Prevention Research Centers Collaborate with Rural Communities to Improve Health and Wellness
People living in rural areas have high rates of unhealthy behaviors like smoking and lack of physical activity, as well as less access to health care services and limited healthy foods options. These factors have been linked to high rates of heart disease, cancer, chronic lower respiratory disease, and strokes among rural residents.1
Working with rural communities to reduce these disparities presents unique challenges. Resources tend to be spread out, so people may have to travel a long way and they may not have good transportation. Less broadband access in some areas means that residents may have limited connectivity to learn about and access resources. PRCs have seen these health disparities in their own communities, and they are taking action.
- 50% of adults living in rural areas did not meet the federal guidelines for aerobic or muscle strengthening physical activities in 2018. 2
- 10% of households in rural areas experience food insecurity. 3
- 16% of rural adults did not visit a health care provider in the previous year. 4
- 19% of people in rural areas smoke cigarettes. 1
Addressing Rural Health Disparities
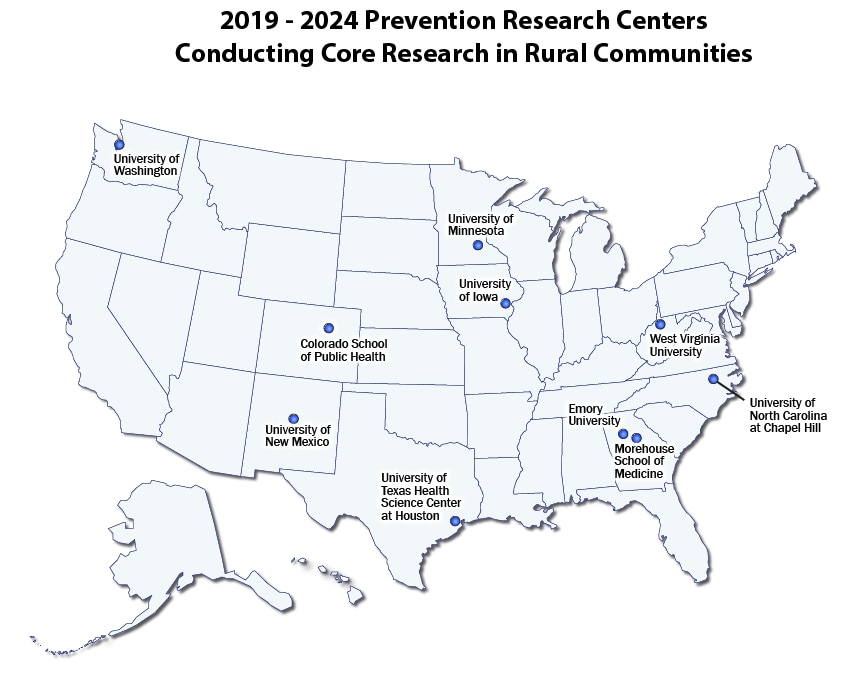
Many PRCs are working to expand access to health care, increase physical activity, decrease substance use, and address other health topics in rural America. In the 2019–2024 funding cycle, 10 PRCs are working to improve health in rural communities.
Examples of PRC work in rural communities from the 2019–2024 funding cycle.
Physical activity: Healthy Places-Healthy People
In New Mexico, 50% of American Indian/Alaska Native adults had obesity in 2021.5
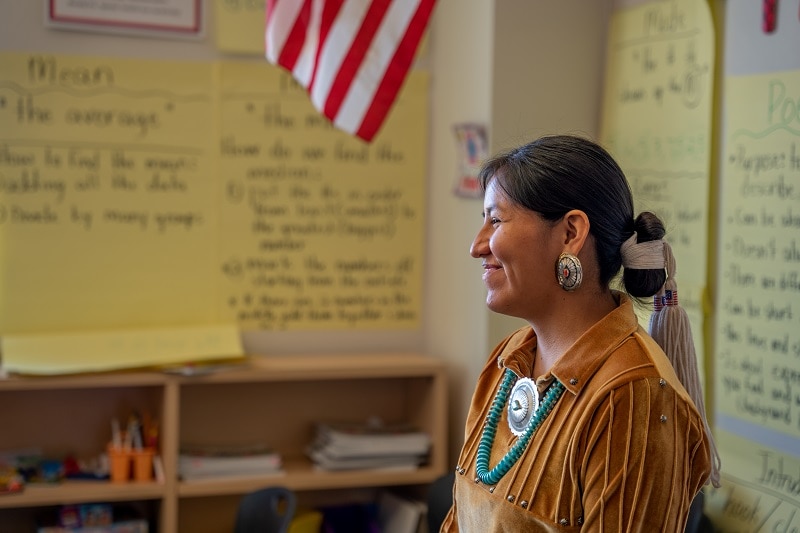
The University of New Mexico Prevention Research Center (UNM-PRC) is working on increasing access to and awareness of different ways to be physically active in 10 Navajo communities. The Healthy Places-Healthy People (HPHP) program uses the Community Guide physical activity recommendations to help communities become more physically active. Recommendations include constructing sidewalks, creating walking trails, and providing social support and outreach.
To support implementation of HPHP in Navajo communities, UNM-PRC provides health education, identifies resources, sponsors events, and creates maps and walking guides. The PRC invites local community members and students, faculty, and staff from Diné College and the Navajo Nation Technological University to participate in workshops, trainings, and the overall implementation and evaluation of HPHP. The UNM-PRC is working to expand the program by adapting it and developing a toolkit for implementation in other communities.
