Cancer Incidence Among African American People, United States—2007–2016
U.S. Cancer Statistics Data Briefs, No. 15
February 2020
This data brief uses the most recent data available at the time of publication. More recent data may be available in a newer data brief or in the U.S. Cancer Statistics Data Visualizations tool.
In 2016, African American men had disproportionately high cancer incidence rates compared with other men, and African American women had the second highest cancer incidence rates, behind White women.
Most Common Cancers
Among African American females, three cancer types (breast, lung, and colorectal) made up more than half of all new cancer cases. Cancers of the uterus, pancreas, kidney, thyroid, ovary, cervix, non-Hodgkin lymphoma, and myeloma made up a little less than a third.
Among African American males, prostate cancer accounted for a third of new cancer cases, lung and colorectal cancers made up a quarter of new cases, and cancers of the kidney, liver, pancreas, bladder, oral cavity/pharynx, and non-Hodgkin lymphoma and myeloma made up another quarter.
Figure 1. Number of New Cancer Cases Among African American People, 2016
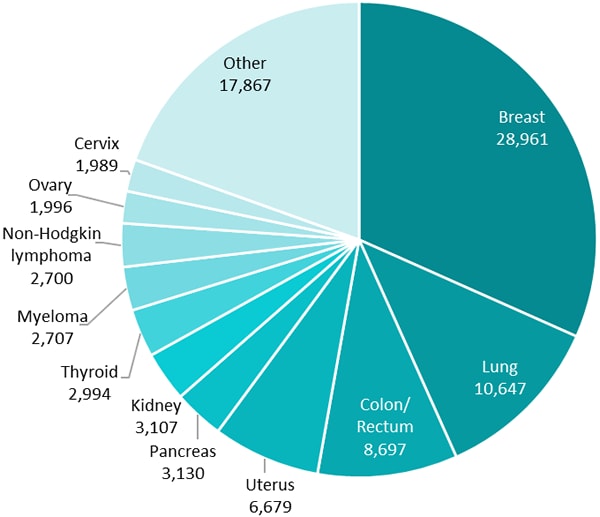
| Site | Cases | Percentage |
|---|---|---|
| Breast | 28,961 | 32% |
| Lung | 10,647 | 12% |
| Colon/Rectum | 8,697 | 10% |
| Uterus | 6,679 | 7% |
| Pancreas | 3,130 | 3% |
| Kidney | 3,107 | 3% |
| Thyroid | 2,994 | 3% |
| Myeloma | 2,707 | 3% |
| Non-Hodgkin lymphoma | 2,700 | 3% |
| Ovary | 1,996 | 2% |
| Cervix | 1,989 | 2% |
| Other | 17,867 | 20% |
| All Sites | 91,474 |
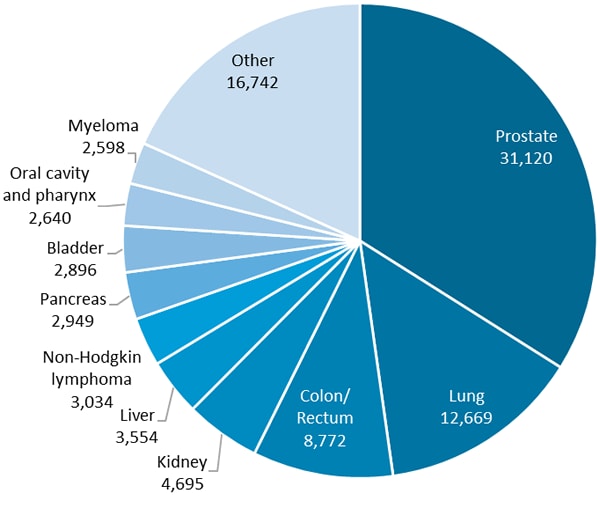
| Site | Cases | Percentage |
|---|---|---|
| Prostate | 31,120 | 34% |
| Lung | 12,669 | 14% |
| Colon/Rectum | 8,772 | 10% |
| Kidney | 4,695 | 5% |
| Liver | 3,554 | 4% |
| Non-Hodgkin lymphoma | 3,034 | 3% |
| Pancreas | 2,949 | 3% |
| Bladder | 2,896 | 3% |
| Oral cavity and pharynx | 2,640 | 3% |
| Myeloma | 2,598 | 3% |
| Other | 16,742 | 18% |
| All Sites | 91,669 |
Differences by Year of Diagnosis
Among African American females, uterine cancer incidence rates went up from 2007 to 2016, while lung and colorectal cancer incidence rates went down, and breast cancer incidence rates stayed about the same. Among African American males, incidence rates of prostate, lung, and colorectal cancer went down from 2007 to 2016, but kidney cancer incidence rates went up. Changes in incidence rates could be due in part to changes in risk factors or changes in screening test use.
