Campylobacter jejuni Infections Associated with Raw Milk Consumption — Utah, 2014
Weekly / April 1, 2016 / 65(12);301–305
Kenneth R. Davis, MPH1; Angela C. Dunn, MD2; Cindy Burnett, MPH1; Laine McCullough1; Melissa Dimond, MPH1; Jenni Wagner, MS3; Lori Smith3; Amy Carter4; Sarah Willardson, MPH5; Allyn K. Nakashima, MD1 (View author affiliations)
View suggested citationSummary
What is already known about this topic?
Raw milk can contain dangerous bacteria and is a common source of milkborne disease–related outbreaks. Campylobacter jejuni is a common raw milk contaminant and is notoriously difficult to isolate from food products, because of its fastidious growth requirements.
What is added by this report?
A total of 99 cases (59 confirmed and 40 probable) of campylobacteriosis, including 10 patients who were hospitalized, and one who died, occurred in an outbreak in northern Utah associated with a single raw milk dairy. The outbreak was documented by epidemiologic, environmental, and laboratory evidence. Despite routine testing of raw milk showing results within acceptable limits, the milk still contained dangerous bacteria.
What are the implications for public health practice?
Public health departments can consider adding ongoing education of the public regarding the risks from raw milk consumption and unreliability of some current safety testing. To limit outbreaks from raw milk consumption, more reliable routine tests are needed that do not rely solely on bacterial, coliform, and somatic cell counts. Case investigation and pulsed-field gel electrophoresis patterns from environmental samples can support an epidemiologic link and allow implementation of control measures.
In May 2014, the Utah Public Health Laboratory (UPHL) notified the Utah Department of Health (UDOH) of specimens from three patients infected with Campylobacter jejuni yielding indistinguishable pulsed-field gel electrophoresis (PFGE) patterns. All three patients had consumed raw (unpasteurized and nonhomogenized) milk from dairy A. In Utah, raw milk sales are legal from farm to consumer with a sales permit from the Utah Department of Agriculture and Food (UDAF). Raw milk dairies are required to submit monthly milk samples to UDAF for somatic cell and coliform counts, both of which are indicators of raw milk contamination. Before this cluster’s identification, dairy A’s routine test results were within acceptable levels (<400,000 somatic cells/mL and <10 coliform colony forming units/mL). Subsequent enhanced testing procedures recovered C. jejuni, a fastidious organism, in dairy A raw milk; the isolate matched the cluster pattern. UDAF suspended dairy A’s raw milk permit during August 4–October 1, and reinstated the permit when follow-up cultures were negative. Additional cases of C. jejuni infection were identified in October, and UDAF permanently revoked dairy A’s permit to sell raw milk on December 1. During May 9–November 6, 2014, a total of 99 cases of C. jejuni infection were identified. Routine somatic cell and coliform counts of raw milk do not ensure its safety. Consumers should be educated that raw milk might be unsafe even if it meets routine testing standards.
Outbreak Investigation
On May 21, 2014, UPHL notified UDOH of three laboratory-confirmed cases (in patients A, B, and C) of C. jejuni infection with indistinguishable SmaI PFGE patterns (DBRS16.0196). Campylobacter infection is a reportable disease in Utah, and all Campylobacter isolates undergo PFGE analysis (1). Patients A and B were a parent and child who had illness onset on May 10, and both were hospitalized. Patient A died 1 week later of multisystem organ failure, related, in part, to gastroenteritis and underlying medical conditions. Patient C’s symptoms began on May 11. All three patients reported raw milk consumption from dairy A in Weber County, in northern Utah (Figure 1). Additional cases were identified during May and June; UDOH initiated an outbreak investigation on June 10. A confirmed case was defined as the onset of diarrheal illness caused by C. jejuni matching the cluster PFGE pattern or confirmed Campylobacter infection on or after May 1 in a person who had consumed dairy A raw milk 1–10 days before illness onset. A probable case was defined as the onset of diarrheal illness on or after May 1 in a person who had consumed raw milk from dairy A 1–10 days before illness onset, or who reported contact with a patient who met the confirmed case definition.
