Continuing Opioid Therapy

This page provides an overview for continuing opioid therapy. Please review the 2022 Clinical Practice Guideline for Prescribing Opioids for Pain (2022 Clinical Practice Guideline) for more detailed guidance.
Continuing Opioid Therapy refers to when clinicians continue to prescribe opioids for acute, subacute, and chronic pain for patients who are already on opioid therapy. For more information about initially prescribing opioids to patients for acute, subacute, and chronic pain for shorter durations, please visit Initiating Opioids.
Clinicians should always involve patients in decisions about whether to continue opioid therapy, including discussing the benefits and risks for changing the opioid dosage.

Before continuing opioid therapy, ensure patients are aware of the following factors:
- Expected benefits of continuing opioids
- Common risks of opioids
- Serious risks of opioids
- Alternative therapies to opioids
Shared decision-making is important when weighing the benefits and risks of continuing opioid therapy.
If benefits outweigh the risks for continued opioid therapy, clinicians should work closely with patients to optimize non-opioid therapies while continuing opioid therapy.
If benefits do not outweigh the risks for continued opioid therapy, clinicians should optimize other therapies and work closely with patients to gradually taper to lower dosages or, if warranted based on the individual clinical circumstances of the patient, to appropriately taper and discontinue opioids.
Unless a patient has indications of a life-threatening issue, such as warning signs of impending overdose, opioid therapy should not be discontinued abruptly. Clinicians should carefully weigh both the benefits and risks for continuing opioid medications and the benefits and risks for tapering opioids (Recommendation 5).
| Duration of less than 1 month
Assess the benefits and risks for opioids at least every 2 weeks |
|
SUBACUTE PAIN
Within 1 to 4 weeks of starting opioid therapy
CHRONIC PAIN
Within 1 to 4 weeks of starting long-term opioid therapy or of dose escalation Assess the benefits and risks of opioids at least every 3 months or when increasing dosage |
|
| Assess the benefits and risks of opioids more frequently than every 3 months
|
Clinicians should regularly evaluate risk for opioid-related harms and discuss with patients because conditions can change during the course of treatment (Recommendation 8). |
| For example, if a patient is already receiving long-term opioids and requires additional opioids for severe acute pain (e.g., major surgery) |
|
*See Recommendations 4, 5, 6, and 7 for more information on continuing opioid therapy for acute, subacute, or chronic pain.
Follow-up is recommended within 1 to 4 weeks of starting opioid therapy for subacute or chronic pain or after increasing dosage (Recommendation 7). Consider follow-up intervals within the lower end of this range when:
- Extended-release and long-acting (ER/LA) opioids are started or increased.
- Total daily opioid dosage is at least 50 MME/day.
Patients receiving opioid therapy for chronic pain should receive regular reassessment of benefits and risks. The suggested interval is every 3 months or more frequently depending on the clinical scenario. During follow up appointments, clinicians should ask patients about their preferences for continuing opioids based on the effects of therapy on pain and function relative to any adverse effects experienced.
Patients with subacute pain that initially received opioid therapy for acute pain and have been treated for more than 30 days should take care to ensure that opioid prescribing does not unintentionally become long-term opioid therapy. Initiation of long-term opioid therapy should occur only as an intentional decision that benefits are likely to outweigh risks following informed discussion between clinician and patient and as a part of a comprehensive pain management approach (Recommendation 2).
Clinicians should carefully evaluate a decision to increase dosage based on individualized assessment of:
- Diagnosis.
- Incremental benefits for pain and function relative to risks.
- Other treatments and effectiveness.
- Patient values and preferences.
Clinicians should evaluate and discuss a patient’s risk for opioid-related harms (Recommendation 8). Strategies to mitigate risk such as offering naloxone should be incorporated into the patient’s comprehensive pain management plan. When considering long-term opioid therapy, ensure that treatment for depression and other mental health conditions is optimized, consulting with behavioral health specialists when needed.
If continuing opioid therapy in patients with prior opioid overdose:
- Discuss increased risks for overdose with patients.
- Consider whether the benefits of opioids outweigh substantial risks.
- Incorporate strategies to mitigate risk into the pain management plan, such as offering naloxone and increasing frequency of monitoring.
When assessing risk and other potential harms of continuing opioid therapy, clinicians should evaluate other situations that may be risky for the patient (i.e., comorbidities). Below are some examples of situations that increase patients’ risk for harm.
The 2022 Clinical Practice Guideline provides recommendations to equip clinicians with the information they need to discuss pain care options with their patients. Before starting and periodically during continuation of opioid therapy clinicians should:
- Offer naloxone when prescribing opioids to patients at increased risk for overdose, including those:
- With a history of overdose or a substance use disorder
- With sleep-disordered breathing
- Taking higher dosages of opioids (e.g., ≥50 MME/day)
- At risk for returning to a high dose to which they have lost tolerance (e.g., patients undergoing tapering or recently released from prison)
- Taking benzodiazepines with opioids (Recommendation 11)
For more information and resources about talking with patients, family members, friends, and caregivers about naloxone, visit Naloxone Can Save Lives.
