years, 3.8% among women aged 35–40 years, and 0.6% among women aged >40 years). ESET rates also varied substantially between states (range: 0 to 45.0% among women aged <35 years).
The number of ART births as a percentage of total infants born in the state or territory is considered as another measure of ART use. Overall, ART contributed to 1.5% of U.S. births (range: 0.1% in Guam to 4.8% in Massachusetts) with the highest rates (>3.5% of all infants born) observed in four states (Connecticut, Massachusetts, New Jersey, and New York), and the District of Columbia. The proportion of ART births was ≤2.5% in the remaining states and territories. Infants conceived with ART comprised 20.0% of all multiple-birth infants (range: 0 in Guam to 40.5% in Massachusetts), 19.0% of all twin infants (range: 0 in Guam to 40.0% in Massachusetts), and 33.0% of triplet or higher order infants (range: 0 in several states to 60.0% in Arizona). Among infants conceived with ART, 46.0% were born in multiple deliveries (range: 0 in Guam to 55.4% in Utah), compared with only 3.0% of infants among all births in the general population (range: 1.3% in Guam to 4.7% in Connecticut). A substantial proportion (43.4%) of ART-conceived infants were twin infants, and a smaller proportion (3.0%) were triplets and higher order infants.
Nationally, infants conceived with ART comprised 5.6% of all low birthweight (<2,500 grams) infants (range: 0 in Guam to 16.0% in Massachusetts) and 5.6% of all very low birthweight (<1,500 grams) infants (range: 0 in Guam to 15.8% in Massachusetts). Overall, among ART-conceived infants, 31.6% were low birthweight (range: 22.6% in New Hampshire to 48.2% in Puerto Rico), compared with 8.0% among all infants (range: 5.7% in Alaska to 12.6% in Puerto Rico); 5.6% of ART infants were very low birthweight (range: 1.9% in Maine to 14.3% in Montana), compared with 1.4% among all infants (range: 0.9% in Alaska to 2.3% in the District of Columbia). Finally, ART-conceived infants comprised 4.4% of all infants born preterm (<37 weeks; range: 0 in Guam to 13.3% in Massachusetts) and 4.9% of all infants born very preterm (<32 weeks; range: 0 in Guam to 16.2% in Massachusetts). Overall, among infants conceived with ART, 36.6% were born preterm (range: 23.6% in New Hampshire to 56.8% in Wyoming), compared with 12.0% among all infants born in the general population (range: 8.4% in Vermont to 17.9% in Guam); 6.6% of ART infants were born very preterm (range: 0 in Maine to 14.5% in Puerto Rico), compared with 2.0% among all infants born in the general population (range: 1.3% in Alaska to 3.0% in the District of Columbia).
Interpretation: The percentage of infants conceived with ART varied considerably by state and territory (range: 0.1% to 4.8%). In most states, multiples from ART comprised a substantial proportion of all twin, triplet, and higher-order infants born in the state, and the rates of low birthweight and preterm infants were disproportionately higher among ART infants than in the birth population overall. Even among women aged <35 years, for whom single embryo transfers should be considered (particularly in patients with a favorable prognosis) according to American Society of Reproductive Medicine (ASRM) guidelines, on average, two embryos were transferred per cycle in ART procedures, influencing the overall multiple infant rates in the United States. ART use per population unit was distributed disproportionately in the United States, with only 13 states showing ART use above the national rate, which might suggest barriers to ART services in the remaining states. Of the four states (Illinois, Massachusetts, New Jersey, and Rhode Island) with comprehensive statewide-mandated health insurance coverage for ART procedures (e.g., coverage for at least four cycles of IVF), three states (Illinois, Massachusetts, and New Jersey) also had rates of ART use >1.5 times the national level. This type of mandated insurance has been associated with greater use of ART and might account for the differences observed in other states.
Public Health Actions: Reducing the number of embryos transferred per ART procedure among all age groups and promotion of eSET procedures, when clinically appropriate, is needed to reduce multiple births, including twin births, and related adverse consequences of ART. Improved patient education and counseling on the risks of twins might be useful in reducing twin births because twins account for the majority of multiples. Although ART contributes to increasing rates of multiple births, it does not explain all of the increases, and therefore the possible role of non-ART fertility treatments warrants further study.
Introduction
Since the birth of the first U.S. infant conceived with Assisted Reproductive Technology (ART) in 1981, use of advanced technologies to overcome infertility has increased steadily, as has the number of fertility clinics providing ART services and procedures in the United States (1). In 1992, Congress passed the Fertility Clinic Success Rate and Certification Act (FCSRCA; Public Law 102-493), which requires that all U.S. fertility clinics performing ART procedures report data to CDC annually on every ART procedure performed. In 1997, CDC published the first annual ART Success Rates Report under FCSRCA, which reported on ART procedures performed in 1995 (2). CDC uses the data it receives to report pregnancy success rates for all ART programs and clinics in the annual ART Success Rates Report (1). Several measures of success for ART are presented in the annual report including the percentage of ART cycles that result in a pregnancy, live-birth deliveries, and singleton live births. Starting with the 2010 data, the ART Success Rates Report was published in two separate reports: a Fertility Clinic Success Rates Report and a National Summary Report (1,3).
ART is associated with potential risks to the mother and fetus. Because multiple embryos are transferred in the majority of ART procedures, ART has been associated with a substantial risk for multiple-gestation pregnancy and multiple births (4–11). Multiple births are associated with greater health problems for mothers and infants, including higher rates of caesarean deliveries, prematurity, low birthweight, infant death, elevated risk of birth defects, and disability (4–15). Further, even singleton infants conceived with ART have a higher risk of low birthweight (16,17).
This report is based on ART surveillance data reported to CDC's Division of Reproductive Health for procedures performed in 2010. Data are presented regarding the use of ART in each U.S. state and territory as well as infant outcomes in 2010 resulting from procedures performed in 2009 and 2010. Additionally, the report examines the contribution of ART to selected adverse outcomes (e.g., multiple birth, low birthweight, and preterm delivery) and compares 2010 ART infant outcomes to outcomes among all infants born in the United States in 2010.
Methods
National ART Surveillance System
In 1996, CDC initiated data collection of ART procedures performed in the United States. ART data for 1995–2003 were obtained from the Society of Assisted Reproductive Technology (SART). Since 2004, CDC has contracted with Westat, Inc., a statistical survey research organization, to obtain data from fertility clinics in the U.S through the National ART Surveillance System (NASS), a web-based data collection system developed by CDC (http://www.cdc.gov/art/NASS.htm). Clinics enter their data into NASS and verify the data's accuracy before sending the data to Westat. The data then are compiled by Westat and reviewed by both CDC and Westat. A few clinics (7.0%) do not report their data to CDC and are listed as nonreporting programs in the Fertility Clinic Success Rates Report as required by FCSRCA. Because nonreporting clinics tend to be smaller, NASS is estimated to contain information on >97.0% of all ART cycles in the United States (1).
Data collected include patient demographics, medical history, and infertility diagnoses; clinical information pertaining to the ART procedure type; and information regarding resultant pregnancies and births. The data file is organized with one record per ART procedure (or cycle of treatment) performed. Multiple procedures from individual patients are not linked. Because ART providers typically do not provide continued prenatal care after a pregnancy is established, information on live births for all procedures is collected by ART clinics either directly from their patients (83.0%) or from their patients' obstetric providers (17.0%).
ART Procedures
ART includes fertility treatments in which both eggs and sperm are handled in the laboratory (i.e., in vitro fertilization [IVF] and related procedures). ART does not include treatments in which only sperm are handled (i.e., intrauterine insemination) or procedures in which a woman takes drugs only to stimulate egg production without the intention of having eggs retrieved. Because an ART procedure consists of several steps over an interval of approximately 2 weeks, a procedure often is referred to as a cycle of treatment. An ART cycle generally begins with drug-induced ovarian stimulation. If eggs are produced, the cycle progresses to the egg-retrieval stage. After the eggs are retrieved, they are combined with sperm in the laboratory through IVF. If this is successful, the most viable embryos (i.e., those that are morphologically most likely to develop and implant) are selected for transfer by clinicians. If an embryo implants in the uterus, a clinical pregnancy is diagnosed by the presence of a gestational sac detectable by ultrasound. Most pregnancy losses occur within the first 12 weeks. Beyond 12 weeks of gestation, the pregnancy usually progresses to a live-birth delivery (with survival probabilities ranging from 95.0% at 16 weeks to 98.0% at 20 weeks), which is defined as the delivery of one or more live-born infants (18).
ART procedures are classified into four types based on the source of the egg (patient or donor) and the status of the embryos (fresh or thawed). Both fresh and thawed embryos might result from either the patient's eggs or from the donor's eggs. ART procedures involving fresh embryos include an egg-retrieval stage. ART procedures that use thawed embryos do not include egg retrieval because the eggs were fertilized during a previous procedure, and the resulting embryos were frozen until the current procedure. An ART procedure can be discontinued at any step for medical reasons or by patient choice.
Variables and Definitions
ART data and outcomes from ART procedures are presented by the patient's state or territory of residence at the time of treatment. If this information was missing, the state or territory of residence was assigned as the state or territory in which the procedure was performed. Cycles among non-U.S. residents are included in NASS data but might be excluded from some calculations for which the exact denominators were not known.
This report presents data on all cycles initiated; however, outcomes are based on cycles that involved embryo transfer. The number of ART procedures performed per 1 million women in the reproductive age (15–44 years) was calculated, and the resulting ratio approximates the proportion of women of reproductive age who used ART in each state or territory. However, this proxy measure of ART use is only an approximation because some women who used ART might fall outside the age range of 15–44 years, and some women might have had more than one procedure during the reporting period.
Live-birth delivery was defined as birth of one or more live-born infants, with delivery of multiple infants counted as one live-birth delivery. A singleton live-birth was defined as a birth of one live-born infant from a single gestation pregnancy. A multiple birth was defined as a birth of two or more infants, at least one of whom was live-born.
Elective single-embryo transfer (eSET) is a procedure in which one embryo, selected from a larger number of available embryos, is placed in the uterus, with extra embryos available for cryopreservation. This procedure does not include cycles in which only one embryo is available. Transfer procedures in which only one embryo was transferred but no embryos were cryopreserved also are excluded from this definition. The embryo selected for eSET might be from a previous IVF cycle (e.g., cryopreserved [frozen] embryos) or from the current fresh IVF cycle that yielded more than one embryo. The remaining embryos might be set aside for future use through cryopreservation. In this report, both eSET procedures and the average number of embryos transferred were calculated only for fresh, nondonor cycles in which at least one embryo was transferred.
The average number of embryos transferred for three age groups (<35 years, 35–40 years, and >40 years) was calculated by dividing the total number of embryos transferred by the total number of embryo-transfer procedures performed in that age group. The percentage of eSET was calculated by dividing the total number of transfer procedures in which only one embryo was transferred and one or more embryos were cryopreserved, by this numerator plus the total number of transfer procedures in which more than one embryo were transferred.