During May 9–November 6, a total of 99 cases (59 confirmed and 40 probable) of C. jejuni infection were identified through laboratory isolates and patient interviews (Figure 2). Eighty-five (86%) patients resided in three northern Utah counties (Weber, Davis, and Salt Lake) in the vicinity of dairy A; 34 cases were reported from Weber County, 33 from Davis County, and 18 from Salt Lake County. An additional 14 cases were reported from other northern Utah counties (Figure 1). Patients ranged in age from 1 to 74 years (median = 23 years); 44 patients were aged <18 years. Reported signs and symptoms were consistent with campylobacteriosis. All 99 patients reported diarrhea; among 84 patients with signs and symptoms available, the majority reported abdominal pain (65 patients) and fever (53). Although 15% of Utah residents and 17% of Weber County residents are Hispanic, a total of 31 cases (32%) occurred in Hispanics. Overall, 10 patients were hospitalized and one died (Table).
Exposure history was available for 98 patients. Among these patients, 53 reported drinking raw milk, including 52 who reported drinking raw milk from dairy A. Entries in dairy A’s raw milk sales ledger during May 1–July 27 documented raw milk purchase by 38 (39%) identified patients, among whom 20 (53%) reported consuming raw milk from dairy A; an additional four (11%) patients reported raw milk consumption but could not recall the dairy’s name. The remaining 14 (37%) patients who purchased raw milk from dairy A did not report consuming raw milk. Among 41 patients with no known raw milk consumption, 21 (51%) reported eating queso fresco, a Mexican-style cheese. Among the patients who reported eating queso fresco, 19 (90%) were Hispanic; however, no common source was identified.
UDAF inspectors visited dairy A on a routine inspection on June 1, before being notified about the outbreak, and on two subsequent outbreak-related inspections on June 12 and July 13. Dairy A passed these inspections with no critical violations noted. During June 1–July 13, three raw milk samples were collected and tested by UDAF for somatic cell and coliform counts. Because no pathogens were detected in the samples, the dairy continued selling raw milk.
Cases of C. jejuni infection continued to be identified, and on July 29, representatives from UDOH, UDAF, and UPHL conducted a collaborative investigation at dairy A. Following the Food and Drug Administration’s Bacteriological Analytical Manual protocol (2), the raw milk bulk tank was agitated, and a UDAF inspector collected a 1-liter sample of raw milk. The sample was neutralized on-site to a pH of 7.5 by a UPHL microbiologist and sent to UPHL and UDAF laboratories for testing. The milk was cultured concurrently at UPHL and UDAF using the selective medium, sheep blood agar. Both UPHL and UDAF isolated C. jejuni; PFGE performed by UPHL identified the same pattern identified in specimens from the initial three patients. UDAF tested samples for somatic cell and coliform counts adhering to regulations set forth by the Utah Dairy Act; counts were within the acceptable range despite the positive culture (3). UPHL tested 56 human Campylobacter isolates related to the outbreak. The isolates were enriched in accordance with the Bacteriological Analytical Manual protocol for Campylobacter culture (2). As is routine in Utah, all samples were analyzed for serotype and SmaI PFGE. Fifty-five of 56 isolates produced indistinguishable PFGE patterns by SmaI (DBRS16.0196) and KpnI (DBRK02.0190). One sample was identified as SmaI PFGE pattern (DBRS16.2505); this pattern is 87% similar to the outbreak pattern, and the patient from whom the isolate was obtained reported having contact with a patient with confirmed C. jejuni infection and having consumed raw milk from dairy A.
Public Health Response
On August 4, after finding positive C. jejuni cultures, UDAF suspended dairy A’s permit to sell raw milk. On August 26, UDOH and UDAF issued a joint press release to inform the public about the outbreak, educate Utah citizens about the dangers of raw milk consumption, and notify them of dairy A raw milk as the outbreak source. The press release led to the identification of one additional probable case.
UDAF reinstated dairy A’s permit to sell raw milk on October 1 after acceptable somatic cell and coliform counts and negative Campylobacter cultures were reported during retesting. However, during October 1–November 4, seven additional cases of C. jejuni infection were identified, and on December 1, UDAF permanently revoked dairy A’s raw milk sales permit. No cases of C. jejuni infection were identified from November 4, 2014, through February 2015. However, after the outbreak investigation concluded and dairy A was no longer selling raw milk, a person with campylobacteriosis matching the outbreak pattern was identified on February 19, 2015. This person did not report drinking raw milk. No campylobacteriosis cases matching the outbreak pattern have been identified since February 19, 2015.
