This is the first report in a new series of occasional MMWR reports entitled CDC Grand Rounds. These reports are based on grand rounds presentations at CDC on high-profile issues in public health science, practice, and policy. Information regarding CDC Grand Rounds is available at http://www.cdc.gov/about/grand-rounds.
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
CDC Grand Rounds: Current Opportunities in Tobacco Control
Tobacco use is the world's leading single preventable cause of death. Worldwide tobacco-related deaths now exceed 5 million a year. Left unchecked, the number is expected to exceed 8 million a year by 2030, and 80% of those tobacco-related deaths will occur in low- and middle-income countries (1,2). In the United States, tobacco use is the single leading preventable cause of disease, disability, and death. Each year, 443,000 U.S. residents die from cigarette smoking and exposure to secondhand smoke, and another 8.6 million have a serious illness caused by smoking (3). In 2008, 20.6% (approximately 46 million) of U.S. adults were current smokers (4). Smoking costs the United States $96 billion in medical costs and $97 billion in lost productivity annually (3). A particular concern is that progress in reducing smoking rates among young persons and adults has stalled. After a substantial decline from 1997 (36.4%) to 2003 (21.9%), the decline in smoking rates among high school students slowed and remained relatively unchanged from 2003 (21.9%) to 2007 (20.0%).* Adult smoking prevalence declined steadily from 1965 (42.4%) through the 1980s; however, the decline in smoking rates among adults began to slow in the 1990s and remained relatively unchanged from 2004 (20.9%) to 2008 (20.6%) (4). By achieving a modest decline in smoking prevalence worldwide (from 25% to 20%) through further use of tobacco control measures, 100 million deaths can be prevented by 2020 (1).
The World Health Organization (WHO) Framework Convention on Tobacco Control (FCTC), signed by 168 countries, went into effect in February 2005.† The treaty commits countries to protect the public's health by adopting various measures to reduce demand for tobacco. Those measures include increased pricing of tobacco products, protection from exposure to tobacco smoke, and efforts to educate the public and consumers about the health risks associated with tobacco use. They also include regulation of product contents, packaging, and advertising. To support that effort, the WHO MPOWER§ policy package outlines objectives and interventions countries can adopt to reduce the supply of and demand for tobacco products to combat global tobacco use (2).
In 2007, the Institute of Medicine (IOM) presented a blueprint for action to "reduce smoking so substantially that it is no longer a public health problem for our nation." IOM called for a two-pronged strategy to include 1) strengthening and fully implementing traditional evidence-based tobacco control measures, and 2) changing the regulatory landscape to permit federal regulation of tobacco product content, design, marketing, and distribution (5). Traditional evidence-based interventions that have had the most success include price increases, smoke-free policies that prohibit smoking in all indoor areas of workplaces and public places, aggressive media campaigns, access to cessation services, comprehensive advertising bans, and graphic warning labels on tobacco products.
Increasing the price of cigarettes discourages initiation among youths, prompts quit attempts, and reduces average cigarette consumption among those who continue to smoke (5). As tobacco prices go up, for example, consumption of tobacco products goes down (Figure 1). Evidence from the United States indicates that a 10% increase in the price reduces cigarette consumption by about 4% (6). Cigarette excise taxes increase cigarette prices, thereby reducing cigarette use and smoking-related death and disease. In 2009, the federal government, 14 states, and the District of Columbia (DC) increased cigarette excise taxes. On December 31, 2009, cigarette excise taxes among all states ranged from $0.07 a pack in South Carolina to $3.46 a pack in Rhode Island, with a national mean of $1.34 per pack (7). Although many countries have moderate taxes on tobacco products that comprise more than 30% of the sales price, inflation led to a decrease in the effect taxes had on the affordability of cigarettes over time (8).