The contribution of ART to an outcome was calculated by dividing the total number of outcomes among ART-conceived pregnancies by the total number of overall outcomes. The contribution of ART to all infants born was calculated by plurality (singleton, multiples, twins, and triplets or higher order births) and by adverse perinatal outcomes (low birthweight and prematurity). The contribution of ART to total infants born in the state or territory was used as a second measure of ART use. The number and percentage of infants (ART-conceived and all infants) born in the state or territory were calculated for singletons, multiples, twins, and triplets or higher order births and for different categories of birthweight and gestational age.
Low birthweight was defined as <2,500 grams, moderate low birthweight as 1,500–2,500 grams, very low birthweight as <1,500 grams, and extremely low birthweight as <1,000 grams. For comparability with births to women who did not undergo ART, for which gestational age is based on the date of the last menstrual period (LMP), gestational age was calculated for fresh cycles by subtracting the date of retrieval from the birth date and adding 14 days. For frozen cycles, and for fresh cycles for which the date of retrieval was not available, gestational age was calculated by subtracting the date of transfer from the birth date and adding 17 days (to account for an average of 3 days in embryo culture). Preterm delivery was defined as gestational age <37 weeks, moderate preterm delivery as gestational age 32–36 weeks, very preterm delivery as gestational age <32 weeks, and extremely preterm delivery as gestational age <28 weeks (19).
Content of This Report
This report provides information on U.S. ART procedures performed in 2010 and compares infant outcomes that occurred in 2010 (resulting from procedures performed in 2009 and 2010) with outcomes for all infants born in the United States in 2010. Specifically, this report provides data on the number and outcomes of all ART procedures performed in the 50 states, the District of Columbia, Guam, the Federated Republic of Micronesia, the Commonwealth of Puerto Rico, and the U.S. Virgin Islands in 2010.* Live-birth delivery rates, the number of live-born infants, live singleton and multiple birth deliveries, and data regarding the number of ART procedures in relation to the number of women in the reproductive age group (15–44 years) are reported (20).† Data also are presented on the number of embryo-transfer procedures performed, the average number of embryos transferred, and the percentage of eSET procedures performed among women who used fresh embryos from their own eggs, by age group, for each state and territory.
For each state and territory, the proportion of singleton, multiple, twin, and triplet or higher order infants resulting from ART are compared with their respective ratios among all infants born in that state in 2010. Infants born in the state or territory during that year include those that were conceived naturally as well as those resulting from ART and other infertility treatments. So that the proportion of ART births among overall U.S. births in 2010 could be assessed accurately, ART births were aggregated from 2 reporting years: 1) infants conceived from ART procedures performed in 2009 and born in 2010 (approximately 69.0% of the live-birth deliveries reported to the ART surveillance system for 2010) and 2) infants conceived from ART procedures performed in 2010 and born in 2010 (approximately 31.0% of the live-birth deliveries reported to the ART surveillance system for 2010). Data on the total number of live-birth and multiple birth infants in each state and territory in 2010 were obtained from U.S. natality files (21). The report presents the number and percentage of select adverse perinatal outcomes (low birthweight, moderate low birthweight, very low birthweight, preterm delivery, moderate preterm delivery and very preterm delivery) among ART- conceived infants and all infants, as well as the contribution of ART to these outcomes. Finally, results for New York City are presented separately from the rest of the state because New York City is an independent vital registration reporting area (21). Therefore, unless otherwise specified, references in this report to New York include only New York state and exclude New York City.
Results
Overview of Fertility Clinics
Of 474 fertility clinics in the U.S. states and territories that performed ART procedures in 2010, a total of 443 (93.0%) provided data to CDC (Figure 1) with the majority located in or near major cities in the eastern United States. The number of fertility clinics performing ART procedures varied by state. States with the largest number of fertility clinics reporting data for 2010 were California (62), New York (including New York City) (37), Texas (34), Illinois (28), Florida (28), and New Jersey (22).
Number and Type of ART Procedures
The number, type, and outcome of ART procedures performed in 2010 are provided for the 50 states, the District of Columbia, New York City, and five U.S. territories (Table 1). State residency data were missing for approximately 3.5% of procedures performed and 3.0% of live-birth deliveries but are included in the total. Approximately 16.0% of ART cycles were conducted among out-of-state residents. Non-U.S. residents accounted for approximately 2.0% of ART procedures, live-birth deliveries, and infants born.
Nationally, a total of 147,260 ART procedures were reported to CDC (Table 1). Of the 147,260 procedures performed, 125,396 (85.2%) progressed to embryo transfer (Table 1). Overall, 46.1% (57,773 of 125,396 ) of ART procedures that progressed to the transfer stage resulted in a pregnancy, 37.6% (47,090 of 125,396) resulted in a live-birth delivery, 26.4% (33,128 of 125,396) resulted in a singleton live-birth delivery, and 11.1% (13,962 of 125,396) resulted in a multiple live-birth delivery. The 47,090 live-birth deliveries from ART procedures performed in 2010 resulted in 61,564 infants (33,128 singleton live-birth deliveries and 13,962 multiple live-birth deliveries) (Table 1; Figure 2).
Six states (California, Illinois, Massachusetts, New Jersey, New York, and Texas) had the highest number of ART procedures performed among residents: California (18,524), New York (excluding New York City) (14,212), Illinois (10,110), Massachusetts (9,854), New Jersey (8,783) and Texas (8,754) (Table 1). Overall, these six states accounted for 47.7% of all ART procedures performed in the United States. Correspondingly, the number of procedures that progressed to embryo transfers was the highest in these six states (California: 16,072; New York: 12,041; Massachusetts: 8,488; Illinois: 8,079; Texas: 7,685; and New Jersey: 7,478) and accounted for 47.7% of all embryo transfer procedures in the United States. The number and percentage of ART-conceived infants born were highest in these six states (California: 7,725 [12.5%]; New York: 4,745 [7.7%]; Texas: 4,413 [7.2%]; New Jersey: 3,856 [6.3%]; Illinois: 3,714 [6.0%]; Massachusetts: 3,403 [5.5%]) and accounted for 45.2% of all infants born from ART in the United States but only 34.0% of all U.S. births (21). Multiple live-birth deliveries were also highest among these states (California: 1,781 [12.8%]; Texas: 1,101 [7.9%]; New York: 995 [7.1%]; New Jersey: 929 [6.7%]; Illinois: 819 [5.9%]; Massachusetts: 667 [4.8%]) and accounted for 45.1% of all ART multiple live-birth deliveries (6,292/13,962).
The number of ART procedures per million women of reproductive age varied from 266 in Puerto Rico to 7,296 in Massachusetts, with an overall national ratio of 2,331 procedures per 1 million women of reproductive age. Thirteen states (California, Connecticut, Delaware, Hawaii, Illinois, Maryland, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Virginia), New York City, and the District of Columbia had ratios higher than the national ratio. Five of these had ratios exceeding twice the national level (Massachusetts (7,296), New York (excluding New York City) (6,653), the District of Columbia (5,763), New Jersey (5,056), and Connecticut (4,996), and two states (Illinois and Maryland) had ratios exceeding one and half times the national level (3,844 and 4,167, respectively) (Figure 3).
Embryo Transfer and Patient's Age
The number of embryo-transfer procedures performed, the average number of embryos transferred per procedure, and the percentage of eSET procedures performed among women who used fresh embryos from their own eggs are provided by age group (Table 2). Overall, the highest number of embryo-transfer procedures performed was among women aged <35 years and lowest among women aged >40 years. Nationally, the average number of embryos transferred per procedure varied from 2.0 among women aged <35 years (range: 1.7 to 2.5) to 2.4 among women aged 35–40 years (range: 1.9 to 4.0), and 3.0 among women aged >40 years (range: 2.0 to 5.0). In 11 states (California, Connecticut, Georgia, Hawaii, Maryland, Massachusetts, New York, Rhode Island, Vermont, Virginia, and Washington), the District of Columbia, New York City, and Puerto Rico, more embryo-transfer procedures were performed among women aged 35–40 years than among younger women. Rates of eSET procedures varied by age group and by state and territory and were highest among women aged <35 years and lowest among women aged >40 years. Nationally, rates of eSET ranged from 10.0% among women aged <35 years (range: 0 in Guam and Idaho to 45.0% in Delaware) to 3.8% among women aged 35–40 years (range: 0 in several states to 34.0% in Delaware) and 0.6% among women aged >40 years (range: 0 in most states to 7.7% in Alabama). Among women aged <35 years, eSET rates exceeded the national rate in 18 states (Arkansas, California, Connecticut, Delaware, Georgia, Illinois, Iowa, Kansas, Maine, Massachusetts, Maryland, Montana, New Hampshire, South Dakota, Tennessee, Virginia, Washington, and West Virginia), the District of Columbia, and the Virgin Islands.
Singleton and Multiple Births
Among 4,046,553 infants born in the U.S in 2010, a total of 59,119 (1.5%) were conceived with ART procedures performed in 2009 and 2010 (Tables 3 and 4). California, Texas, and Florida ranked among the three highest states in total U.S. births. ART-conceived births were highest in California, followed by Texas and New York.
Approximately 0.1% (in Guam) to 4.8% (in Massachusetts) of infants were born with ART. The contribution of ART to all infants born in the state was highest in Massachusetts followed by New York (excluding New York City) (3.8%), Connecticut (3.7%), the District of Columbia (3.7%) and New Jersey (3.6%) (Table 3).
Although singletons accounted for 96.5% of total infants born in 2010, singletons accounted for only 53.6% of all ART infants (range: 44.6% in Utah to 65.7% in Delaware). The percentage of singletons among all infants ranged from 95.3% in Connecticut to 98.7% in Guam.
Nationwide, 46.4% (range: 0 in Guam to 55.4% in Utah) of ART infants were multiples compared with only 3.4% (range: 1.3% in Guam to 4.7% in Connecticut) of all infants (Table 4). ART multiple-birth infants represent 19.8% (range: 0 in Guam to 40.5% in Massachusetts) of total multiple-birth infants. Approximately 43.4% (range: 0 in Guam to 52.0% in Oklahoma) of all ART-conceived infants were twins compared with only 3.3% (range: 1.8% in Puerto Rico to 4.5% in Connecticut) of all infants. ART-conceived twin infants accounted for 19.2% (range: 0 in Guam to 40.2% in Massachusetts) of all twins born in 2010. Finally, 3.0% of ART-conceived infants were triplets or higher order multiples (range: 0 in several states to 10.8% in Puerto Rico) compared with only 0.1% (with very little variation by state) of all infants. ART triplet or higher order multiple infants contributed to 32.5% (range: 0 in several states to 60.0% in Arizona) of all triplet or higher order infants born in 2010.
