Prevalence of Age-Related Macular Degeneration (AMD)
AMD Composite Prevalence Estimates at a Glance
| Data Type | Predicted prevalence rates and prevalence counts created using a statistical modeling approach |
|---|---|
| Source Data |
|
| Case Definition |
|
| Year | Released 2022, estimates based on 2019 population estimates. |
| Publications | Prevalence of Age-Related Macular Degeneration in the United States in 2019 |
| Suggested Citations | Rein DB, Wittenborn JS, Burke-Conte Z, Gulia R, Robalik T, Ehrlich JR, Lundeen EA, Flaxman AD. Prevalence of Age-Related Macular Degeneration in the United States in 2019. JAMA Ophthalmology. 2022; in press. |
Overview
The Vision and Eye Health Surveillance System (VEHSS) composite prevalence estimate of AMD is CDC’s primary estimate of the prevalence of AMD in the United States. VEHSS researchers used a statistical method called Bayesian meta-regression to combine information from multiple data sources available in VEHSS to produce AMD prevalence estimates among the entire US population in 2019. VEHSS includes crude and standardized estimates (standardized to the national age, sex, and race/ethnicity distribution).
Case Definition:
AMD is defined as having vision threatening or non-vision threatening AMD, as measured using the retinal imaging module of the National Health and Nutrition Examination Survey (NHANES).
- Vision Threatening AMD: Also referred to as “Late Stage AMD,” includes vision threatening advanced stages of AMD including geographic atrophy and/or exudative AMD (alternatively defined as wet-form AMD or choroidal neovascularization) in either eye.
- Non-Vision Threatening AMD: Also referred to as “Early Stage AMD,” includes retinal pigment epithelium abnormalities or drusen ≥125 µm in the worse-affected eye, but no vision threatening AMD in either eye.
Overall Findings
- In 2019, an estimated 19.8 million (12.6%) Americans aged 40 and older were living with age-related macular degeneration (AMD).
- Of these, 1.49 million (0.94%) were living with vision threatening
- Prevalence of AMD increased with age from 2% (95% Uncertainty Interval [UI]: 1.3 to 2.9) among people aged 40 to 44 to 46.6% (95% UI: 28.4 to 72.4) among people aged ≥85.
- Sex- and age-standardized rates of AMD were lower for non-Hispanic Black people (7.0%, 95%UI: 5.2% to 9.1%) than for other racial and ethnic groups (13.3%, 95% UI: 10.2% to 17.1%).
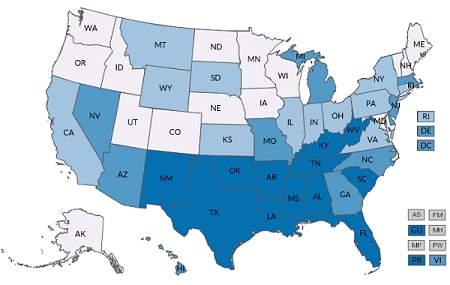
- AMD prevalence varied substantially at the state and county level, even after accounting for differences in demographics.
- By state, the crude prevalence of AMD ranged from a low of 6.2% in the District of Columbia to a high of 18.3% in Florida.
National Results:
Table 1. Prevalence of Early, Late, or Any Stage of Age-Related Macular Degeneration (AMD) in 2019, Number of People (95% Uncertainty Interval)
| Non-Vision Threatening AMD |
Vision Threatening AMD |
Any AMD |
|
|---|---|---|---|
| Overall National | 18,343,000 (15,300,000 – 22,025,000) |
1,486,000 (975,000 – 2,146,000) |
19,828,000 (16,275,000 – 24,171,000) |
| Female | 9,205,000 (7,224,000 – 11,514,000) | 884,000 (534,000 – 1,348,000) | 10,089,000 (7,758,000 – 12,862,000) |
| Male | 9,137,000 (7,187,000 – 11,513,000) | 602,000 (361,000-915,000) | 9,739,000 (7,547,000 – 12,427,000) |
| Black (Non-Hispanic) | 1,142,000 (870,000 – 1,470,000) | 88,000 (51,000 – 140,000) | 1,230,000 (921,000 – 1,610,000) |
| Hispanic | 2,061,000 (1,591,000 – 2,612,000) | 51,000 (22,000 – 102,000) | 2,111,000 (1,612,000 – 2,715,000) |
| White (Non-Hispanic) | 14,035,000 (11,143,000 – 17,647,000) | 1,254,000 (785,000 – 1,856,000) | 15,289,000 (11,928,000 – 19,503,000) |
| Other race/ethnicity | 1,105,000 (756,000-1,542,000) | 93,000 (40,000-184,000) | 1,199,000 (796,000 – 1,726,000) |
| 40-64 Years | 7,460,000 (5,800,000 – 9,472,000) | 146,000 (82,000 – 235,000) | 7,605,000 (5,882,000 – 9,706,000) |
| 65-84 Years | 8,650,000 (6,619,000 – 11,184,000) | 618,000 (359,000 – 956,000) | 9,269,000 (6,978,000 – 12,140,000) |
| 85+ Years | 2,232,000 (1,388,000 – 3,415,000) | 722,000 (409,000 – 1,169,000) | 2,954,000 (1,797,000 – 4,585,000) |
Figure 1. Percentage of 2019 US Resident Population With Age-Related Macular Degeneration, by Stage and Age Group
Figure 2. Percentage of 2019 US Resident Population with Age-Related Macular Degeneration, by Sex and Race/Ethnicity
Figure 3. Crude or Adjusted Percentage of 2019 US Resident Population With Any Age-Related Macular Degeneration (AMD) or Vision Threatening AMD, by County
*“Crude Prevalence” reports the actual estimated prevalence of vision loss or blindness per county. “Adjusted Prevalence” reports county level estimates standardized to the 2010 US population by age, race/ethnicity, and sex. Adjusted Prevalence shows county-level variation in vision loss or blindness that is not explained by differences in the population distribution by age, race/ethnicity, or sex across counties.