Strong smoke-free policies substantially improve indoor air quality, reduce negative health outcomes among nonsmokers, decrease consumption, encourage smokers to quit, change social norms regarding the acceptability of smoking, and reduce the risk for cardiovascular disease (9). In 2007, only 11 countries had national laws prohibiting smoking in public places: Botswana, France, Iran, Ireland, Italy, New Zealand, Niger, Norway, Sweden, United Kingdom, and Uruguay (Figure 2) (8). Although on December 31, 2009, a total of 21 U.S. states and DC had comprehensive smoke-free laws in effect that prohibit smoking in workplaces, restaurants, bars, and other public places, about half of U.S. residents are not protected by comprehensive state or local smoke-free laws, and 12 states preempt local communities from passing smoke-free policies.¶
Sustained media campaigns, combined with other interventions, increase negative attitudes about smoking and the tobacco industry, decrease the likelihood of tobacco initiation among youth, and promote smoking cessation (6,10). Prominently displaying health warnings on tobacco packaging also has been effective in getting smokers to consider quitting. In Brazil, more than half of smokers surveyed said they changed their opinion about the health consequences of smoking and close to 70% said they wanted to quit as a result of new graphic warning labels (2).
The more states spend on comprehensive tobacco control programs, the greater the reductions in smoking, and the longer states invest in such programs, the greater the impact (10). States that invest heavily in comprehensive tobacco control have seen cigarette sales drop more than twice as much as the United States as a whole, and youth and adult smoking prevalence declines faster as spending for tobacco control programs increases (10--12). States that have sustained and coordinated tobacco control programs, such as Maine, New York, and Washington, have seen 45% to 60% reductions in youth smoking (10).
Full implementation of these traditional evidence-based strategies is essential to end the tobacco use epidemic in the United States. In 2002, after approximately a decade of unchanging smoking rates among adults and youths, New York City implemented a multipronged and comprehensive effort to reduce tobacco use that included 1) increasing tobacco taxes, 2) establishing a strong smoke-free policy, 3) implementing aggressive media campaigns, 4) providing free cessation services to smokers, and 5) rigorously evaluating the results. As a result of this effort, which combined multiple interventions, youth smoking rates were reduced by about 50% and adult smoking rates decreased from 21.6% in 2002 to 15.8% in 2008 (13).** The decline in adult smoking prevalence since 2002 is greater than that in the United States overall and represents 350,000 fewer smokers in New York City (Figure 3).
If all U.S. states annually funded comprehensive tobacco control programs at the levels CDC recommended in 2007 (between $9 and $18 per capita; or $3.7 billion nationally), in 5 years, an estimated 5 million fewer persons would smoke, and hundreds of thousands of premature tobacco-related deaths would be prevented (10). Approximately 15% of the $25.4 billion states received in 2009 from the Master Settlement Agreement†† and excise tax revenue would be needed to fully fund state tobacco control programs at CDC-recommended levels. However, less than 3% of this tobacco-generated revenue was dedicated to tobacco use prevention, and half the states were funded at less than 20% of CDC-recommended levels (14).
In addition to implementing and sustaining interventions, continued or enhanced high quality surveillance for exposure and disease is essential for monitoring progress and shortfalls and for ensuring that interventions have their desired effects. In 1999, WHO, CDC, and the Canadian Public Health Association developed the Global Tobacco Surveillance System (GTSS), the only worldwide surveillance effort tracking tobacco use among youth and adults. Global youth surveys have been completed in 163 countries. The Global Adult Tobacco Survey (GATS) is initially being implemented in 14 countries. Funding for GATS is provided by the Bloomberg Initiative to Reduce Tobacco Use. The Bill and Melinda Gates Foundation is providing funding for GATS in China and the African region.
In 2003, WHO created the Tobacco Laboratory Network of government, academic, and independent laboratories worldwide to strengthen national and regional capacity for testing and research of the contents and emissions of tobacco products, in accordance with Article 9 of the WHO FCTC. The Network's stated goals are to establish global capacity to test tobacco products for regulatory compliance, to research and develop harmonized standards for contents and emissions testing, to share tobacco research and testing standards and results, to inform risk assessment activities related to the use of tobacco products, and to develop harmonized reporting of results so that data can be transformed into meaningful trend information that can be compared across countries and over time.
Until enactment of the Family Smoking Prevention and Tobacco Control Act (Tobacco Control Act) §§ on June 22, 2009, the United States had no product standards for cigarettes or other tobacco products. Without standards, the tobacco industry could make unregulated changes to highly engineered products that appeal to youths and help maintain addiction (5). The design of a tobacco product substantially influences the levels of toxic chemicals it emits, as seen through the differences in levels of tobacco-specific nitrosamines that result from the use of different types of cigarettes in different countries (Figure 4) (15).