Adverse Perinatal Outcomes
Nationally, ART infants represented approximately 5.6% of all low birthweight, very low birthweight, and moderate low birthweight infants (Table 5). The contribution of ART to low birthweight infants ranged from 0 in Guam to 16.0% in Massachusetts. The contribution of ART to very low birthweight infants ranged from 0 in Guam to 15.8% in Massachusetts. The contribution of ART to moderate low birthweight infants ranged from 0 in Guam to 16.0% in Massachusetts. In four states (Connecticut, Massachusetts, New Jersey, and New York [excluding New York City]) >10.0% of all low birthweight, moderate low birthweight, and very low birthweight infants born were conceived with ART.
In all states and territories, rates of low birthweight, very low birthweight, and moderate low birthweight infants were higher among infants conceived with ART than among all infants (Table 5). Among ART infants, 31.6% were low birthweight infants (range: 22.6% in New Hampshire to 48.2% in Puerto Rico), compared with 8.2% among all infants (range: 5.7% in Alaska to 12.6% in Puerto Rico). Approximately 5.6% of ART infants were very low birthweight infants (range: 1.9% in Maine to 14.3% in Montana), compared with 1.4% among all infants (range: 0.9% in Alaska to 2.3% in the District of Columbia). Approximately 26.0% of ART infants were moderately low birthweight infants (range: 18.1% in Montana to 35.8% in Oklahoma), compared with 6.7% among all infants (range: 4.8% in Alaska to 11.3% in Puerto Rico). (Table 5). In additional analyses, 2.0% of ART infants were born with a birthweight of less than 1,000g (range: 0 in Alaska, Maine, Vermont, and Wyoming to 8.6% in Montana). Among all very low birthweight (<1,500 g) ART-conceived infants, 39.0% were born with extremely low birthweight (ELBW) of <1,000g.
Nationally, infants conceived with ART contributed approximately 4.4%, 4.9%, and 4.4% respectively to all preterm, very preterm, and moderate preterm infants (Table 6). The contribution of ART to preterm infants ranged from 0 in Guam to 13.3% in Massachusetts. The contribution of ART to very preterm infants ranged from 0 in Guam to 16.2% in Massachusetts. The contribution of ART to moderate preterm birth infants ranged from 0 in Guam to 12.8% in Massachusetts. In four states (Connecticut, Massachusetts, New Jersey, and New York), >10.0% of all preterm, very preterm, and moderate preterm infants in the state were conceived with ART.
As with low birthweight, rates of preterm, very preterm, and moderate preterm infants were higher among ART infants than in the general birth population (Table 6). Among ART infants, 36.6% were born preterm (range: 23.6% in New Hampshire to 56.8% in Wyoming), compared with 12.0% among all infants (range: 8.4% in Vermont to 17.9% in Guam). Approximately, 6.6% of ART infants were very preterm (range: 0 in Maine to 14.5% in Puerto Rico), compared with 2.0% among all infants (range: 1.3% in Alaska to 3.0% in District of Columbia). Approximately 30.0% of ART infants were moderate preterm infants (range: 19.1% in New Hampshire to 45.5% in Wyoming), compared with 10.1% among all infants (range: 6.9% in Vermont to 15.1% in Guam) (Table 6).
In additional analyses, 2.0% of ART infants were born extremely preterm at <28 weeks of gestation (range: 0 in Alaska and Maine to 7.6% in Montana). Among all ART-conceived infants born very preterm (<32 weeks), 40.0% were born extremely preterm (<28 weeks of gestation).
Discussion
Overview
The use of ART has increased substantially in the United States since the beginning of ART surveillance. In 1996 (the first full year for which ART data were reported to CDC), 20,597 infants were born from 64,036 ART cycles (22). Since then, the number of cycles reported to CDC has more than doubled while the number of infants born from ART procedures has nearly tripled. The impact of ART on multiple infant rates and poor birth outcomes is substantial because almost half of ART infants (46.0%) were born in multiple births (compared with only 3.0% of infants among the general birth population). On average, two embryos were transferred among women aged <35 years. National rates of eSET procedures were low, even among women aged <35 years. Rates of low birthweight and preterm births were substantially higher among ART infants (31.6% and 36.6% respectively) than among all infants (8.0% and 12.0% respectively). Overall, 19.2% of all twin and 32.5% of triplet or higher order infants were conceived with ART.
Variations by State
ART use varied widely by state, especially after controlling for the size of the population of women of reproductive age. Residents of California, Illinois, Massachusetts, New York (excluding New York City), New Jersey, and Texas had 45.0% of all ART infants but only 34.0% of all infants born in the United States. Rates of ART use were not correspondingly high in all six states. ART use exceeded twice the national average in only three of these six states (Massachusetts, New Jersey, and New York) (as measured by the number of ART procedures performed per 1 million women of reproductive age). By this measure, Massachusetts ranked highest in ART use whereas California, despite having the highest overall number of ART procedures and the highest number of ART infants, ranked 15th nationally. Furthermore, the contribution of ART to all infants born in the state was 4.8% in Massachusetts compared with 1.5% in California, which also indicates higher ART use in Massachusetts. Similarly, residents of Connecticut, the District of Columbia, Illinois, Maryland, New Jersey, New York, and New York City, in addition to residents of seven other states (California, Delaware, Hawaii, New Hampshire, Pennsylvania, Rhode island, Virginia), had higher rates of ART use than the national average as reflected by the high number of ART procedures performed per 1 million women of reproductive age.
This divergence might be explained in part by variations in state health insurance coverage. Currently, 15 states (Arkansas, California, Connecticut, Hawaii, Illinois, Louisiana, Maryland, Massachusetts, Montana, New Jersey, New York, Ohio, Rhode Island, Texas, and West Virginia) have passed legislation mandating insurance coverage for infertility treatments; four of these states (Illinois, Massachusetts, New Jersey, and Rhode Island) also have mandated comprehensive insurance coverage that must cover at least four cycles of IVF.§ Three out of the four states with mandates (Illinois, Massachusetts, and New Jersey) also had rates of ART use >1.5 times the national level. This type of mandated insurance has been associated with greater use of ART (23–25).
Elective Single-Embryo Transfer Rates
Typically, younger women are better candidates for eSET procedures because they might have more than one embryo available for transfer and better prognosis. Data indicate that eSET rates varied by age group and also by state. ESET procedures were more prevalent among women aged <35 years and varied enormously among states (range: 0 to 45.0%). Although many factors (e.g., a patient's age and diagnostic factors) influence eSET rates, research shows that broad insurance mandates for IVF might result not only in large increases in access to ART services but also in substantially fewer aggressive treatments, with fewer embryos transferred within a procedure (24,26). In the four states with mandatory insurance for ART, among women aged <35 years, eSET rates were higher than the national average of 10.0% in Illinois (10.7%) and Massachusetts (18.2%) but lower in New Jersey (4.3%) and Rhode Island (7.2%). Because ART procedures are expensive, attempts to reduce out-of-pocket costs might result in higher number of embryo transfers per attempt for patients who do not have insurance coverage for ART (24,26). In the United States, private insurance coverage of ART is rare, and it is estimated that approximately 20.0% of all ART costs are covered by state mandate of private insurers and/or by private insurers. Even where mandated, coverage for infertility treatment often varies in scope (23). The higher use of eSET in Illinois and Massachusetts is consistent with previous research linking insurance with embryo transfer practices that might promote eSET. This link is not evident in New Jersey and Rhode Island, both of which had state-mandated insurance for ART but lower-than-national rates of eSET procedures performed. ESET rates also exceeded the national average in a number of states that do not have mandated insurance coverage for ART, especially among women aged <35 years, suggesting compliance with American Society for Reproductive Medicine (ASRM)/Society for Assisted Reproductive Technology (SART) recommendations on eSET (27).
ART Multiple Births
Since 2000 (the first year for which state-specific data were reported by CDC), the percentage of ART-conceived multiple infants in the United States declined by 13.0% (from 53.0% in 2000 to 46.0% in 2010) (28). A sharp decline was noted in the rate of ART-conceived triplets and higher order infants of 67.0% (from 9.0% in 2000 to 3.0% in 2010) and a lesser decline in ART-conceived twin infant rates of 2.0% (from 44.0% in 2000 to 43.0% in 2010).
Despite the decline, multiple birth rates remain high in the United States. On average, two embryos were transferred per cycle among all age groups, even among younger women in 2010. To control costs, patients and providers might be willing to transfer multiple embryos to maximize the chance of live-birth delivery in a single procedure (25). The expected association between fewer average number of embryos transferred and availability of mandated insurance coverage for ART is not wholly supported by our data. The average percentage of embryos transferred among women aged <35 years in the four states with universal mandated coverage (Illinois, 2.0%; Massachusetts, 1.8%; New Jersey, 2.1%; Rhode Island, 2.0%) was similar to the national rate (2.0%). In addition, only in Massachusetts was the rate of ART-conceived multiple infants (38.8%) lower than the national rate of ART multiple infants (46.4%). Thus, rates of ART-conceived multiple infants varied substantially between the four states with mandated insurance, suggesting that the link between insurance and embryo transfer practices such as the number of embryos transferred per procedure, and multiple births might be complex.
Evidence suggests that infertile couples might prefer multiple births, especially twins, in their desire to achieve parenthood, and might not estimate the risks for such pregnancies accurately or they might weigh the risks but see the potential benefits as outweighing them. Infertile women might be more receptive to the idea of a multiple birth than fertile women (29,30). Therefore, understanding the viewpoint of couples undergoing infertility treatments about multiple births is an important consideration. ART providers also can vary widely in their clinical practices for a variety of reasons, which can affect the outcomes in each state; the extent that clinic practices affect the overall state results shown in this report depends on various factors including patient age and diagnostics, the number of cycles performed as well as the number and size of the other clinics in the state.
In 2010, approximately half of all ART infants were born in multiple births. During 1980–2009, the overall twin birth rates in the United States, which comprise the majority of multiple births, increased by 76.0%, from 18.9 to 33.3 per 1,000 births (31). In 2009, one in every 30 babies born in the United States was a twin, compared with one in every 53 babies in 1980 (31). The increased use of infertility treatments, both ART and non-ART fertility treatments (ovulation stimulation medications without ART), likely is associated with this sharp increase (32). Because of the risks associated with multiple-gestation pregnancies, medical experts believe that the best outcome of IVF treatment is a singleton pregnancy followed by a singleton birth (33). Singleton live-birth deliveries have much lower risks than multiple births for adverse birth outcomes such as prematurity, low birthweight, disability, and death.
