Military Service Members and Veterans
Service members and military veterans have higher rates of tobacco product use than civilians. Cigarette smoking is more common among Service members who have been deployed overseas. Cigarette smoking increases your risk for lung cancer, heart disease, chronic bronchitis, and many other diseases.
- Many Service members start using tobacco after they enter military service.
- During 2010–2015, more than 1 in 5 (21.6%) veterans in the United States reported current cigarette smoking.1 In 2018, 14.6% of veterans enrolled for care reported current cigarette smoking.2
In addition to adversely affecting their health, the high prevalence of tobacco use among military and veteran personnel also has a significant financial impact. In 2014, the Defense Department spent nearly $1.8 billion in medical and non-medical costs related to tobacco use.3 During 2010, Veterans Health Administration (VHA) spent an estimated $2.7 billion on smoking-related ambulatory care, prescription drugs, hospitalizations, and home health care.5
Learn what percentage of people currently smokes cigarettes, both in the United States overall and among specific population groups.
Start your quit journey by visiting a Quit Guide.
Call a quitline for free help to quit smoking:
- English: 1-800-QUIT-NOW (1-800-784-8669)
- Spanish: 1-855-DÉJELO-YA(1-855-335-3569)
- Military veterans with health insurance through the U.S. Department of Veterans Affairs (VA): 1-855-QUIT-VET (1-855-784-8838)
For free help quitting smoking through mobile text messages, text QUITNOW to 333888.
For help quitting smokeless tobacco: text “SPIT” to 333888.
- Know the Facts
- Get Help Quitting Tobacco
- Resources for Active Duty or Retired Service Members
- Service-Specific Resources and Programs
- Resources for Veterans Enrolled in the Veterans Affairs Health Care System
- Resources for Federal Employees Health Benefits (FEHB) Program Enrollees
- Real Stories: Military Service Members and Veterans in Tips®
- References

If you are an active duty or a retired Service member, you and your family may access quitting support through your TRICARE coverage and through Defense Department programs. If you are in the Reserve or National Guard, check out the resources below.
- The Defense Department’s YouCanQuit2 campaign has many resources to help people in the U.S. military quit tobacco use.
- Tobacco cessation services may be available to you through TRICARE, including counseling and medications to help you quit tobacco use.
- Find more information and resources about how to quit all forms of tobacco including smoking on the Tobacco-Free Living webpage of the Total Force Fitness website.
The YouCanQuit2 campaign has resources and tools to help you quit any form of tobacco. The interactive Quit Plan guides you step-by-step on how to quit tobacco. The Support Locator can help you find resources and programs to help you quit tobacco.
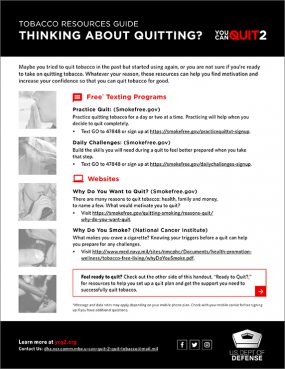
Find resources [PDF-794 KB] at the Defense Department’s YouCanQuit2 campaign to help motivate you and increase your confidence so you can quit tobacco for good.
Are you in the Air Force?
- Contact your local Military Treatment Facility (MTF) and/or Health Promotion team for local tobacco cessation resources.
Are you in the Army?
- Visit the Army Public Health Center to learn more about Tobacco-Free Living & Vaping.
Are you in the Navy?
- Find resources and tools to help you quit tobacco use through the Tobacco-Free Living program at the Navy and Marine Corps Public Health Center.
- You can also visit your local health promotion office or talk with your medical or dental provider at your military treatment facility.
- Use the Starter Kit to Quit Tobacco for tips, considerations, and actions if you use tobacco or are supporting someone who is quitting.
Are you in the Marine Corps?
- Learn more about the Operation Tobacco-Free Marine (OTFM) Tobacco Cessation Program.
- Visit your battalion aid station or talk with your local medical staff.
Are you in the US Coast Guard?
- Get more information from the Office of Work-Life Programs about the Tobacco Cessation Program.
If you are a veteran enrolled in the U.S. Department of Veterans Affairs (VA) health care system, you have access to VA resources and services to help you quit smoking. Smoking cessation counseling is available at all VA medical centers, and FDA-approved smoking cessation medications are available through all VA pharmacy programs. Use the Veterans Health Administration Facility Locator to find a VA health care facility near you.