The Tobacco Control Act granted the Food and Drug Administration (FDA) authority to regulate tobacco products so that, without FDA's approval, existing products cannot be altered substantially and new products cannot be introduced. Additionally, the Tobacco Control Act prohibits the use of certain flavors, such as candy, fruit, and spices, in cigarettes. It also establishes a Tobacco Products Scientific Advisory Committee that will make reports and recommendations to FDA on the public health effects of menthol flavoring in cigarettes and the use of dissolvable tobacco products, and provide advice on other critical issues.
Under the Tobacco Control Act, FDA has authority to adopt tobacco product standards to protect the public's health, review and authorize the marketing of new and modified risk tobacco products, and regulate advertising and promotion of tobacco products. Information on ingredients in tobacco products and tobacco smoke must be submitted to FDA, which then uses this information as it implements various provisions of the Tobacco Control Act, such as when adopting a tobacco product standard. Additionally, as required by law, FDA will reissue a rule originally published in 1996, which establishes restrictions on youth access, and on advertising and promotion practices that are particularly attractive to youths. The rule prohibits the sale of cigarettes and smokeless tobacco to persons aged <18 years and imposes specific marketing, labeling, and advertising requirements.
Provisions of the Tobacco Control Act go into effect at different times. The prohibition against using characterizing flavors in cigarettes went into effect on September 22, 2009. The reissued regulation aimed at reducing access to and appeal of tobacco products to young persons will go into effect on June 22, 2010. Also on June 22, 2010, tobacco product manufacturers may no longer use the terms "light," "low," and "mild" in product labels, labeling, or advertising, and warning statements for smokeless tobacco products will be revised and strengthened. By late 2012, health warnings on cigarette packages and in advertising will include color graphics depicting the negative health consequences of smoking. FDA will use its enforcement authority to ensure that these important public health actions are followed.
The regulation of tobacco products is an important and critical component of an overall comprehensive tobacco prevention and control strategy that will not replace, but will strengthen, existing tobacco control efforts. Tobacco regulation offers opportunities for FDA to work as a partner in tobacco prevention and control, including through collaboration with CDC and other agencies providing expertise in surveillance, research, product design, and evaluation, and state tobacco control programs. In the future, continual evaluation of FDA-established product standards will be needed to measure their effect on the public's health. Effective product standards should protect the public's health by reducing risks to the population as a whole, increasing the likelihood that smokers will quit smoking, and increasing the likelihood that nonsmokers will not start smoking. Monitoring of these new tobacco prevention and control measures and their impact will require expansion of existing surveillance efforts.
Reported by
M Tynan, T Pechacek, PhD, M McKenna, MD, Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion; D Ashley, PhD, National Center for Environmental Health, CDC. L Deyton, MD, Center for Tobacco Products, Food and Drug Admin. P Briss, MD, T Popovic, MD, PhD, Office of the Director, CDC.
Acknowledgments
The report is based, in part, on contributions by G Promoff, MA, K McCall, MPH, D Shelton, MPH, J Francis, MPH, MBA, S Babb, MPH, and R Kaufmann, PhD, Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, CDC.
References
- Frieden T, Bloomberg M. How to prevent 100 million deaths from tobacco. Lancet 2007;369:1758--61.
- World Health Organization. WHO report on the global tobacco epidemic, 2008---the MPOWER package. Geneva, Switzerland: World Health Organization; 2008. Available at http://www.who.int/tobacco/mpower/mpower_report_full_2008.pdf. Accessed April 21, 2010.
- CDC. Smoking-attributable mortality, years of potential life lost, and productivity losses---United States, 2000--2004. MMWR 2008;57:1226--8.
- CDC. Cigarette smoking among adults and trends in smoking cessation---United States, 2008. MMWR 2009;58:1227--32.
- Institute of Medicine. Ending the tobacco problem: a blueprint for the nation. Washington, DC: The National Academies Press; 2007.
- The Task Force on Community Preventive Services. The guide to community preventive services: what works to promote health? New York, NY: Oxford University Press; 2005. Available at http://www.thecommunityguide.org/tobacco/tobacco.pdf. Accessed April 22, 2010.
- CDC. State cigarette excise taxes---United States, 2009. MMWR 2010;59:385--8.
