Guidelines for Collecting and Handling Specimens for Mpox Testing
General Guidance
Review Biosafety Laboratory Guidance for Handling and Processing Mpox Specimens for recommended laboratory procedures and biosafety guidelines when collecting, handling, and processing specimens.
Specimen collection, storage, and shipping of human specimens are subject to Clinical Laboratory Improvement Amendments (CLIA) restrictions. Therefore, it is recommended to contact the laboratory testing facility to determine their specific requirements. See below guidance for suspected or confirmed mpox lesion collection, storage, packaging, and shipping.
For additional information:
Unroofing or aspiration of lesions (or otherwise using sharp instruments for mpox testing) is not necessary, nor recommended, due to the risk for sharps injury.
All recommended PPE should be worn when collecting a specimen from a person with suspected or confirmed mpox.
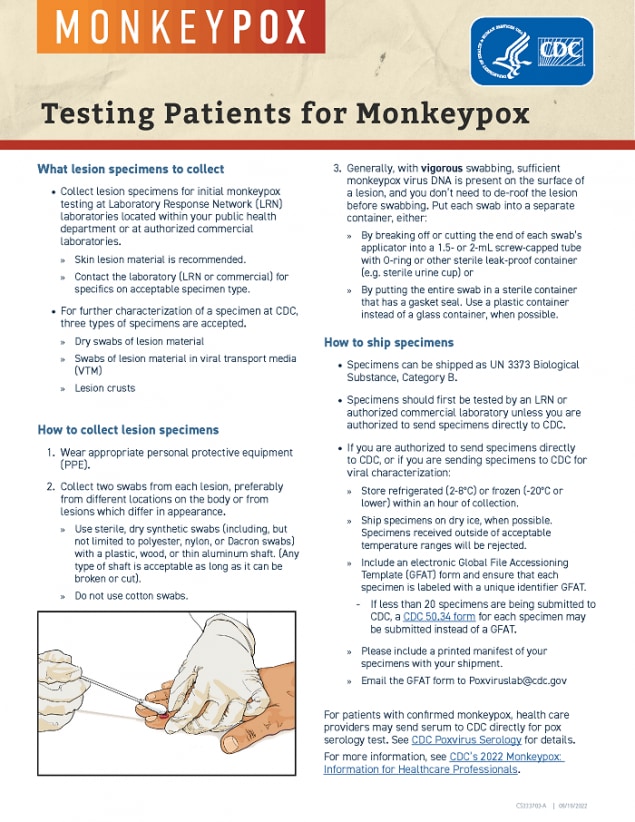
Only sterile, synthetic swabs (including but not limited to polyester, nylon, or Dacron) with plastic, wood, or thin aluminum (wire) shafts should be used to collect suspected or confirmed mpox specimens for diagnostic testing. Do not use cotton swabs.
Skin lesion material, including swabs of lesion surface, exudate, or lesion crusts are the recommended specimen types for laboratory testing of mpox virus specimens. Procedures and materials used for collecting specimens may vary depending on the phase of the rash (e.g., swabs from lesion surface or crust from healing lesion). Collect two swabs from each lesion, preferably from different locations on the body or from lesions that differ in appearance (e.g., a pair of swabs for each lesion with a total of 2-3 lesions). Vigorously swab each lesion, avoiding contamination of gloved hands, to ensure adequate viral DNA is collected. Unroofing or aspiration of lesions (or otherwise using sharp instruments for mpox testing) before swabbing is not necessary, nor recommended due to the risk for sharps injury. Place swabs from lesions, crusts, and exudate in separate tubes.
The type of acceptable specimen (dry swab or wet swab in transport media) for diagnostic testing may vary depending on the laboratory. Contact the appropriate laboratory facility to determine the specimen types accepted. At CDC, only dry swabs or swabs in viral transport media (VTM) from lesions, or lesion crusts are currently accepted for testing. Swabs in media designated for bacterial preservation may cause PCR inhibition and are not recommended.