Healthy eating: Med-South Lifestyle Program
In 2021, less than one-third (30%) of adults in North Carolina met their recommended body mass index range.5
The University of North Carolina at Chapel Hill Center for Promotion and Disease Prevention (UNC-PRC) is researching the most effective ways to implement and expand the Med-South Lifestyle Program, an evidence-based intervention that promotes healthy eating and physical activity. The program applies Mediterranean-style cooking to traditional Southern recipes. It promotes whole grains, healthy fats, and vegetables that are proven to help prevent chronic diseases. UNC-PRC is researching the barriers and facilitators for wide-scale implementation, and based on those findings, plans to offer the program to rural, minority, low-income, and medically underserved communities throughout North Carolina.
Health care access: TALK: Toolkit for Adolescent Care
As of 2021, nearly half (47%) of rural counties in Minnesota did not have a sexual health clinic.6
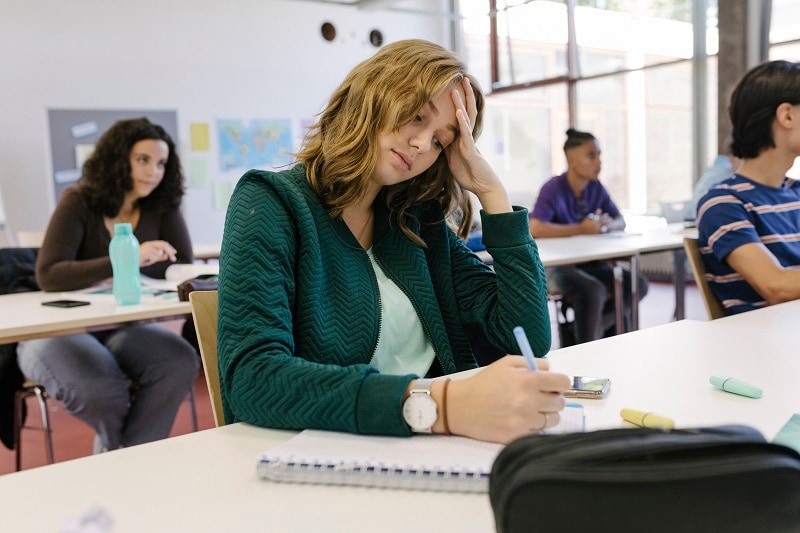
The University of Minnesota Healthy Youth Development Prevention Research Center (HYD-PRC) found that parents and teenagers want to talk with primary care providers about sexual health and psychosocial topics like substance use and mental health, but often don’t know how to have the conversation or lack the opportunity to do so.
HYD-PRC developed and is researching the effectiveness of TALK: Toolkit for Adolescent Care, a program for rural primary care clinics and clinicians to help them provide high-quality preventive care related to adolescent psychosocial and sexual health. The toolkit has three components:
- Clinician training on discussing sensitive topics with teens and parents.
- Tools for clinicians with information, resources, and talking points for discussions with parents.
- Suggestions for adolescent-friendly clinic practices, including one-on-one time between the clinician and adolescent and a “welcome to adolescent care” letter to parents and teens.
The goal of the toolkit is to help providers create a safe space to discuss sexual health and psychosocial topics with adolescents.
Substance use: The Integrated Community Engagement (ICE) Collaborative
In 2021, 50% of high school students in West Virginia reported trying e-cigarettes, and 28% reported currently using them.7
The West Virginia Prevention Research Center (WVPRC) is improving the representation of rural adolescents in data collection to better identify adolescent substance use in rural counties. WVPRC is partnering with local schools and coalitions in two rural counties—Wyoming and Fayette—to collect data on the prevalence of substance use and risk and protective factors among middle- and high school-aged youth in these rural communities. Based on these data, WVPRC will develop and implement appropriate interventions for youth in rural West Virginia.
- Cornelius ME, Loretan CG, Wang TW, Jamal A, Homa DM. Tobacco product use among adults – United States, 2020. MMWR Morb Mortal Wkly Rep. 2022;71(11):397-405. doi:10.15585/mmwr.mm7111a1
- Centers for Disease Control and Prevention. Table 25. Participation in leisure-time aerobic and muscle-strengthening activities that meet the federal 2008 Physical Activity Guidelines for Americans among adults aged 18 and over, by selected characteristics: United States, selected years 1998–2018 [PDF]. Available at https://www.cdc.gov/nchs/data/hus/2019/025-508.pdf [PDF – 158KB]. Accessed December 27, 2022.
- Rural Health Information Hub. Rural Hunger and Access to Healthy Food. Available at https://www.ruralhealthinfo.org/topics/food-and-hunger. Accessed December 27, 2022.
- National Center for Health Statistics. Percentage of having a doctor visit for any reason in the past 12 months for adults aged 18 and over, United States, 2019–2021. National Health Interview Survey. Generated interactively: May 16 2023 from https://wwwn.cdc.gov/NHISDataQueryTool/SHS_adult/index.html
- Centers for Disease Control and Prevention. BRFSS Prevalence & Trends Data. Available at https://nccd.cdc.gov/BRFSSPrevalence/rdPage.aspx?rdReport=DPH_BRFSS.ExploreByTopic&irbLocationType=StatesAndMMSA&islClass=CLASS14&islTopic=TOPIC09&islYear=2021&rdRnd=57824. Accessed December 28, 2022.
- Rural Health Information Hub. 2021 Minnesota Adolescent Sexual Health Report. Available at https://www.ruralhealthinfo.org/resources/18103. Accessed December 27, 2022.
- West Virginia Prevention Research Center. Substance Use. Available at https://prc.hsc.wvu.edu/projects/substance-use/. Accessed December 27, 2022.