- Visit The VA’s Tobacco and Health page to find information about:
- Quitting tobacco use.
- Cessation medications.
- Cessation counseling.
- Find tools, resources, and support to help you become tobacco-free at SmokefreeVET.
- Learn how nicotine replacement therapy can increase your chances of quitting.
- Enroll in text messaging cessation support at SmokefreeVET. Text VET to 47848 for support in English, or VETesp for support in Spanish.
- Call the VA National Quitline at 1-855-QUIT-VET (1-855-784-8838). Get more information about the VA national quitline.
- Contact your primary care team today to learn more about the resources that are available to help you quit tobacco use.
You have access to the FEHB plan tobacco cessation benefit if you are a federal employee whose Condition of Employment includes:
- Membership in a military unit and who has elected coverage in the FEHB Program.
- An activated federal employee eligible and is electing to maintain FEHB enrollment during military service.
- A Defense Department civilian employee electing coverage in the FEHB program.
- A veteran, who makes up about 30% of the federal workforce.4
- A family member included as a beneficiary under a FEHB enrollee.
The tobacco cessation benefit covers treatment for all forms of tobacco use, including cigarettes, electronic cigarettes, and smokeless tobacco. Because the combination of counseling and medication gives you the best chance of quitting successfully, the benefit covers:
- At least two quit attempts per year, and at least four tobacco cessation counseling sessions per quit attempt. These behavioral interventions include individual counseling, group counseling, and proactive telephone counseling.
- All FDA-approved tobacco cessation medications, including over-the-counter tobacco cessation medications, with a doctor’s prescription or as part of a plan-approved tobacco cessation program. This includes combination nicotine replacement therapy (NRT).
- These benefits are provided with no copayments or coinsurance and are not subject to deductibles or annual or life-time dollar limits.
For more information on how to access the benefit, please contact your health plan or consult your plan’s brochure.

Meet Beatrice R. Beatrice, age 40, lives in New York and formerly served in the U.S. Navy. She began smoking regularly at age 13. A mother of two, Beatrice quit smoking in 2010 because she wanted to be around for her family.

Meet Brian H. Brian lived in Texas and started smoking at age 8. He had a heart attack at age 35, was diagnosed with chronic obstructive pulmonary disease (COPD), and had bypass surgery, a heart transplant, lung cancer, and part of his lung removed due to smoking. Brian died at age 68 after suffering from smoking-related health problems for more than 30 years.
Meet Ethan B. Ethan, age 59, lives in California and started smoking menthol cigarettes regularly at age 18. He grew up seeing ads that made him think smoking cigarettes was “cool.” He suffered two strokes as a result of smoking.
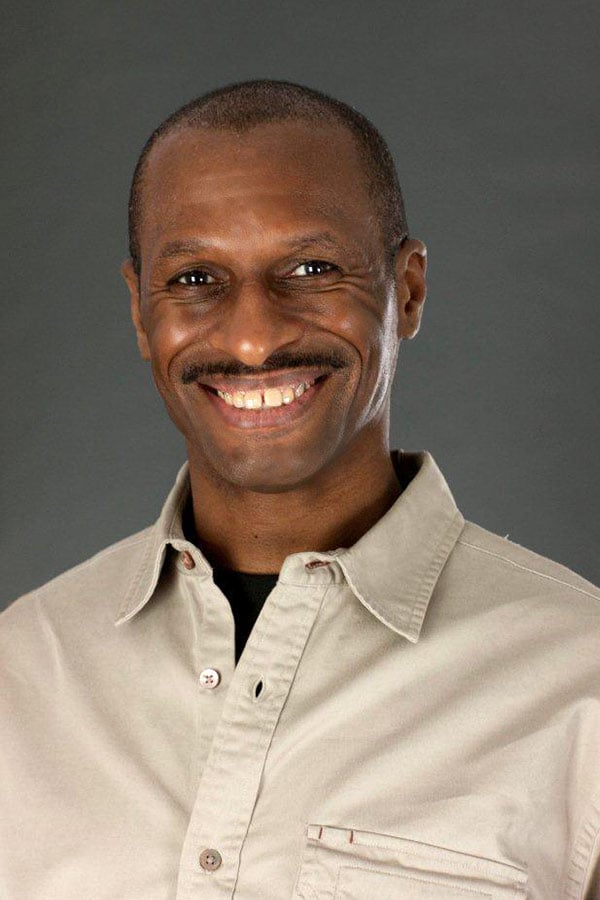
Meet James F. James, age 48, lives in New York and began smoking at age 14. He quit smoking in 2010 to reduce his risk for health problems and now bikes 10 miles every day.