- Mackay J, Eriksen M. The tobacco atlas. 3rd ed. Geneva, Switzerland: World Health Organization; 2008. Available at http://www.tobaccoatlas.org. Accessed April 23, 2010.
- CDC. The health consequences of involuntary exposure to tobacco smoke: a report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, CDC; 2006. Available at http://www.surgeongeneral.gov/library/secondhandsmoke/report. Accessed April 22, 2010.
- CDC. Best practices for comprehensive tobacco control programs---2007. Atlanta, GA: US Department of Health and Human Services, CDC, Office on Smoking and Health; 2007.
- Tauras JA, Chaloupka FJ, Farrelly MC, et. al. State tobacco control spending and youth smoking. Am J Public Health 2005;95:338--44.
- Farrelly MC, Pechacek TF, Thomas KY, Nelson D. The impact of tobacco control programs on adult smoking. Am J Public Health 2008;98:304--9.
- CDC. Decline in smoking prevalence---New York City, 2002--2006. MMWR 2007;56:604--8.
- Campaign for Tobacco-Free Kids. State tobacco revenue and prevention spending FY2000--FY2010. Washington, DC: Campaign for Tobacco-Free Kids; 2009. Available at http://www.tobaccofreekids.org/reports/settlements/FY2010/Tob%20Rev%20and%20Prev%20Spending.pdf. Accessed April 26, 2010.
- Ashley DL, Beeson MD, Johnson DR, et al. Tobacco-specific nitrosamines in tobacco from US brand and non-US brand cigarettes. Nicotine Tob Res 2003;5:323--31.
* CDC. Youth Risk Behavior Survey, 1991--2007. Available at http://www.cdc.gov/healthyyouth/yrbs/pdf/yrbs07_us_tobacco_use_trend.pdf.
† Additional information available at http://www.who.int/fctc/en.
§ MPOWER is an acronym derived from key elements of the policy package: Monitor tobacco use and prevention policies; Protect people from tobacco smoke; Offer help to quit tobacco use; Warn about the dangers of tobacco; Enforce bans on tobacco advertising, promotion, and sponsorship; and Raise taxes on tobacco. Additional information available at http://www.who.int/entity/tobacco/mpower/mpower_english.pdf.
¶ CDC. State Tobacco Activities Tracking and Evaluation (STATE) System. Available at http://www.cdc.gov/tobacco/statesystem.
** New York City Department of Health and Mental Hygiene data. Additional information available at http://www.nyc.gov/html/doh/html/pr2009/pr023-09.shtml (adult data) and http://www.nyc.gov/html/doh/html/pr2008/pr001-08.shtml (youth data).
†† In 1998, major U.S. cigarette manufacturers settled litigation brought against them through a master agreement with 46 states. Full text of the agreement is available at http://ag.ca.gov/tobacco/pdf/1msa.pdf.
§§ Family Smoking Prevention and Tobacco Control Act. Pub. L. No. 111-31 (June 22, 2009). Available at http://www.gpo.gov/fdsys/pkg/PLAW-111publ31/content-detail.html.
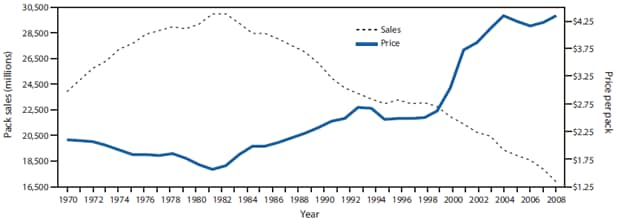
SOURCE: Chaloupka FJ. The economics of tobacco taxation. Chicago, IL: ImpacTEEN, University of Illinois at Chicago; 2009. Available at http://www.impacteen.org/generalarea_PDFs/Chaloupka_TobaccoTaxes_AK_041609.pdf.
* Adjusted to February 2009 dollars.
Alternate Text: The figure above shows cigarette sales and average price per pack for the United States from 1970-2008. According to the figure, as tobacco prices go up, consumption of tobacco products goes down. Evidence from the United States indicates that a 10% increase in the price reduces cigarette consumption by about 4%.