The economic costs of multiple births are also much higher compared with singleton births. The mean medical cost of delivering a singleton baby was estimated to be $9,329, whereas a set of twins costs $20,318, and triplets have a delivery expense of $153,335 (34). Transferring two embryos is associated with a more than threefold increase in the birth rate and a more than 16-fold increase in the twin birth rate (35). In 2010, the transfer of two embryos was still a common practice, even among younger patients. To improve the likelihood of optimal birth outcomes, patients and providers should agree to transfer fewer numbers of embryos when possible, taking into consideration patient age and prognosis (36). The guidelines on the number of embryos transferred were revised in 2004, 2006, 2008, 2009, and 2012 (37–41). At its 2011 annual meeting, the American Society for Reproductive Medicine Practice Committee noted that the most direct way to limit the risk for multiple gestations from ART is to transfer single embryos (27).
ART Low Birthweight Infants
and Preterm Births
The rates of low birthweight and very low birthweight infants were disproportionately higher among ART infants than in the general birth population. Four states (Connecticut, Massachusetts, New Jersey, and New York) with high number of ART cycles and births also had high ART contributions (>10.0%) to all three categories of low birthweight and preterm births. The contribution of ART to preterm births in the United States, most of which are also low birthweight, is a key concern. Since 1981, the rate of preterm births in the United States has increased >30.0% (42). Fertility treatments, both ART and controlled ovarian stimulations, contribute substantially to preterm births among both multiple and singleton pregnancies (42). Preterm births are a leading cause of infant mortality and morbidity, and preterm infants are at increased risk for death and have more health and developmental problems than full-term infants (42–45). Among ART infants, a substantial proportion of very preterm and very low birthweight infants were born extremely preterm at less than 28 weeks of gestation and with extremely low birthweight at less than 1,000 grams. The health risks associated with preterm births are monumental and have contributed to increasing health-care costs. In 2005, the estimated economic burden associated with preterm births in the United States was $26 billion ($51,600 per infant born preterm) (42). In 2010, ART infants born preterm accounted for approximately 4.0% of all preterm births in the United States, a total economic burden likely to far exceed the earlier estimated costs of $1 billion.
Limitations
The findings in this report are subject to at least six limitations. First, ART surveillance data were reported for each ART procedure performed rather than for each patient who used ART. Linking procedures among patients who underwent more than one ART procedure in a given year is difficult. Second, because patients who underwent more than one procedure in a given year were most likely to include those in which a pregnancy was not achieved during that year but might be achieved with repeated treatments, the success rates reported might represent underestimates if interpreted as per-patient rather than per-cycle success rates. Third, from the available data, it is not possible to differentiate between risks associated with naturally conceived multiple births and risks associated with multiple births resulting from ART procedures. Prematurity and low birthweight could be associated with factors contributing to infertility, and not entirely to ART procedures. Fourth, a small percentage of fertility clinics that performed ART in 2010 did not report their data to CDC and might have had results different from clinics that reported their data. Fifth, four states had a substantial percentage of residency information missing for procedures performed in 2010 (Hawaii: 6.7%, Georgia: 9.2%, Pennsylvania: 9.3%, and Massachusetts: 33.1%). Finally, overall, residency data were missing for approximately 4.0% of procedures performed and 3.0% of all live-birth deliveries resulting from ART procedures performed in 2010.
Conclusion
During 1996–2010, the number of ART procedures performed in the United States doubled while the number of infants born as a result of these procedures nearly tripled. With this increasing use, ART-conceived infants now represent 1.5% of infants born in the U.S and might have a noticeable impact on the prevalence of low birthweight and preterm deliveries in many states, as 46.4% of these infants were born in multiple-gestation pregnancies that resulted in multiple births. Furthermore, although rates of triplet or higher order infants have declined during the last decade, ART-conceived twin infant rates have remained persistently high. Therefore, the impact of ART on poor birth outcomes remains substantial despite the overall decline in multiple infant rates. This could be attributed to the persistently high rates of ART-conceived twin infants, which have declined very little in the last decade. This report documents the rates and contribution of ART to multiples, twins, and triplets, and higher order infants as well as low birthweight infants and preterm infants by each state/territory and allows state health departments to monitor the extent of ART-related adverse perinatal outcomes in their individual state and territories.
Comprehensive insurance coverage of ART might increase access to fertility treatments. The findings in this report indicate that ART use was higher than the national rate in all four states with mandated comprehensive insurance coverage. Three of these four states had utilization rates >1.5 national levels. However, embryo transfer practices were similar to the national rates in all four mandated states. The use of elective single-embryo transfers was higher only in Massachusetts, which had a correspondingly lower rate of ART multiple infants. Further research is needed to ascertain the influence of state insurance mandates on ART use, embryo transfer practices, and infant outcomes, as well as the economic costs of multiple births (23–26), including out-of-pocket costs to patients. Addressing the risk for multiple births also requires understanding the perspectives of couples undergoing infertility treatments who might see a multiple birth, especially twins, as an acceptable or even desired outcome and who might not be aware of the increased risks associated with multiple birth to mother and infants. Clinicians should continue to support ongoing efforts to limit the number of embryos transferred to single embryo to reduce twin rates, which have remained high, and encourage wider implementation of elective single-embryo transfers, when clinically appropriate, as mechanisms of promoting singleton infant births among ART-conceived pregnancies.
CDC is working to extend the utility of NASS by linking to data collected by states (birth certificate, infant deaths, hospital discharge, birth defect registries, and cancer registries) to conduct state-based surveillance of ART, infertility, and related issues. This initiative, the States Monitoring ART (SMART) Collaborative,¶ has been determined to be feasible and useful, especially for monitoring long-term outcomes of ART (46). To date, data from NASS have been linked with vital records from three states (Florida, Massachusetts, and Michigan). The overarching purpose of the SMART Collaborative is to strengthen the capacity of states to evaluate maternal and perinatal outcomes and programs through state-based public health surveillance systems (47).
Further efforts also are needed to monitor the use of non-ART fertility treatments and their role in the rising number of multiple births (42). Despite its substantial impact on adverse birth outcomes, ART only partially explains the overall prevalence of these adverse outcomes in the United States. Preterm births resulting from controlled ovarian stimulation (superovulation-intrauterine insemination and conventional ovulation induction) also might contribute to multiple gestations (42). More research is needed to identify the causes and consequences of preterm births that occur because of infertility treatments and to institute guidelines to reduce the number of multiple gestations (42). The risk for multiple gestations associated with non-ART fertility treatments is less well documented, as clinics are not mandated to report data on their use. Recent studies have demonstrated that singleton infants conceived with ovulation stimulation are more likely than naturally conceived infants to be small for gestational age (48). CDC is monitoring the prevalence of non-ART fertility treatment use among women who had live births and their resultant outcomes in several states through the Pregnancy Risk Assessment Monitoring System (PRAMS)** (49). The most recent ART Surveillance Summary was published by CDC in 2012 (50). CDC will continue to provide updates of ART use in the United States as data become available.
Acknowledgment
Map created by Mary (Dabo) Brantley, PhD, Applied Sciences Branch, Division of Reproductive Health, CDC.
References
- CDC. American Society for Reproductive Medicine, Society for Assisted Reproductive Technology. 2010 Assisted Reproductive Technology Fertility Clinic Success Rates Report. Atlanta, GA: US Department of Health and Human Services, CDC; 2012.
- CDC. American Society for Reproductive Medicine, Society for Assisted Reproductive Technology, RESOLVE. 1995 Assisted Reproductive Technology Success Rates. Atlanta, GA: US Department of Health and Human Services, CDC; 1997.
- CDC. American Society for Reproductive Medicine, Society for Assisted Reproductive Technology. 2010 Assisted Reproductive Technology National Summary Report. Atlanta, GA: US Department of Health and Human Services, CDC; 2012.
- Schieve LA, Peterson HB, Meikle SF, et al. Live-birth rates and multiple-birth risk using in vitro fertilization. JAMA 1999;282:1832–8.
- Schieve LA, Meikle SF, Peterson HB, Jeng G, Burnett NM, Wilcox LS. Does assisted hatching pose a risk for monozygotic twinning in pregnancies conceived through in vitro fertilization? Fertil Steril 2000;74:288–94.
- Reynolds MA, Schieve LA, Martin JA, Jeng G, Macaluso M. Trends in multiple births conceived using assisted reproductive technology, United States, 1997–2000. Pediatrics 2002;111:1159–62.
- Reynolds MA, Schieve LA, Jeng G, Peterson HB, Wilcox LS. Risk of multiple birth associated with in vitro fertilization using donor eggs. Am J Epidemiol 2001;154:1043–50.
- Vahratian A, Schieve LA, Reynolds MA, Jeng G. Live-birth rates and multiple-birth risk of assisted reproductive technology pregnancies conceived using thawed embryos, USA, 1999–2000. Hum Reprod 2002;18:1442–8.
- Wright V, Schieve LA, Vahratian A, Reynolds MA. Monozygotic twinning associated with day 5 embryo transfer in pregnancies conceived after IVF. Hum Reprod 2004;19:1831–6.
- Kissin DM, Schieve LA, Reynolds MA. Multiple-birth risk associated with IVF and extended embryo culture: USA, 2001. Hum Reprod 2005;20:2215–23.
- Reynolds MA, Schieve LA. Trends in embryo transfer practices and multiple gestation for IVF procedures in the USA, 1996–2002. Hum Reprod 2006;21:694–700.
- European Society of Human Reproduction and Embryology (ESHRE) Capri Workshop Group. Multiple gestation pregnancy. Hum Reprod 2000;15:1856–64.
- Mackay AP, Berg CJ, King JC, Duran C, Chang J. Pregnancy-related mortality among women with multifetal pregnancies. Obstet Gynecol 2006;107:563–8.
- Bukulmez O. Does assisted reproductive technology cause birth defects? Current Opin Obstet Gynecol 2009;21:260–4.
- Reefhuis J, Honein MA, Schieve LA, Correa A, Hobbs CA, Rasmussen SA; National Birth Defects Prevention Study. Assisted reproductive technology and major structural birth defects in the United States. Hum Reprod 2009;24:360–6.
- Schieve LA, Meikle SF, Ferre C, Peterson HB, Jeng G, Wilcox LS. Low and very low birthweight in infants conceived with use of assisted reproductive technology. N Engl J Med 2002;346:731–7.
- Schieve LA, Ferre C, Peterson HB, Macaluso M, Reynolds MA, Wright VC. Perinatal outcomes among singleton infants conceived through assisted reproductive technology in the United States. Obstet Gynecol 2004;103:1144–53.
- Farr SL, Schieve LA, Jamieson DJ. Pregnancy loss among pregnancies conceived through assisted reproductive technology, United States, 1999–2002. Am J Epidemiol 2007;165:1380–8.
- Kramer MR, Hogue CR. What causes racial disparities in very preterm birth? A biosocial perspective. Epidemiol Rev 2009;31:84–98.
- US Census Bureau. Annual estimates of the population for the United States and States, and for Puerto Rico: April 1, 2000 to July 1, 2010 (NST-EST2010-01).Washington, DC: US Census Bureau; 2010. Available at http://factfinder.census.gov.
- Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2010. National Vital Stat Rep 2010;61:1–72.