Discussion
An estimated 3% of the U.S. population drinks raw milk, and prefer it to pasteurized milk, in part, because of perceived health benefits of raw milk consumption (4,5). Raw milk can be contaminated with Campylobacter in different ways. Campylobacter is ubiquitous in the dairy environment. Fecal matter contamination, wild bird droppings, poorly sanitized milking equipment, contamination during repair of milking machines, and silent mastitis are among documented contamination routes reported during previous outbreaks (6–9). Campylobacter is a fragile organism and is notoriously difficult to culture from milk; documented outbreaks in which human cases of Campylobacter infection have been linked by PFGE to raw milk are rare. In this outbreak, immediate on-site pH neutralization and use of selective media enhanced recovery of Campylobacter from raw milk, and laboratory and epidemiologic evidence were both necessary to document ongoing illnesses from the milk, which led UDAF to permanently revoke dairy A’s permit.
Routine testing of and standards for raw milk (somatic cell and coliform counts) do not ensure that the raw milk is free of pathogens (8). As required by Utah regulation, dairy A submitted raw milk samples to UDAF for bacterial and coliform counts every 4 weeks. These counts continually yielded acceptable results before and throughout the outbreak investigation. Previous studies have demonstrated a lack of correlation between bacterial counts and presence of pathogens in raw milk (9,10). Mandatory reporting, timely sample collection, pathogen testing, and on-site milk neutralization likely led to C. jejuni detection during this outbreak. Specific pathogen testing for raw milk, in addition to somatic cell and coliform counts, might more readily detect contaminated raw milk. PFGE patterns linking human isolates from Campylobacter cases with raw milk from dairy A provided evidence that led to implementation of control measures.
Consumers should be aware of dangers associated with consuming unpasteurized milk. Current raw milk testing standards do not readily detect contamination; thus, the safest alternative is to consume pasteurized milk.
Acknowledgments
Cody Huft, Utah Department of Agriculture and Food; Steven L. Wright, Sushma Karna, Dairy Testing Laboratory, Laboratory Services Division, Utah Department of Agriculture and Food; state and local enteric disease investigators from Weber-Morgan, Davis County, Salt Lake County, Bear River, Tri-County, Summit County, and Utah County Health Departments.
1Utah Department of Health; 2Epidemic Intelligence Service, CDC; 3Utah Public Health Laboratory; 4Weber-Morgan Health Department, Utah; 5Davis County Health Department, Utah. Corresponding author: Kenneth R. Davis, krdavis@utah.gov, 801-538-6205.
References
- Utah Department of Health. Health, disease control and prevention, epidemiology. Communicable disease rule; R386–702. Salt Lake City, UT: Utah Department of Health; 2016. http://www.rules.utah.gov/publicat/code/r386/r386-702.htm
- Tan JM, Abeyta C, Tran T. Campylobacter. Bacteriological analytical manual. Silver Spring, MD: US Department of Health and Human Services, Food and Drug Administration; 2016. http://www.fda.gov/Food/FoodScienceResearch/LaboratoryMethods/ucm2006949.htm
- Utah Department of Agriculture. Utah dairy act. 2010. Chapter 3. Salt Lake City, UT: Utah Department of Agriculture; 2013. http://le.utah.gov/xcode/Title4/Chapter3/C4-3_1800010118000101.pdf
- CDC. Foodborne diseases active surveillance network (FoodNet) population survey atlas of exposures, 2006–2007. Atlanta, GA: US Department of Health and Human Services, CDC; 2011. http://www.cdc.gov/foodnet/PDFs/FNExpAtl03022011.pdf
- Katafiasz AR, Bartlett P. Motivation for unpasteurized milk consumption in Michigan, 2011. Food Prot Trends 2012;32:124–8.