Stage
Stage
- Any AMD
- Vision threatening AMD
- Non-vision threatening AMD
- Any AMD
- Vision threatening AMD
- Non-vision threatening AMD
Age Group
Age Group
- Ages ≥40 years
- Detailed age groups (5-year groups)
- Major age groups (40-64, 65-84, ≥85 years)
- Ages ≥40 years
- Detailed age groups (5-year groups)
- Major age groups (40-64, 65-84, ≥85 years)
Sex
Sex
- All
- Male
- Female
- All
- Male
- Female
Race/Ethnicity
Race/Ethnicity
- All racial and ethnic groups
- Black (non-Hispanic)
- Hispanic
- White (non-Hispanic)
- Other racial and ethnic groups
- All racial and ethnic groups
- Black (non-Hispanic)
- Hispanic
- White (non-Hispanic)
- Other racial and ethnic groups
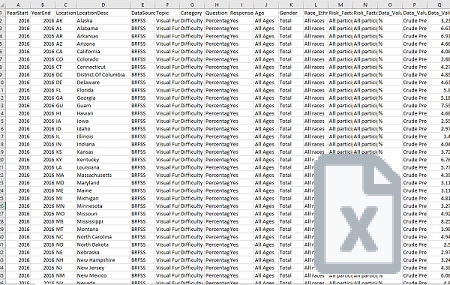
Data Type
Data Type
- Crude prevalence
- Adjusted prevalence (adjusted by age, race/ethnicity, and sex)
- Crude prevalence
- Adjusted prevalence (adjusted by age, race/ethnicity, and sex)
| National | State | County |
|---|---|---|
Methods
The VEHSS composite prevalence estimates of AMD were generated using a statistical modeling approach called Bayesian meta-regression, which is used to combine information from multiple VEHSS data sources into a single summary estimate. The VEHSS estimates use measured AMD based on retinal imaging from National Health and Nutrition Examination Survey (NHANES) as the reference point dataset to create output based on the characteristics and performance of the NHANES retinal imaging exam. In addition to NHANES, the estimation model used population-based study data to provide additional evidence on the prevalence of AMD by stage and demographic group, 2018 Medicare claims data to provide evidence on the single-year age trends and regional variation in AMD, and 2019 American Community Survey data to estimate the underlying US population at risk for AMD. Full details of the methods are available in the publication by Rein et al 2022.
Other AMD Indicators in the VEHSS Data Explorer
CDC uses the VEHSS composite estimate as the primary estimate to assess the percentage of people with AMD in the United States by state, county, and across different age groups, racial and ethnic groups, and sex. However, VEHSS also contains several other data sources with prevalence or useful information about AMD. Readers should consider all sources when deciding which to use to fit their specific information needs.
Self-Report Measures: VEHSS contains estimates of people who reported that a doctor ever told them they had AMD from the National Health Interview Survey. These estimates provide a measure of how many people are aware they have AMD, whereas the composite prevalence estimates measure AMD whether it is diagnosed or not.
Examination-Based AMD: VEHSS contains prevalence estimates of measured AMD from NHANES. This is one of the primary inputs into the composite prevalence estimate. These estimates are available in the VEHSS Data Explorer but are only available at the national level, were last collected in 2008, and do not incorporate statistical corrections and adjustments included in the composite prevalence estimates.
Diagnosed AMD: The VEHSS Data Explorer also contains information on patients with diagnosed AMD from administrative claims data, including Medicare, Medicaid, commercial medical insurance, and managed vision care insurance, in addition to electronic health record registry data from the IRIS Registry. These data use diagnosis codes to measure the percentage of patients in each dataset who had a claim or encounter containing an AMD diagnosis code during a calendar year. These datasets provide large samples of millions of patients each and include additional detail on AMD prevalence by clinical stages. However, these data sources are convenience samples, will only capture diagnosed and treated AMD, and cannot provide nationally representative estimates.
Utilization Measures: The VEHSS Data Explorer contains information on using health services related to AMD as coded in insurance claims information from Medicare, Medicaid, commercial medical insurance (MarketScan), and managed vision care (VSP) programs, as well as services included in ophthalmology electronic health records summarized by the IRIS Registry. These estimates measure the proportion of patients who had an AMD diagnosis during a calendar year and received at least one medical service related to AMD treatment, including anti-vascular endothelial growth factor (VEGF) injections or photocoagulation.
Summary
The VEHSS Composite Estimates of AMD are CDC’s estimate of the percentage of US residents who have AMD, where they live, and who they are. These estimates are based on data that identify AMD by retinal imaging and therefore represents total prevalence and not just diagnosed prevalence, such as would be measured in a self-report survey, or in claims data. That said, users should consider the differences in available measures when determining the most appropriate resource to answer their specific research question.