- CDC. American Society for Reproductive Medicine, Society for Assisted Reproductive Technology, RESOLVE. 1996 assisted reproductive technology success rates. Atlanta, GA: US Department of Health and Human Services, CDC; 1998.
- Henne MB and Bundorf MK. Insurance mandates and trends in infertility treatments. Fertil Steril 2008;89:66–73.
- Hamilton BH, McManu B. The effects of insurance mandates on choices and outcomes in infertility treatment markets. Health Econ2012;21:994–1016.
- Bitler,MP, Schmidt L. Utilization of infertility treatments: the effects of insurance mandates. Demography 2012;49:125–49.
- Jain T, Harlow BL, Hornstein MD. Insurance coverage and outcomes of in vitro fertilization. New Engl J Med 2002;347:661–6.
- The Practice Committee of the Society for Assisted Reproductive Technology, the American Society for Reproductive Medicine. Elective single-embryo transfer. Fertil Steril 2012;97:835–42.
- CDC. Assisted reproductive technology surveillance—United States, 2000. MMWR 2003;52(No. SS-9).
- Grobman W, Milad M, Stout J, Klock S. Patient perceptions of multiple gestations: an assessment of knowledge and risk aversion. Am J Obstet Gynecol 2001;185:920–4.
- Blennborn M, Nilsson, S, Hillervik, C, Hellberg, D. The couple's decision-making in IVF: one or two embryos at transfer? Hum Reprod 2005;20:1292–7.
- Martin JA, Hamilton BE, Osterman MJK. Three decades of twin births in the United States, 1980–2009. NCHS data brief, no 80. Bethesda, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2012.
- Schieve LA, Devine O, Boyle CA, Petrini JR, Warner L. Estimation of the contributionof non-assisted reproductive technology ovulation stimulation fertility treatments to US singleton and multiple births. Am J Epidemiol 2009;170:1396–407.
- The Practice Committee of the American Society for Reproductive Medicine. Multiple Gestation Associated with Infertility Therapy: An ASRM Practice Committee Opinion, 2011. Fertil Steril 2012;97:825–34.
- Hidlebaugh DA, Thompson IE, Berger MJ. Cost of assisted reproductive technologies for a health maintenance organization. J Reprod Med 1997;
42:570–4. - Henne, MB and Bundorf MK. The effects of competition on assisted reproductive technology outcomes. Fertil Steril 2010;93:1820–30.
- US American Society for Reproductive Medicine. Guidelines on number of embryos transferred. Birmingham, AL: American Society for Assisted Reproductive Medicine; 1999.
- The Practice Committee of the Society for Assisted Reproductive Technology, the American Society for Reproductive Medicine. Guidelines on the number of embryos transferred. Fertil Steril 2004;
82(Suppl 1):1–2. - The Practice Committee of the Society for Assisted Reproductive Technology, the American Society for Reproductive Medicine. Guidelines on the number of embryos transferred. Fertil Steril 2006;86(Suppl 5):S51–2.
- The Practice Committee of the Society for Assisted Reproductive Technology, the American Society for Reproductive Medicine. Guidelines on the number of embryos transferred. Fertil Steril 2008;90(Suppl 3):S163–4.
- The Practice Committee of the Society for Assisted Reproductive Technology, the American Society for Reproductive Medicine. Guidelines on the number of embryos transferred. Fertil Steril 2009;92:1518–19.
- The Practice Committee of the Society for Assisted Reproductive Technology, the American Society for Reproductive Medicine. Criteria for number of embryos to transfer: a committee opinion. Fertil Steril 2013;99:44–6.
- Behrman RE, Stith Butler A, eds. Preterm birth: causes, consequences, and prevention. Washington, DC: National Academies Press; 2006.
- Callaghan WM, MacDorman MF, Rasmussen SA, Qin C, Lackritz EM. The contribution of preterm birth to infant mortality rates in the United States. Pediatrics 2006;118:1566–73.
- Tanner K, Sabrine N, Wren C. Cardiovascular malformations among preterm infants. Pediatrics 2005;116:e833–8.
- Rasmussen SA, Moore CA, Pauloi LJ, Rhodenhiser EP. Risk for birth defects among premature infants: a population-based study. J Pediatr 2001;138:668–73.
- Kissin DK, Jamieson DJ, Barfield W. Assisted reproductive technology program reporting. JAMA 2011;306:2564; author reply: 2564–5.
- Mneimneh A, Boulet S, Sunderam S, et al. States Monitoring Assisted Reproductive Technology (SMART) Collaborative: data collection, linkage, dissemination, and use. J Womens Health 2013;22:571–7.
- D'Angelo DV, Whitehead N, Helms K, Barfield WD, Ahuwalia IB. Birth outcomes of intended pregnancies among women who used assisted reproductive technology, ovulation stimulation, or no treatment. Fertil Steril 2011;96:314–20.
- Barradas DT, Barfield WD, Wright V, D'Angelo D, Manning SE, Schieve LA. Assessment of assisted reproductive technology use questions: Pregnancy Risk Assessment Monitoring System survey, 2004. Public Health Rep 2012;127:516–23.
- CDC. Assisted reproductive technology surveillance—United States, 2009. MMWR 2012;61(No. SS-7).
* Numbers <20 are not reported to preserve confidentiality but are included in totals.
† Data regarding population size are based on July 1, 2010, estimates from the U.S. Census Bureau (20).
§ Nine states (Arkansas, Connecticut, Hawaii, Louisiana, Maryland, Montana, New York, Ohio, and West Virginia) have restricted mandates. Two states (California and Texas) have other insurance regulations on ART or other infertility treatments but do not require coverage of ART.
¶ SMART is a collaboration between CDC and state health departments in Florida, Massachusetts, and Michigan (information available at http://www. cdc.gov/art/smart.htm).
** PRAMS is a population-based surveillance system of maternal and infant health indicators funded in part by CDC and administered by state health departments (information available at http://www.cdc.gov/PRAMS).
FIGURE1. Location of clinics that perform assisted reproductive technology (ART) procedures — United States, 2010*
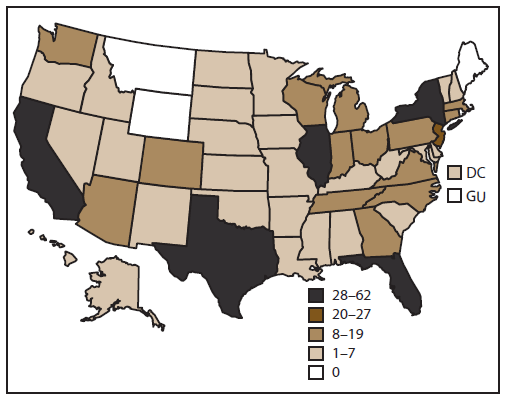
Abbreviations: DC = District of Columbia; GU = Guam.
* In 2010, of 479 ART clinics in the United States, 443 submitted data.
Alternate Text: The figure shows a map of the United States indicating states with clinics that used assisted reproductive technology in 2010. Of 474 ART clinics in the United States, 443 submitted data.
FIGURE 2. Number of outcomes of assisted reproductive technology cycles, by stage — United States, 2010
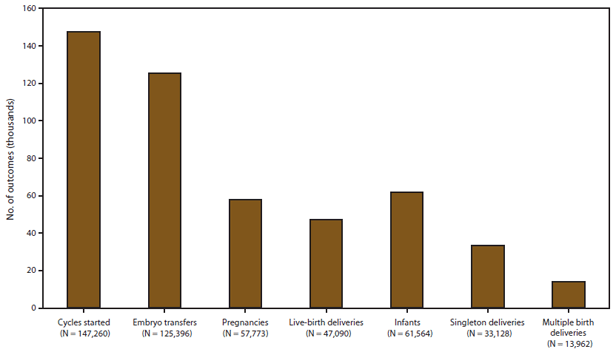
Alternate Text: The figure shows the number of cycles started (147,260), embryo transfers (125,396), pregnancies (57,773), live-birth deliveries (47,090), infants (61,564), singletons (33,128) and multiples (13,962) resulting from use of assisted reproductive technology in the United States in 2010.
FIGURE 3. Number of procedures performed using assisted reproductive technology among women* of reproductive age (ages 15–44 years),
— United States, 2010
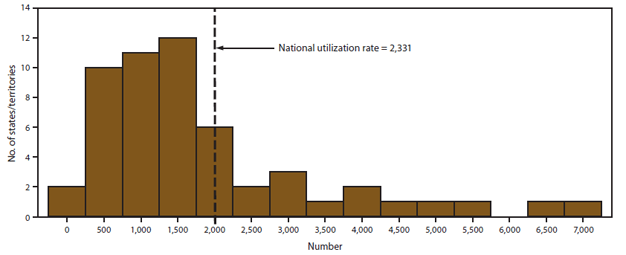
* Per 1 million women aged 15–44 years.
Alternate Text: The figure shows the number of procedures performed in the United States in 2010 using assisted reproductive technology among women of reproductive age, per 1 million women aged 15-44 years, by the number of states and territories. The number of procedures ranged from 0 to 7,000; the national utilization rate was 2,331.