Meet Mark A. Mark, age 47, lives in California and started smoking as a teenager. He continued smoking during military service in the Persian Gulf and in civilian life until he developed rectal cancer at age 42.
Meet Michael P. Michael lived in Alaska and began smoking at age 9. At age 44, he was diagnosed with chronic obstructive pulmonary disease (COPD), which makes it harder and harder to breathe and can cause death. Michael died at age 64.

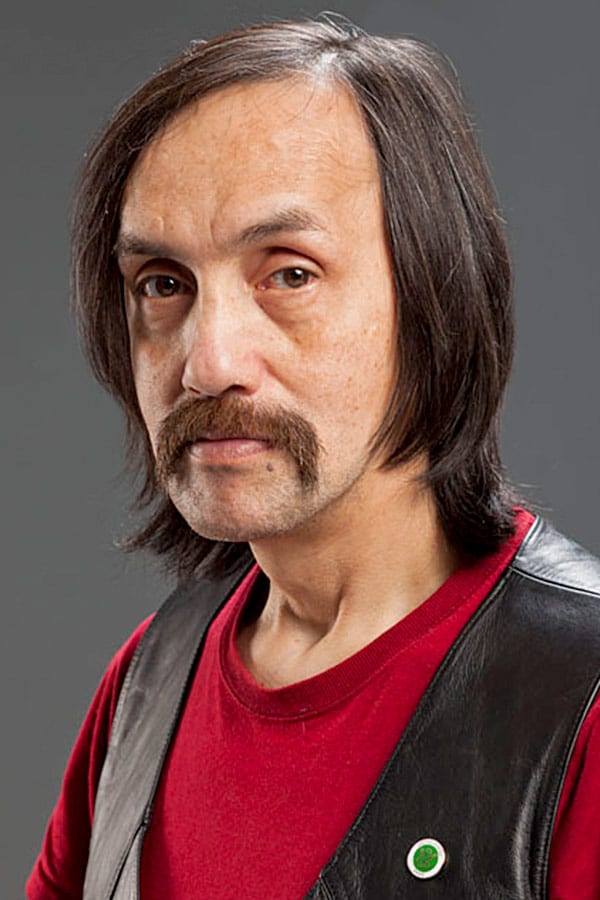
Meet Nathan M. Nathan, a member of the Oglala Sioux tribe, lived in Idaho. Exposure to secondhand smoke at work triggered asthma attacks so severe he had to leave his job. Nathan died at age 54 from lung damage caused by secondhand smoke exposure.
Learn more about all of the Tips participants in our Real Stories section.
- Centers for Disease Control and Prevention. Tobacco product Use among military veterans—United States, 2010–2015. MMWR. Morbidity and Mortality Weekly Report. 2018; 67:7–12.
- US Department of Veterans Affairs. 2018 Survey of Veteran Enrollees’ Health and Use of Healthcare Data Findings Report [PDF – 4.1 MB]. Washington, DC: US Department of Veterans Affairs; 2019.
- Lewin Group. Cost of Tobacco Use & Exposure, Overweight and Obesity, and High Alcohol Consumption within the TRICARE Prime and Standard Population: Technical Report., 2016.
- Office of Personnel Management. OPM Releases Veteran Employment Data. Washington, DC: Office of Personnel Management, 2017.
- Barnett PG, Hamlett-Berry K, Sung HY, Max W. Health care expenditures attributable to smoking in military veterans. Nicotine Tob Res. 2015;17(5):586-591.