- Use additional caution and increased monitoring (Recommendation 7) to minimize risks of opioids prescribed for:
- Patients with renal or hepatic insufficiency
- Patients 65 years and older
- Implement interventions to mitigate common risks of opioid therapy among older adults, such as:
- Exercise or bowel regimens to prevent constipation
- Risk assessment for falls
- Monitoring for cognitive impairment
- Avoid prescribing opioids to patients with moderate or severe sleep-disordered breathing, when possible, to minimize risks for opioid overdose.
- Use PDMP data (Recommendation 9) and toxicology screening (Recommendation 10) as appropriate to assess for concurrent substance use that might place patients at higher risk for opioid use disorder and overdose.
- Assess patients’ abilities to safely perform daily work that involves potentially hazardous tasks (e.g., driving, use of heavy equipment, climbing ladders, working at heights or around moving machinery, working with high voltage equipment) where receiving opioids or other medications that can negatively affect sleep, cognition, balance, or coordination.
*To read more information on situations or other specific considerations that are risky for prescribing opioids, see Recommendation 8 of the 2022 Clinical Practice Guideline.
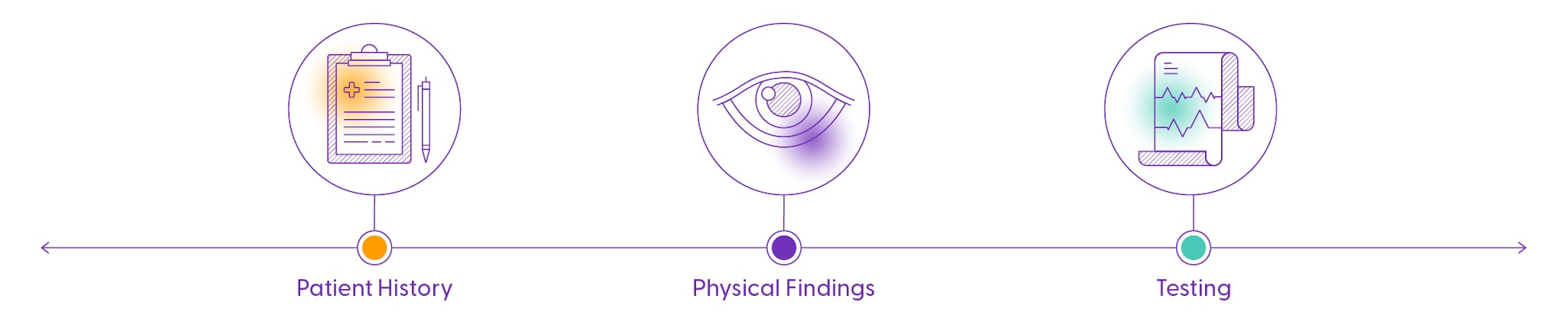
During long-term opioid therapy, prescription drug monitoring program (PDMP) data should be reviewed at least every 3 months or more frequently (Recommendation 9). Clinicians should use specific PDMP information about medications prescribed to their patient in the context of other clinical information, including their patient’s history, physical findings, and other relevant testing, in order to help protect and communicate with their patient. Learn more about PDMP programs here.
When prescribing opioids for subacute or chronic pain, clinicians should consider the benefits and risks for toxicology screening, such as urine drug screening, to assess for prescribed medications as well as other prescribed and non-prescribed controlled substances that increase risk for overdose when combined with opioids, such as benzodiazepines and illicit opioids.
Before ordering toxicology testing, clinicians should have a plan for responding to unexpected results. Clinicians should explain to patients that the results will not be used punitively (e.g., to dismiss patients from care) and that testing is intended to improve their safety.
Use Caution When Prescribing Concurrent Opioid Medications and Other Central Nervous System Depressants
Clinicians should use caution when prescribing opioid pain medication and benzodiazepines concurrently. Clinicians should also consider whether the benefits outweigh the risks for concurrent prescribing of opioids and other central nervous system depressants such as:
- Muscle relaxants
- Non-benzodiazepine sedative hypnotics
- Potentially sedating anticonvulsant medications such as gabapentin and pregabalin
Clinicians should check the PDMP for concurrent controlled medications prescribed by other clinicians and consider involving pharmacists as part of the management team when opioids are co-prescribed with other central nervous system depressants.
For more information about the 2022 Clinical Practice Guideline, visit What’s New, What’s Changed.
*Disclaimer: This webpage provides a high-level overview of continuing opioid therapy. For in-depth information and implementation considerations of the guidance, you are encouraged to read the full 2022 Clinical Practice Guideline for Prescribing Opioids for Pain.