|
TABLE 1. (Continued) Number and outcomes of assisted reproductive technology (ART) procedures, by female patient's state/territory of residence* at time of treatment — United States, 2010 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Patient's state/territory of residence |
No. |
No. |
No. |
No. pregnancies |
No. |
No. |
No. |
No. live-born infants |
Procedures started/women aged 15–44 yrs Ratio |
|
New York§§ |
19 |
14,212 |
12,041 |
4,659 |
3,697 |
2,702 |
995 |
4,745 |
6,653.3 |
|
New York City |
18 |
4,756 |
3,887 |
1,615 |
1,229 |
905 |
324 |
1,559 |
2,487.6 |
|
North Carolina |
10 |
2,934 |
2,563 |
1,286 |
1,089 |
721 |
368 |
1,473 |
1,503.4 |
|
North Dakota |
1 |
196 |
157 |
75 |
63 |
44 |
— |
82 |
1,514.8 |
|
Ohio |
10 |
3,444 |
2,913 |
1,279 |
1,089 |
768 |
321 |
1,430 |
1,543.2 |
|
Oklahoma |
3 |
701 |
624 |
320 |
270 |
173 |
97 |
371 |
950.4 |
|
Oregon |
4 |
1,083 |
954 |
533 |
438 |
283 |
155 |
595 |
1,435.5 |
|
Pennsylvania†† |
19 |
5,738 |
4,740 |
2,145 |
1,753 |
1,264 |
489 |
2,258 |
2,351.6 |
|
Puerto Rico |
3 |
206 |
189 |
79 |
44 |
28 |
— |
62 |
266.0 |
|
Rhode Island |
1 |
721 |
614 |
237 |
198 |
152 |
46 |
244 |
3,360.8 |
|
South Carolina |
4 |
1,091 |
953 |
488 |
428 |
281 |
147 |
576 |
1,174.4 |
|
South Dakota |
1 |
199 |
183 |
95 |
82 |
64 |
— |
102 |
1,303.6 |
|
Tennessee |
8 |
1,099 |
924 |
433 |
374 |
275 |
99 |
478 |
862.2 |
|
Texas |
34 |
8,754 |
7,685 |
3,968 |
3,272 |
2,171 |
1,101 |
4,413 |
1,639.0 |
|
Utah |
3 |
995 |
843 |
429 |
369 |
234 |
135 |
507 |
1,646.1 |
|
Vermont |
1 |
230 |
173 |
70 |
53 |
39 |
— |
67 |
1,945.7 |
|
Virgin Islands |
0 |
— |
— |
— |
— |
— |
— |
— |
|
|
Virginia |
13 |
5,042 |
4,222 |
1,915 |
1,549 |
1,122 |
427 |
1,982 |
3,046.5 |
|
Washington |
11 |
2,718 |
2,385 |
1,261 |
1,044 |
746 |
298 |
1,349 |
2,002.1 |
|
West Virginia |
3 |
282 |
244 |
108 |
90 |
61 |
29 |
119 |
825.1 |
|
Wisconsin |
8 |
1,440 |
1,287 |
587 |
502 |
349 |
153 |
662 |
1,312.7 |
|
Wyoming |
0 |
84 |
76 |
44 |
41 |
24 |
— |
58 |
787.1 |
|
Nonresident |
2,600 |
2,337 |
1,307 |
1,081 |
787 |
294 |
1,385 |
¶¶ |
|
|
Total |
443 |
147,260 |
125,396 |
57,773 |
47,090 |
33,128 |
13,962 |
61,564 |
2,330.8 |
|
* In cases of missing residency data (4%), the patient's state of residence was assigned as the state in which the ART procedure was performed. † Embryo transfer procedures include all procedures that are not cancelled and a transfer was attempted (even if no embryos were transferred, n = 14). § Annual Estimates of the Population for the United States, Regions, States, and Puerto Rico: April 1, 2010 to July 1, 2012 (NST-EST2012-01). Source: U.S. Census Bureau, Population Division. Release date: December 2012. ¶ Data are not provided to preserve confidentiality but are included in totals. ** Of all ART procedures, 0.6% were reported from military medical centers located in California, the District of Columbia, Hawaii, Maryland, and Texas. In each of these areas, ≥1% of ART procedures among residents were performed in a military medical center. In the District of Columbia, 12% of ART procedures among residents were performed in a military medical center. †† A substantial percentage (5%–33%) of residency information was missing for procedures performed in these four states. Overall, residency information was missing for 5,189 (4%) procedures performed and 1,363 (3%) of live-birth deliveries. §§ Outcomes for New York state do not include New York City. ¶¶ Non-U.S. residents excluded from ratio because the appropriate denominators were unknown. |
|||||||||
|
TABLE 2. (Continued) Number of embryo transfer procedures* among patients who used fresh embryos from their own eggs, by female patient's age group and state/territory of residence† at time of treatment — United States, 2010 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Patient's state/territory of residence |
Age group (yrs) |
||||||||
|
<35 |
35–40 |
>40 |
|||||||
|
No. embryo transfer procedures |
Average no. embryos transferred (mean) |
eSET§ |
No. embryo transfer procedures |
Average no. embryos transferred (mean) |
eSET |
No. embryo transfer procedures |
Average no. embryos transferred (mean) |
eSET |
|
|
New York†† |
3,118 |
2.1 |
(7.7) |
3,542 |
2.5 |
(2.8) |
1,700 |
2.8 |
(1.0) |
|
New York City |
710 |
2.1 |
(6.8) |
1,218 |
2.5 |
(3.8) |
791 |
3.0 |
(1.4) |
|
North Carolina |
821 |
2.0 |
(5.3) |
676 |
2.4 |
(2.4) |
136 |
3.0 |
(0) |
|
North Dakota |
62 |
2.1 |
(5.2) |
26 |
2.4 |
(0) |
— |
— |
— |
|
Ohio |
1,043 |
2.1 |
(7.8) |
736 |
2.4 |
(1.2) |
152 |
3.0 |
(0) |
|
Oklahoma |
265 |
2.0 |
(4.5) |
136 |
2.2 |
(3.2) |
21 |
2.7 |
(0) |
|
Oregon |
238 |
2.0 |
(4.7) |
232 |
2.3 |
(5.0) |
51 |
3.2 |
(0) |
|
Pennsylvania** |
1,512 |
2.0 |
(6.9) |
1,277 |
2.4 |
(3.2) |
259 |
2.8 |
(0) |
|
Puerto Rico |
68 |
2.3 |
(3.0) |
78 |
2.5 |
(0) |
— |
2.9 |
(0) |
|
Rhode Island |
195 |
2.0 |
(7.2) |
202 |
2.5 |
(3.3) |
78 |
3.3 |
(0) |
|
South Carolina |
346 |
2.0 |
(2.1) |
209 |
2.3 |
(1.6) |
36 |
3.0 |
(0) |
|
South Dakota |
82 |
1.8 |
(26.3) |
27 |
2.2 |
(4.3) |
— |
2.6 |
(0) |
|
Tennessee |
306 |
2.1 |
(10.8) |
212 |
2.3 |
(3.0) |
32 |
2.5 |
(0) |
|
Texas |
2,585 |
2.0 |
(7.1) |
2,070 |
2.3 |
(3.3) |
449 |
2.9 |
(0.5) |
|
Utah |
390 |
1.9 |
(7.2) |
157 |
2.2 |
(1.5) |
28 |
2.5 |
(0) |
|
Vermont |
37 |
2.0 |
(5.9) |
77 |
2.2 |
(8.8) |
— |
2.7 |
(0) |
|
Virgin Islands |
— |
1.8 |
(20.0) |
— |
2.0 |
(0) |
— |
3.0 |
(0) |
|
Virginia |
1,151 |
1.8 |
(16.8) |
1,294 |
2.2 |
(6.1) |
342 |
2.9 |
(0.4) |
|
Washington |
593 |
1.8 |
(20.7) |
642 |
2.3 |
(7.1) |
184 |
3.0 |
(1.2) |
|
West Virginia |
87 |
2.0 |
(18.4) |
61 |
2.6 |
(3.5) |
— |
3.0 |
(0) |
|
Wisconsin |
468 |
2.0 |
(9.2) |
313 |
2.4 |
(2.4) |
47 |
2.7 |
(0) |
|
Wyoming |
33 |
2.0 |
(3.1) |
— |
2.4 |
(0) |
— |
2.0 |
(0) |
|
Nonresident |
366 |
2.2 |
(5.3) |
462 |
2.4 |
(4.0) |
152 |
2.8 |
(4.0) |
|
Total |
36,390 |
2.0 |
(10.0) |
34,904 |
2.4 |
(3.8) |
11,320 |
3.0 |
(0.6) |
|
Abbreviation: eSET= elective Single Embryo Transfer. * Include all procedures in which at least one embryo was transferred. † In cases of missing residency data (4%), the patient's state of residence was assigned as the state in which the ART procedure was performed. § A procedure in which one embryo, selected from a larger number of available embryos, is placed in the uterus. A cycle in which only one embryo is available is not defined as eSET. ¶ Data are not provided to preserve confidentiality but are included in totals. ** A substantial percentage (5%–33%) of residency information was missing for procedures performed in these four states. †† Outcomes for New York state do not include New York City. |
|||||||||
|
TABLE 3. (Continued) Number, percentage, and proportion of infants born with the use of assisted reproductive technology (ART), by female patient's state/territory of residence* at time of treatment — United States, 2010† |
||||||||
|---|---|---|---|---|---|---|---|---|
|
Patient's state/territory of residence |
No. infants born§ |
No. ART infants born |
Proportion of infants born who are ART infants |
ART |
Singletons |
Proportion of ART singletons among all singletons |
||
|
No. |
(%) |
No. |
(%) |
|||||
|
New York§§ |
123,678 |
4,672 |
3.8 |
2,753 |
(58.9) |
118,630 |
(95.9) |
2.3 |
|
New York City |
120,697 |
1,586 |
1.3 |
954 |
(60.2) |
116,126 |
(96.2) |
0.8 |
|
North Carolina |
122,350 |
1,455 |
1.2 |
718 |
(49.3) |
118,063 |
(96.5) |
0.6 |
|
North Dakota |
9,104 |
87 |
1.0 |
51 |
(58.6) |
8,813 |
(96.8) |
0.6 |
|
Ohio |
139,128 |
1,512 |
1.1 |
781 |
(51.7) |
134,103 |
(96.4) |
0.6 |
|
Oklahoma |
53,238 |
369 |
0.7 |
171 |
(46.3) |
51,535 |
(96.8) |
0.3 |
|
Oregon |
45,540 |
560 |
1.2 |
265 |
(47.3) |
44,014 |
(96.6) |
0.6 |
|
Pennsylvania†† |
143,321 |
2,162 |
1.5 |
1,164 |
(53.8) |
138,009 |
(96.3) |
0.8 |
|
Puerto Rico |
42,153 |
83 |
0.2 |
48 |