- Schildt M, Savolainen S, Hänninen ML. Long-lasting Campylobacter jejuni contamination of milk associated with gastrointestinal illness in a farming family. Epidemiol Infect 2006;134:401–5 . CrossRef PubMed
- Black RE, Levine MM, Clements ML, Hughes TP, Blaser MJ. Experimental Campylobacter jejuni infection in humans. J Infect Dis 1988;157:472–9. CrossRef PubMed
- Humphrey TJ, Beckett P. Campylobacter jejuni in dairy cows and raw milk. Epidemiol Infect 1987;98:263–9. CrossRef PubMed
- Heuvelink AE, van Heerwaarden C, Zwartkruis-Nahuis A, et al. Two outbreaks of campylobacteriosis associated with the consumption of raw cows’ milk. Int J Food Microbiol 2009;134:70–4. CrossRef PubMed
- Bianchini V, Borella L, Benedetti V, et al. Prevalence in bulk tank milk and epidemiology of Campylobacter jejuni in dairy herds in Northern Italy. Appl Environ Microbiol 2014;80:1832–7. CrossRef PubMed
 FIGURE 1. Location of dairy A and distribution of Campylobacter jejuni cases, by local health department district — Utah, May–November 2014
FIGURE 1. Location of dairy A and distribution of Campylobacter jejuni cases, by local health department district — Utah, May–November 2014
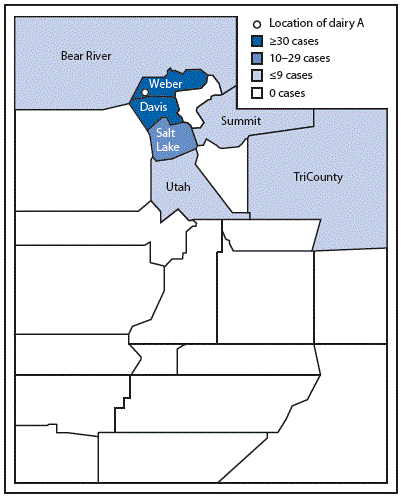
 FIGURE 2. Week of illness onset among patients (N = 99) with probable and confirmed Campylobacter jejuni infection associated with consumption of raw milk from a dairy — Utah, May–November 2014
FIGURE 2. Week of illness onset among patients (N = 99) with probable and confirmed Campylobacter jejuni infection associated with consumption of raw milk from a dairy — Utah, May–November 2014
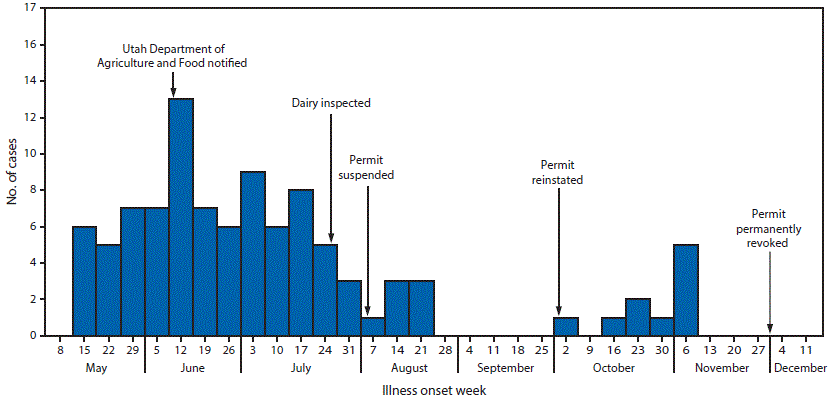
 TABLE. Demographic and clinical characteristics for 99 patients with Campylobacter jejuni infection associated with consumption of raw milk from a dairy — Utah, May–November 2014
TABLE. Demographic and clinical characteristics for 99 patients with Campylobacter jejuni infection associated with consumption of raw milk from a dairy — Utah, May–November 2014
| Characteristic | No. (%) |
|---|---|
| Sex (n = 97) | |
| Male | 57 (59) |
| Female | 40 (41) |
| Hispanic ethnicity (n = 98) | |
| Non-Hispanic | 67 (68) |
| Hispanic | 31 (32) |
| Age group (yrs) (n = 99) | |
| 0–5 | 11 (11) |
| 6–18 | 29 (29) |
| ≥19 | 48 (48) |
| Unknown | 11 (11) |
| Signs and symptoms (n = 84*) | |
| Abdominal pain | 65 (77) |
| Fever | 53 (63) |
| Nausea | 41 (49) |
| Vomiting | 36 (43) |
| Bloody diarrhea† | 35 (42) |
| Outcome (N = 99) | |
| Hospitalized | 10 (10) |
| Died | 1 (1) |
* Patients for whom information was available.
† All 99 patients reported diarrhea.
Suggested citation for this article: Davis KR, Dunn AC, Burnett C, et al. Campylobacter jejuni Infections Associated with Raw Milk Consumption — Utah, 2014. MMWR Morb Mortal Wkly Rep 2016;65:301–305. DOI: http://dx.doi.org/10.15585/mmwr.mm6512a1.
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (https://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.