Key points
- Leprosy is diagnosed based on clinical presentation, and the diagnosis is confirmed by skin or nerve biopsy and acid-fast staining.
- In the United States, the National Hansen’s Disease Program can provide diagnostic services.
- Leprosy is a reportable condition to state or local health departments.
Arranging diagnostic testing
In the United States, the National Hansen’s Disease Program can provide diagnostic services.
Healthcare providers should seek prompt consultation with National Hansen's Disease Program. Phone 1-800-642-2477, weekdays 9 AM to 5:30 PM ET (in Hawaii: 1-808-733-9831).
Recommended specimens
Depending on the form of leprosy the treating physician suspects, the following specimens may be collected:
- Skin smears from the earlobes, elbows, and knees
- Skin biopsy from edges of active patches
- Nerve biopsy from thickened nerves
Recommended tests
Skin and nerve biopsy
Biopsies are needed to definitively diagnose and classify leprosy. Slit skin smear may also be helpful in diagnosing those with multibacillary (MB) leprosy.
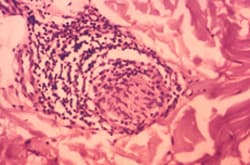
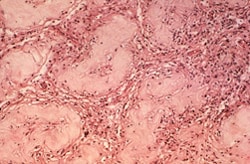
In MB leprosy, biopsying tissue from various affected sites may reveal typical histopathologic changes and large numbers of foam cells. Foam cells are macrophages that have ingested M. leprae or M. lepromatosis bacteria but are unable to digest the organisms. The M. leprae bacteria multiply and use the macrophage as a method of transport throughout the body. This is how the bacteria cause the multiple lesions that appear in all parts of the body on MB leprosy patients.
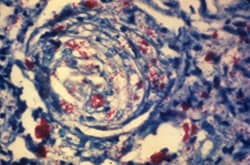
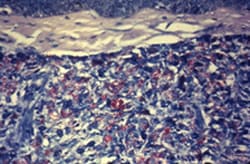
Acid-fast staining
Laboratory workers should use the Ziehl-Neelson method using 5% sulfuric acid as decolorizing agent. The presence of acid-fast bacilli confirms the diagnosis of leprosy.
Polymerase Chain Reaction (PCR) Testing
PCR testing can detect genetic material from M. leprae and M. lepromatosis in a skin biopsy. PCR may be useful when clinical and histopathologic findings are unclear. PCR does not replace routine diagnostic methods but can provide supportive evidence for leprosy, particularly in early or paucibacillary cases. PCR testing for leprosy is available only in specialized laboratories, including the National Hansen's Disease Program.
Reporting cases
Leprosy cases must be reported to jurisdictions when identified by a healthcare provider, hospital, or laboratory. Specific reporting requirements may vary by jurisdiction.
