QuickStats: Percentage* of Residential Care Community Residents with an Advance Directive,† by Census Division§ — National Study of Long-Term Care Providers, 2016
Weekly / July 20, 2018 / 67(28);790
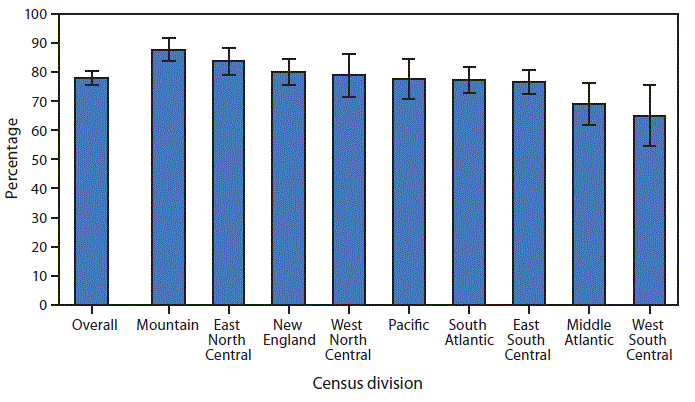
* With 95% confidence intervals shown with error bars.
† Based on the question “Of the current residents, how many have documentation of an advance directive in their file?” asked of the 98% of communities that responded “yes” to “Does this residential care community typically maintain documentation of residents’ advance directives or have documentation that an advance directive exists in resident files?”
§ New England: Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont; Middle Atlantic: New Jersey, New York, and Pennsylvania; East North Central: Illinois, Indiana, Michigan, Ohio, and Wisconsin; West North Central: Iowa, Kansas, Minnesota, Missouri, Nebraska, North Dakota, and South Dakota; South Atlantic: Delaware, Florida, Georgia, Maryland, North Carolina, South Carolina, Virginia, District of Columbia, and West Virginia; East South Central: Alabama, Kentucky, Mississippi, and Tennessee; West South Central: Arkansas, Louisiana, Oklahoma, and Texas; Mountain: Arizona, Colorado, Idaho, Montana, Nevada, New Mexico, Utah, and Wyoming; Pacific: Alaska, California, Hawaii, Oregon, and Washington.
In 2016, 77.9% of residents in residential care communities had an advance directive documented in their files. By Census division, the highest percentage (87.8%) of residents who had an advance directive were located in the Mountain division, followed by residents in East North Central (83.7%), New England (80.0%), West North Central (78.9%), Pacific (77.6%), South Atlantic (77.4%), East South Central (76.4%), Middle Atlantic (68.8%), and West South Central (64.9%).
Source: National Center for Health Statistics, National Study of Long-Term Care Providers, 2016. https://www.cdc.gov/nchs/nsltcp/index.htm.
Reported by: Jessica Penn Lendon, PhD, jlendon@cdc.gov, 301-458-4714; Christine Caffrey, PhD; Denys T. Lau, PhD.
Suggested citation for this article: QuickStats: Percentage of Residential Care Community Residents with an Advance Directive, by Census Division — National Study of Long-Term Care Providers, 2016. MMWR Morb Mortal Wkly Rep 2018;67:790. DOI: http://dx.doi.org/10.15585/mmwr.mm6728a7.
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (https://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.