(57.8) |
41,382 |
(98.2) |
0.1 |
|
Rhode Island |
11,177 |
239 |
2.1 |
125 |
(52.3) |
10,774 |
(96.4) |
1.2 |
|
South Carolina |
58,342 |
521 |
0.9 |
255 |
(48.9) |
56,415 |
(96.7) |
0.5 |
|
South Dakota |
11,811 |
98 |
0.8 |
60 |
(61.2) |
11,438 |
(96.8) |
0.5 |
|
Tennessee |
79,495 |
458 |
0.6 |
275 |
(60.0) |
76,998 |
(96.9) |
0.4 |
|
Texas |
386,118 |
4,347 |
1.1 |
2,075 |
(47.7) |
374,047 |
(96.9) |
0.6 |
|
Utah |
52,258 |
522 |
1.0 |
233 |
(44.6) |
50,567 |
(96.8) |
0.5 |
|
Vermont |
6,223 |
93 |
1.5 |
51 |
(54.8) |
6,009 |
(96.6) |
0.8 |
|
Virgin Islands |
1,600 |
— |
0.7 |
— |
(81.8) |
1,562 |
(97.6) |
0.6 |
|
Virginia |
103,002 |
1,931 |
1.9 |
1,096 |
(56.8) |
99,226 |
(96.3) |
1.1 |
|
Washington |
86,539 |
1,318 |
1.5 |
677 |
(51.4) |
83,677 |
(96.7) |
0.8 |
|
West Virginia |
20,470 |
124 |
0.6 |
74 |
(59.7) |
19,863 |
(97.0) |
0.4 |
|
Wisconsin |
68,487 |
568 |
0.8 |
282 |
(49.6) |
66,225 |
(96.7) |
0.4 |
|
Wyoming |
7,556 |
44 |
0.6 |
22 |
(50.0) |
7,327 |
(97.0) |
0.3 |
|
Total |
4,046,553 |
59,119 |
1.5 |
31,672 |
(53.6) |
3,907,633 |
(96.5) |
0.8 |
|
* In cases of missing residency data (4%), the patient's state of residency was assigned as the state in which the ART procedure was performed. † Includes infants conceived from ART procedures performed in 2009 and born in 2010, and infants conceived from ART procedures performed in 2010 and born in 2010. Total ART births exclude nonresidents. § Source: US natality file, CDC, National Center for Health Statistics. U.S. births include nonresidents. ¶ ART singletons include singletons from singleton gestations only. ** Data are not provided to preserve confidentiality but are included in totals. †† A substantial percentage (5%–33%) of residency information was missing for procedures performed in these four states. §§ Outcomes for New York state do not include New York City. |
||||||||
|
TABLE 4. (Continued) Number, percentage, and proportion of multiple-birth, twins, and triplets (plus) infants born with use of assisted reproductive technology (ART) procedure, by female patient's place of residence* — United States, 2010† |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Patient's state/territory of residence |
Proportion of ART multiple-birth infants among all multiple-birth infants |
Proportion of ART |
Proportion of ART triplet (plus) infants among all triplet (plus) infants |
||||||||||||
|
ART |
Triplet (plus) infants among all infants¶ |
||||||||||||||
|
ART |
Twin infants |
||||||||||||||
|
ART |
Multiple-birth infants |
||||||||||||||
|
No. |
(%) |
No. |
(%) |
No. |
(%) |
No. |
(%) |
No. |
(%) |
No. |
(%) |
||||
|
North Carolina |
737 |
(50.7) |
4,287 |
(3.5) |
17.2 |
689 |
(47.4) |
4,133 |
(3.4) |
16.7 |
48 |
(3.3) |
154 |
(0.1) |
31.2 |
|
North Dakota |
36 |
(41.4) |
291 |
(3.2) |
12.4 |
36 |
(41.4) |
270 |
(3.0) |
13.3 |
0 |
(0) |
21 |
(0.2) |
0 |
|
Ohio |
731 |
(48.3) |
5,025 |
(3.6) |
14.5 |
649 |
(42.9) |
4,743 |
(3.4) |
13.7 |
82 |
(5.4) |
282 |
(0.2) |
29.1 |
|
Oklahoma |
198 |
(53.7) |
1,703 |
(3.2) |
11.6 |
192 |
(52.0) |
1,655 |
(3.1) |
11.6 |
— |
(1.6) |
48 |
(0.1) |
12.5 |
|
Oregon |
295 |
(52.7) |
1,526 |
(3.4) |
19.3 |
280 |
(50.0) |
1,471 |
(3.2) |
19.0 |
— |
(2.7) |
55 |
(0.1) |
27.3 |
|
Pennsylvania†† |
998 |
(46.2) |
5,312 |
(3.7) |
18.8 |
931 |
(43.1) |
5,107 |
(3.6) |
18.2 |
67 |
(3.1) |
205 |
(0.1) |
32.7 |
|
Puerto Rico |
35 |
(42.2) |
771 |
(1.8) |
4.5 |
26 |
(31.3) |
744 |
(1.8) |
3.5 |
— |
(10.8) |
27 |
(0.1) |
33.3 |
|
Rhode Island |
114 |
(47.7) |
403 |
(3.6) |
28.3 |
111 |
(46.4) |
391 |
(3.5) |
28.4 |
— |
(1.3) |
— |
(0.1) |
25.0 |
|
South Carolina |
266 |
(51.1) |
1,927 |
(3.3) |
13.8 |
251 |
(48.2) |
1,862 |
(3.2) |
13.5 |
— |
(2.9) |
65 |
(0.1) |
23.1 |
|
South Dakota |
38 |
(38.8) |
373 |
(3.2) |
10.2 |
32 |
(32.7) |
355 |
(3.0) |
9.0 |
— |
(6.1) |
— |
(0.2) |
33.3 |
|
Tennessee |
183 |
(40.0) |
2,497 |
(3.1) |
7.3 |
171 |
(37.3) |
2,417 |
(3.0) |
7.1 |
— |
(2.6) |
80 |
(0.1) |
15.0 |
|
Texas |
2,272 |
(52.3) |
12,071 |
(3.1) |
18.8 |
2,093 |
(48.1) |
11,513 |
(3.0) |
18.2 |
179 |
(4.1) |
558 |
(0.1) |
32.1 |
|
Utah |
289 |
(55.4) |
1,691 |
(3.2) |
17.1 |
269 |
(51.5) |
1,625 |
(3.1) |
16.6 |
20 |
(3.8) |
66 |
(0.1) |
30.3 |
|
Vermont |
42 |
(45.2) |
214 |
(3.4) |
19.6 |
42 |
(45.2) |
205 |
(3.3) |
20.5 |
0 |
(0) |
— |
(0.1) |
0 |
|
Virgin Islands |
— |
(18.2) |
38 |
(2.4) |
5.3 |
— |
(18.2) |
38 |
(2.4) |
5.3 |
0 |
(0) |
0 |
(0) |
|
|
Virginia |
835 |
(43.2) |
3,776 |
(3.7) |
22.1 |
795 |
(41.2) |
3,645 |
(3.5) |
21.8 |
40 |
(2.1) |
131 |
(0.1) |
30.5 |
|
Washington |
641 |
(48.6) |
2,862 |
(3.3) |
22.4 |
603 |
(45.8) |
2,795 |
(3.2) |
21.6 |
38 |
(2.9) |
67 |
(0.1) |
56.7 |
|
West Virginia |
50 |
(40.3) |
607 |
(3.0) |
8.2 |
50 |
(40.3) |
591 |
(2.9) |
8.5 |
0 |
(0) |
— |
(0.1) |
0 |
|
Wisconsin |
286 |
(50.4) |
2,262 |
(3.3) |
12.6 |
265 |
(46.7) |
2,163 |
(3.2) |
12.3 |
21 |
(3.7) |
99 |
(0.1) |
21.2 |
|
Wyoming |
22 |
(50.0) |
229 |
(3.0) |
9.6 |
22 |
(50.0) |
220 |
(2.9) |
10.0 |
0 |
(0) |
— |
(0.1) |
0 |
|
Total |
27,447 |
(46.4) |
138,920 |
(3.4) |
19.8 |
25,647 |
(43.4) |
133,390 |
(3.3) |
19.2 |
1,800 |
(3.0) |
5,530 |
(0.1) |
32.5 |
|
* In cases of missing residency data (4%), the patient's state of residency was assigned as the state in which the ART procedure was performed. † ART totals include infants conceived from ART procedures performed in 2009 and born in 2010, and infants conceived from ART procedures performed in 2010 and born in 2010. Total ART births exclude nonresidents. § Includes only the number of infants live-born in a multiple-birth delivery. For example, if three infants were born in a live-birth delivery and one of the three infants was stillborn, the total number of liveborn infants would be two. However, the two infants still would be counted as triplets. ¶ Source: U.S. natality file, CDC, National Center for Health Statistics. U.S. totals include nonresidents. ** Data not provided to preserve confidentiality but included in totals. †† A substantial percentage (5%–33%) of residency information was missing for procedures performed in these four states. §§ Outcomes for New York state do not include New York City. ¶¶ The total number of multiple birth infants in New York City cannot be separated into twins and triplets (plus); the number is reported as an aggregate that includes twins and higher-order multiple birth infants. |
|||||||||||||||
|
TABLE 5. (Continued) Number, percentage, and proportion of infants born with use of assisted reproductive technology (ART), by low birthweight category and female patient's place of residence* — United States, 2010† |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Patient's state/territory of residence |
<2,500 g (LBW) |
<1,500 g (VLBW) |
1,500–2,499 g (MLBW) |
||||||||||||
|
Proportion of ART LBW infants among all LBW infants |
Proportion of ART VLBW |
Proportion of ART MLBW infants among all MLBW infants |
|||||||||||||
|
ART |
All |
||||||||||||||
|
ART |
All |
||||||||||||||
|
ART |
All |
||||||||||||||
|
No. |
(%) |
No. |
(%) |
No. |
(%) |
No. |
(%) |
No. |
(%) |
No. |
(%) |
||||
|
New York§§ |
1,350 |
(28.9) |
9,562 |
(7.7) |
14.1 |
233 |
5.0 |
1,759 |
(1.4) |
13.2 |
1,117 |
(23.9) |
7,803 |
(6.3) |
14.3 |
|
New York City |
401 |
(25.3) |
10,487 |
(8.7) |
3.8 |
53 |
3.3 |
1,923 |
(1.6) |
2.8 |
348 |
(21.9) |
8,564 |
(7.10 |
4.1 |
|
North Carolina |
484 |
(33.3) |
11,109 |
(9.1) |
4.4 |
94 |
6.5 |
2,081 |
(1.7) |
4.5 |
390 |
(26.8) |
9,028 |
(7.4) |
4.3 |
|
North Dakota |
25 |
(28.7) |
607 |
(6.7) |
4.1 |
— |
9.2 |
105 |
(1.2) |
7.6 |
— |
(19.5) |
502 |
(5.5) |
3.4 |
|
Ohio |
501 |
(33.1) |
11,899 |
(8.6) |
4.2 |
110 |
7.3 |
2,303 |
(1.7) |
4.8 |
391 |
(25.9) |
9,596 |
(6.9) |
4.1 |
|
Oklahoma |
151 |
(40.9) |
4,458 |
(8.4) |
3.4 |
— |
5.1 |
749 |
(1.4) |
2.5 |
132 |
(35.8) |
3,709 |
(7.0) |
