Medicaid
Medicaid Claims at a Glance
| Medicaid T-MSIS claims | |
|---|---|
| Description | 100% Medicaid Transformed Medicaid Statistical Information System (T-MSIS) |
| Sample | Full population of Medicaid and Children’s Health Insurance Program (CHIP) beneficiaries from states and programs participating in the T-MSIS. |
| VEHSS Topics Included |
|
| Approximate Size | 55 million persons per year |
Medicaid Transformed Medicaid Statistical Information System (T-MSIS) data are a set of de-identified person-level data files with information on enrollment, eligibility, service utilization, diagnoses, and payments in Medicaid and Children’s Health Insurance Program (CHIP). Owned by the Centers for Medicare and Medicaid Services (CMS), Medicaid data cover everyone enrolled in Medicaid and CHIP from participating states within a given year. The new T-MSIS system provides several improvements over the Medicaid MAX data previously used in VEHSS, including expanded data elements, the inclusion of CHIP data, more participating states, and the inclusion of files for managed care plans, providers, and third-party liability.
Please see Medicaid.gov for more information
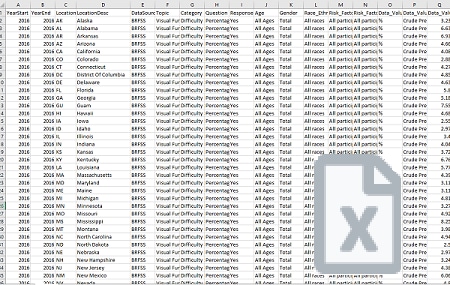
The VEHSS team calculated prevalence of diagnosed eye and vision disorders and prevalence of receipt of covered eye care services in Medicaid and CHIP claims based on the presence of ICD9 and ICD10 diagnosis codes and CPT procedure codes on any patient claim during the year of observation.
VEHSS reports summary prevalence and counts for the topics and categories listed, by the geographic levels and stratification factors listed below:
Available Geographic Levels
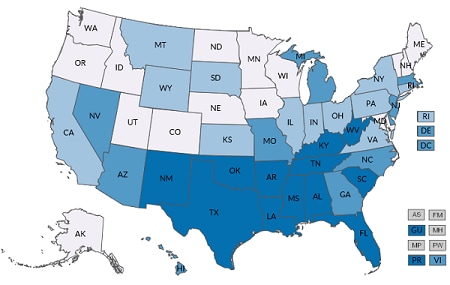
| National | State* | County* |
|---|---|---|
*Not all states are included in T-MSIS data, county data is only available for participating states. State coverage differs by year.
| Included Stratification Factors (State and National Estimates) | |
|---|---|
| Age Group |
|
| Gender |
|
| Race/Ethnicity |
|
| Risk Factors |
|
| Data Type |
|
A detailed description of the VEHSS analysis of T-MSIS is described in the report “VEHSS Claims & Registry Data Analysis Plan [PDF – 579 KB].”
Full analysis documentation is included in the “VEHSS Medicare Data Report [PDF – 1.5 MB]
The VEHSS analysis of Medicaid data is subject to a number of potential limitations:
- Medicaid claims are intended for billing purposes only. Diagnosis information included on claims is intended to justify payment. Therefore, diagnosis data on claims may suffer from bias or limited detail.
- Medicaid does not cover all healthcare services and coverage differs by patient, plan and state. Medicaid patients may utilize these services using a different payer, and thus these services are not captured in Medicaid data.
- Patients may be insured by multiple insurers. Thus, even normally covered ophthalmology services may not be indicated in Medicaid data if services were reimbursed by another plan.
- A large proportion of Medicaid beneficiaries are enrolled for only part of the year. Unlike other administrative claims databases included in VEHSS, we did not require full annual coverage because this would have excluded the majority of patients and services. We therefore allow Medicaid beneficiaries who have at least 1 month of enrollment.
- While Medicaid claims represent the universe of persons enrolled in Medicaid, the data are only representative of persons in the Medicaid program. Because the Medicaid population differs substantially from the general population, users should not attempt to infer results from Medicaid data to all persons in the general population.