Figure 2. Change in Ratesa of Common Cancers Among African American People During 2007 to 2016
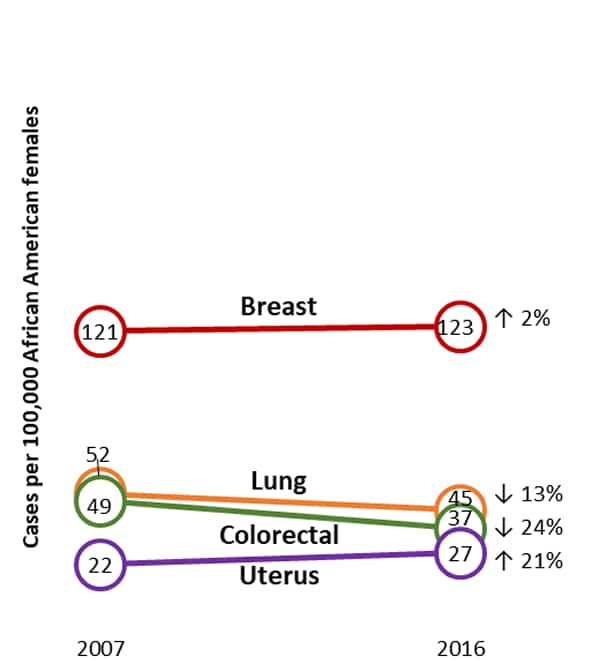
| Cancer | 2007 | 2016 | Change |
|---|---|---|---|
| Breast | 121 | 123 | 2% |
| Lung | 52 | 45 | 13% |
| Colorectal | 49 | 37 | 24% |
| Uterus | 22 | 27 | 21% |
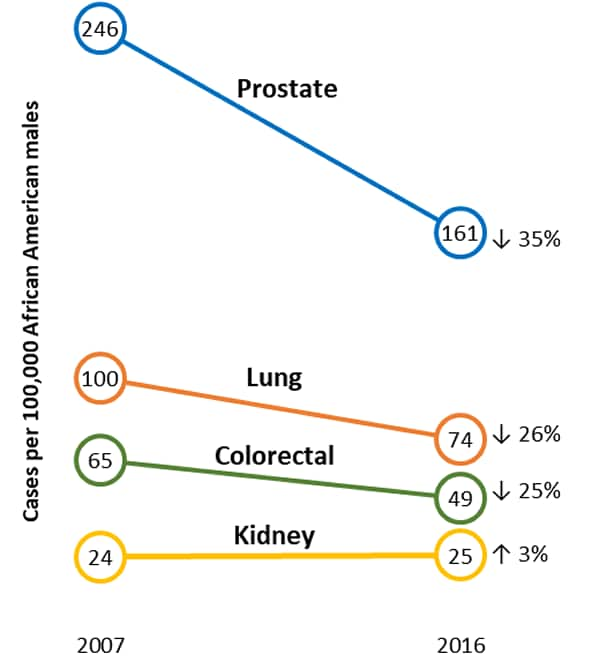
| Cancer | 2007 | 2016 | Change |
|---|---|---|---|
| Prostate | 246 | 161 | 35% |
| Lung | 100 | 74 | 26% |
| Colorectal | 65 | 49 | 25% |
| Kidney | 24 | 25 | 3% |
aRates are per 100,000 and age-adjusted to the 2000 US standard population.