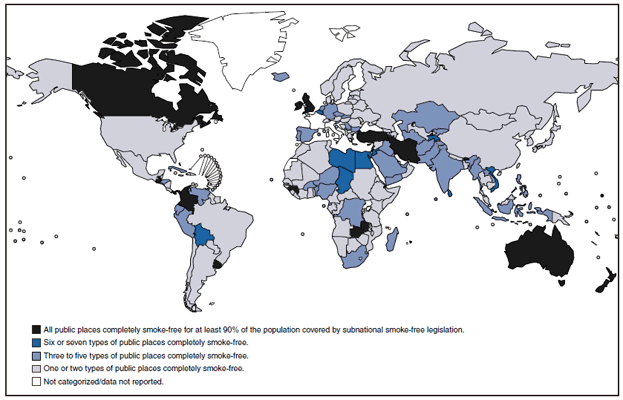
SOURCE: World Health Organization. WHO report on the global tobacco epidemic, 2009: implementing smoke-free environments. Geneva, Switzerland: WHO; 2009. Available at http://www.who.int/tobacco/mpower/en.
* Includes health-care facilities, universities and other educational facilities, government facilities, indoor offices, restaurants, pubs and bars, and public transport.
Alternate Text: The figure above shows countries with smoke-free public places in 2008, worldwide. In 2007, only 11 countries had national laws prohibiting smoking in public places: Botswana, France, Iran, Ireland, Italy, New Zealand, Niger, Norway, Sweden, United Kingdom, and Uruguay. In 2008, nearly all countries had local, state, or national laws making at least one or two public places completely smoke-free, and at least a dozen banned smoking in all public places for at least 90% of the population.
FIGURE 3. Percentage of current smokers among adults, 1994--2008, and high school students, 2001--2007 --- New York City
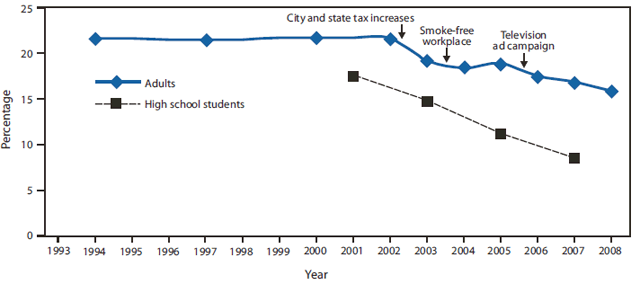
SOURCES: CDC. Decline in smoking prevalence---New York City, 2002--2006. MMWR 2007;56:604--8. New York City Department of Health and Mental Hygiene.
* Because of small sample sizes, data were grouped into 3-year averages during 1993--2001.
Alternate Text: The figure above shows the percentage of current smokers among adults, 1994-2008, and high school students, 2001-2007, in New York City. The decline in adult smoking prevalence since 2002 is greater than that in the United States overall and represents 350,000 fewer smokers in New York City.
FIGURE 4. Comparison of carcinogenic nitrosamine content of Marlboro and local* brand cigarettes --- eight countries, 2000--2001
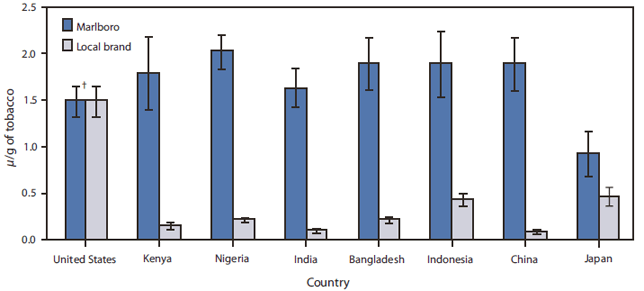
SOURCE: Ashley DL, Beeson MD, Johnson DR, et al. Tobacco-specific nitrosamines in tobacco from U.S. brand and non-U.S. brand cigarettes. Nicotine Tob Res 2003;5:323--31.
* Comparable, locally popular brand not distributed internationally.
† 95% confidence interval.
Alternate Text: The figure above shows the comparison of carcinogenic nitrosamine content of Marlboro and local brand cigarettes in eight countries, from 2000-2001. The design of a tobacco product substantially influences the levels of toxic chemicals it emits, as seen through the differences in levels of tobacco-specific nitrosamines that result from the use of different types of cigarettes in different countries. Except for the United States, local brands in those countries contained considerably less nitrosamine compared with Marlboro brand cigarettes.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