3.6 |
|
Oregon |
168 |
(30.0) |
2,865 |
(6.3) |
5.9 |
24 |
4.3 |
472 |
(1.0) |
5.1 |
144 |
(25.7) |
2,393 |
(5.3) |
6.0 |
|
Pennsylvania†† |
658 |
(30.4) |
11,941 |
(8.3) |
5.5 |
127 |
5.9 |
2,309 |
(1.6) |
5.5 |
531 |
(24.6) |
9,632 |
(6.7) |
5.5 |
|
Puerto Rico |
40 |
(48.2) |
5,304 |
(12.6) |
0.8 |
— |
13.3 |
544 |
(1.3) |
2.0 |
29 |
(34.9) |
4,760 |
(11.3) |
0.6 |
|
Rhode Island |
69 |
(28.9) |
862 |
(7.7) |
8.0 |
— |
5.9 |
167 |
(1.5) |
8.4 |
55 |
(23.0) |
695 |
(6.2) |
7.9 |
|
South Carolina |
188 |
(36.1) |
5,781 |
(9.9) |
3.3 |
42 |
8.1 |
1,102 |
(1.9) |
3.8 |
146 |
(28.0) |
4,679 |
(8.0) |
3.1 |
|
South Dakota |
33 |
(33.7) |
806 |
(6.8) |
4.1 |
— |
10.2 |
150 |
(1.3) |
6.7 |
23 |
(23.5) |
656 |
(5.6) |
3.5 |
|
Tennessee |
139 |
(30.3) |
7,179 |
(9.0) |
1.9 |
24 |
5.2 |
1,245 |
(1.6) |
1.9 |
115 |
(25.1) |
5,934 |
(7.5) |
1.9 |
|
Texas |
1,674 |
(38.5) |
32,486 |
(8.4) |
5.2 |
297 |
6.8 |
5,531 |
(1.4) |
5.4 |
1,377 |
(31.7) |
26,955 |
(7.0) |
5.1 |
|
Utah |
183 |
(35.1) |
3,655 |
(7.0) |
5.0 |
25 |
4.8 |
574 |
(1.1) |
4.4 |
158 |
(30.3) |
3,081 |
(5.9) |
5.1 |
|
Vermont |
25 |
(26.9) |
382 |
(6.1) |
6.5 |
— |
4.3 |
66 |
(1.1) |
6.1 |
21 |
(22.6) |
316 |
(5.1) |
6.6 |
|
Virgin Islands |
— |
(27.3) |
141 |
(8.8) |
2.1 |
— |
9.1 |
27 |
(1.7) |
3.7 |
— |
(18.2) |
114 |
(7.1) |
1.8 |
|
Virginia |
543 |
(28.1) |
8,448 |
(8.2) |
6.4 |
92 |
4.8 |
1,588 |
(1.5) |
5.8 |
451 |
(23.4) |
6,860 |
(6.7) |
6.6 |
|
Washington |
399 |
(30.3) |
5,464 |
(6.3) |
7.3 |
66 |
5.0 |
876 |
(1.0) |
7.5 |
333 |
(25.3) |
4,588 |
(5.3) |
7.3 |
|
West Virginia |
37 |
(29.8) |
1,880 |
(9.2) |
2.0 |
— |
4.0 |
270 |
(1.3) |
1.9 |
32 |
(25.8) |
1,610 |
(7.9) |
2.0 |
|
Wisconsin |
177 |
(31.2) |
4,818 |
(7.0) |
3.7 |
37 |
6.5 |
859 |
(1.3) |
4.3 |
140 |
(24.6) |
3,959 |
(5.8) |
3.5 |
|
Wyoming |
21 |
(47.7) |
679 |
(9.0) |
3.1 |
— |
4.5 |
83 |
(1.1) |
2.4 |
— |
(43.2) |
596 |
(7.9) |
3.2 |
|
Total |
18,672 |
(31.6) |
331,302 |
(8.2) |
5.6 |
3,298 |
5.6 |
58,462 |
(1.4) |
5.6 |
15,374 |
(26.0) |
272,840 |
(6.7) |
5.6 |
|
Abbreviations: LBW= low birthweight; MLBW= moderate low birthweight; VLBW = very low birthweight. * In cases of missing residency data (4%), the patient's state of residency was assigned as the state in which the ART procedure was performed. † ART totals include infants conceived from ART procedures performed in 2009 and born in 2010, and infants conceived from ART procedures performed in 2010 and born in 2010. Total ART infants exclude nonresidents. § Includes only the number of infants live-born in a multiple-birth delivery. For example, if three infants were born in a live-birth delivery and one of the three infants was stillborn, the total number of live-born infants would be two. However, the two infants still would be counted as triplets. ¶ Source: US natality file, CDC, National Center for Health Statistics. U.S. totals include nonresidents. ** Data are not provided to preserve confidentiality but are included in totals. †† A substantial percentage (5%–33%) of residency information was missing for procedures performed in these four states. §§ Outcomes for New York state do not include New York City. |
|||||||||||||||
|
TABLE 6. (Continued) Number, percentage, and proportion of infants born with use of assisted reproductive technology (ART), by low gestational age category and female patient's place of residence* — United States, 2010† |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Patient's state/territory of residence |
<37 weeks (PTB) |
<32wks (VPTB) |
32–36 wks (MPTB) |
Proportion of |
|||||||||||
|
Proportion of ART |
Proportion of ART VPTB infants among all VPTB infants |
||||||||||||||
|
ART |
All |
||||||||||||||
|
ART |
All |
||||||||||||||
|
ART |
All |
||||||||||||||
|
No. |
(%) |
No. |
(%) |
No. |
(%) |
No. |
(%) |
No. |
(%) |
No. |
(%) |
||||
|
New York§§ |
1,529 |
(32.7) |
13,560 |
(11.0) |
11.3 |
282 |
6.0 |
2,424 |
(2.0) |
11.6 |
1,247 |
(26.7) |
11,136 |
(9.0) |
11.2 |
|
New York City |
479 |
(30.2) |
14,564 |
(12.1) |
3.3 |
71 |
4.5 |
2,454 |
(2.0) |
2.9 |
408 |
(25.7) |
12,110 |
(10.0) |
3.4 |
|
North Carolina |
557 |
(38.3) |
15,569 |
(12.7) |
3.6 |
96 |
6.6 |
2,932 |
(2.4) |
3.3 |
461 |
(31.7) |
12,637 |
(10.3) |
3.6 |
|
North Dakota |
33 |
(37.9) |
989 |
(10.9) |
3.3 |
— |
10.3 |
152 |
(1.7) |
5.9 |
24 |
(27.6) |
837 |
(9.2) |
2.9 |
|
Ohio |
542 |
(35.8) |
17,007 |
(12.2) |
3.2 |
115 |
7.6 |
3,056 |
(2.2) |
3.8 |
427 |
(28.2) |
13,951 |
(10.0) |
3.1 |
|
Oklahoma |
170 |
(46.1) |
7,376 |
(13.9) |
2.3 |
— |
4.9 |
1,119 |
(2.1) |
1.6 |
152 |
(41.2) |
6,257 |
(11.8) |
2.4 |
|
Oregon |
212 |
(37.9) |
4,529 |
(9.9) |
4.7 |
35 |
6.3 |
665 |
(1.5) |
5.3 |
177 |
(31.6) |
3,864 |
(8.5) |
4.6 |
|
Pennsylvania†† |
754 |
(34.9) |
16,250 |
(11.3) |
4.6 |
165 |
7.6 |
2,857 |
(2.0) |
5.8 |
589 |
(27.2) |
13,393 |
(9.3) |
4.4 |
|
Puerto Rico |
39 |
(47.0) |
7,019 |
(16.7) |
0.6 |
— |
14.5 |
920 |
(2.2) |
1.3 |
27 |
(32.5) |
6,099 |
(14.5) |
0.4 |
|
Rhode Island |
80 |
(33.5) |
1,207 |
(10.8) |
6.6 |
— |
7.1 |
210 |
(1.9) |
8.1 |
63 |
(26.4) |
997 |
(8.9) |
6.3 |
|
South Carolina |
226 |
(43.4) |
8,263 |
(14.2) |
2.7 |
48 |
9.2 |
1,506 |
(2.6) |
3.2 |
178 |
(34.2) |
6,757 |
(11.6) |
2.6 |
|
South Dakota |
37 |
(37.8) |
1,349 |
(11.4) |
2.7 |
— |
12.2 |
239 |
(2.0) |
5.0 |
25 |
(25.5) |
1,110 |
(9.4) |
2.3 |
|
Tennessee |
167 |
(36.5) |
10,208 |
(12.8) |
1.6 |
28 |
6.1 |
1,588 |
(2.0) |
1.8 |
139 |
(30.3) |
8,620 |
(10.8) |
1.6 |
|
Texas |
1,998 |
(46.0) |
50,696 |
(13.1) |
3.9 |
345 |
7.9 |
7,799 |
(2.0) |
4.4 |
1,653 |
(38.0) |
42,897 |
(11.1) |
3.9 |
|
Utah |
237 |
(45.4) |
5,682 |
(10.9) |
4.2 |
30 |
5.7 |
756 |
(1.4) |
4.0 |
207 |
(39.7) |
4,926 |
(9.4) |
4.2 |
|
Vermont |
26 |
(28.0) |
524 |
(8.4) |
5.0 |
— |
2.2 |
93 |
(1.5) |
2.2 |
24 |
(25.8) |
431 |
(6.9) |
5.6 |
|
Virgin Islands |
— |
(36.4) |
201 |
(12.6) |
2.0 |
— |
9.1 |
33 |
(2.1) |
3.0 |
— |
(27.3) |
168 |
(10.5) |
1.8 |
|
Virginia |
683 |
(35.4) |
11,969 |
(11.6) |
5.7 |
104 |
5.4 |
2,088 |
(2.0) |
5.0 |
579 |
(30.0) |
9,881 |
(9.6) |
5.9 |
|
Washington |
442 |
(33.5) |
8,785 |
(10.2) |
5.0 |
85 |
6.4 |
1,253 |
(1.4) |
6.8 |
357 |
(27.1) |
7,532 |
(8.7) |
4.7 |
|
West Virginia |
42 |
(33.9) |
2,480 |
(12.1) |
1.7 |
8 |
6.5 |
363 |
(1.8) |
2.2 |
34 |
(27.4) |
2,117 |
(10.3) |
1.6 |
|
Wisconsin |
215 |
(37.9) |
7,425 |
(10.8) |
2.9 |
44 |
7.7 |
1,262 |
(1.8) |
3.5 |
171 |
(30.1) |
6,163 |
(9.0) |
2.8 |
|
Wyoming |
25 |
(56.8) |
831 |
(11.0) |
3.0 |
5 |
11.4 |
138 |
(1.8) |
3.6 |
20 |
(45.5) |
693 |
(9.2) |
2.9 |
|
Total |
21,638 |
(36.6) |
486,622 |
(12.0) |
4.4 |
3,924 |
6.6 |
79,493 |
(2.0) |
4.9 |
17,714 |
(30.0) |
407,129 |
(10.1) |
4.4 |
|
Abbreviations: PTB = preterm birth; MPTB = moderate preterm birth; VPTB = very preterm birth. * In cases of missing residency data (4%), the patient's state of residency was assigned as the state in which the ART procedure was performed. † ART totals include infants conceived from ART procedures performed in 2009 and born in 2010, and infants conceived from ART procedures performed in 2010 and born in 2010. Total ART births exclude nonresidents. § Includes only the number of infants live-born in a multiple-birth delivery. For example, if three infants were born in a live-birth delivery and one of the three infants was stillborn, the total number of live-born infants would be two. However, the two infants still would be counted as triplets. ¶ Source: U.S. Natality File, CDC, National Center for Health Statistics. U.S. totals include nonresidents. ** Data not provided to preserve confidentiality but included in totals. †† A substantial percentage (5%–33%) of residency information was missing for procedures performed in these four states. §§ Outcomes for New York state do not include New York City. |
|||||||||||||||
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