The change in rates was calculated as the total percentage change from the rate in 2007 to the rate in 2016.
Differences by Sex, Age, and Cancer Type
| Female | Male | Total | |
|---|---|---|---|
| All cancer sites | 388.5 | 499.8 | 433.2 |
| Age group (years) | |||
| <20 | 12.5 | 15.0 | 13.7 |
| 20–49 | 202.8 | 120.9 | 164.0 |
| 50–64 | 771.0 | 1,028.7 | 888.3 |
| ≥65 | 1,523.1 | 2,334.8 | 1,849.7 |
| Screening-amenable cancers | |||
| Colon and rectum | 37.2 | 49.1 | 42.2 |
| Lung and bronchus | 45.2 | 73.9 | 57.0 |
| Female breast | 122.6 | ||
| Cervix | 8.7 | ||
| Vaccine-preventable cancersb | |||
| HPV-associated cancers | 13.1 | 9.1 | 11.2 |
| Liver | 5.4 | 17.2 | 10.6 |
| Cancers related to select risk factorsc | |||
| Cancers related to tobacco use | 147.1 | 243.4 | 187.2 |
| Cancers related to excess body weight | 220.9 | 129.0 | 181.1 |
aRates are per 100,000 and age-adjusted to the 2000 US standard population.
bHPV-associated cancers: carcinoma of the cervix and squamous cell carcinomas of the vagina, vulva, penis, anus (and rectum), and oropharynx; these rates include all cancer types related to HPV but do not estimate what proportion of these cancers were attributable to HPV. Liver cancer is related to hepatitis virus; all liver cancers are included, not just those attributable to hepatitis virus.
cCancers related to tobacco use: oral cavity and pharynx, esophagus, stomach, colon and rectum, liver, pancreas, larynx, lung, bronchus and trachea, cervix, kidney and renal pelvis, urinary bladder, and acute myeloid leukemia. Cancers related to excess body weight: adenocarcinoma of the esophagus, gastric cardia, colon and rectum, liver, gallbladder, pancreas, postmenopausal female breast, uterus, ovary, kidney, thyroid, meningioma, and multiple myeloma. These rates include all the cancer types related to tobacco use or excess weight but do not estimate what proportion of these cancers were attributable to tobacco use or excess weight.
Screening tests are recommended for breast, colorectal, and cervical cancers for persons at average risk, and lung cancer for persons at high risk, which can help detect these cancers early. Colorectal and cervical cancer screening tests can also detect precancerous lesions that can be removed before they turn into cancer.
Vaccines also help lower cancer risk. The human papillomavirus (HPV) vaccine helps prevent most cervical cancers and several other kinds of cancer. The hepatitis B vaccine can help lower liver cancer risk.
Proven community-based strategies can make it easier for people to avoid tobacco and tobacco smoke, engage in physical activity, and eat healthy foods, decreasing their risk of several types of cancer.
Public health and community leaders can work together to support culturally competent cancer prevention and control efforts. These can make it easier for people to get appropriate cancer screening tests, get vaccines for cancer-causing viruses, avoid tobacco and tobacco smoke, engage in physical activity, and eat healthy foods to decrease their risk of several types of cancer.
Data Sources
Data in this brief come from U.S. Cancer Statistics, the official federal cancer statistics.
U.S. Cancer Statistics incidence data are from population-based registries that participate in CDC’s National Program of Cancer Registries (NPCR) and/or the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program and meet high-quality data for the November 2018 data submission, covering 100% of the U.S. population.
Centers for Disease Control and Prevention. Cancer Incidence Among African American People, United States—2007–2016. USCS Data Brief, no. 15. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2020.