Insert each swab into a sterile container such as a sterile tube or urine container. Glass containers are not recommended. Carefully bend to break the swab’s shaft to fit inside the sterile container (if applicable, or place the entire swab into the container) . After completely securing the lid, wipe the container with an EPA-approved disinfectant for emerging viral pathogens. Placing parafilm around the lid of the container is recommended for additional leak-proof protection, but not required. Remove gloves, wash your hands (hand hygiene), and don a new pair of gloves.
Testing Patients for Mpox
File Details: 1 MB, 1 page
Specimen Label
Clinical Laboratory Improvement Amendments (CLIA) require laboratories to ensure positive specimen identification and optimum integrity of a patient’s specimen using 2 identifiers and the specimen information.
Clearly label the specimen container with the patient identifiers and include the appropriate specimen information prior to collecting the specimen. Identifiers must be visible, and labels cannot cover the identifiers. Patient identifiers should include at least 2 of the following:
- Patient name (full first and last name, no initials)
- Patient date of birth (MM/DD/YYYY)
- Patient sex assigned at birth
- A unique ID generated at the time of collection (e.g., a medical record number). A State Public Health Lab ID does not satisfy the requirement
Specimen information should include but is not limited to:
- Collection site (e.g., left arm, upper left groin, right cheek, etc.)
- Collection date
- Specimen type
Contact the laboratory facility if additional information is required on the label.
When accessioning specimens, confirm the specimen has been collected correctly from the individual being tested.
Storage
After specimen collection, store specimens in sterile leak-proof containers. Use a durable container for the required shipping and temperature conditions. Glass containers are not recommended.
If testing occurs at an external laboratory, contact the appropriate laboratory facility to determine specimen storage requirements. For testing at CDC, if specimen testing does not occur promptly after specimen collection, refrigerate (2-8°C) or freeze (-20°C or lower) the specimens until testing occurs. Dry swabs, swabs in VTM, or lesion crust(s) that are stored at 2-8°C can be tested up to 7 days from collection. Swab specimens in VTM and lesion crust(s) that are stored frozen (-20°C or lower) can be tested up to 30 days from collection whereas dry swabs that are stored frozen (-20°C or lower) can be tested up to 60 days from collection. For additional information regarding specimens shipped to CDC, see Requirements for Shipping Specimens to CDC.
Pneumatic Tube Transportation
CDC recommends that each laboratory perform a risk assessment before using the pneumatic tube system to transport suspected or confirmed mpox specimens. Each facility should conduct a site- and activity-specific risk assessment of the procedures performed, identifying the hazards involved in the process, the competency level of the personnel performing the methods, and the laboratory facility. An institution’s biosafety professional, laboratory management, scientific/clinical, and safety staff should conduct the risk assessment process to determine the appropriate specimen transport practices to implement at the facility.
Facilities should ensure that all personnel transporting specimens via pneumatic tubes are trained in safe handling practices, specimen management, and spill decontamination procedures.
For additional information about performing a risk assessment, refer to the Biological Risk Assessment: General Considerations for Laboratories and the Biosafety in Microbiological and Biomedical Laboratories (BMBL) 6th Edition [4.3 MB, 604 pages], Section II – Biological Risk Assessment, pages 9-20.
Shipment
Laboratory testing has indicated that the current mpox outbreak is associated with Clade II (formerly known as the West African clade) of mpox virus. The U.S. government does not consider Clade II of mpox virus as meeting the definition of Category A infectious substance under the Managing Solid Waste Contaminated with a Category A Infectious Substance (page 94). Ship specimens and material suspected or confirmed to contain Clade II of mpox virus as UN 3373 Biological Substance, Category B.
When preparing specimens for shipment, consider individually bagging specimens so that if a leak does occur, it does not cause the rejection of all specimens.
Ship specimens on dry ice, if available. Do not ship specimens at room temperature. Specimens received outside of acceptable temperature ranges will be rejected. If mpox test confirmation occurs at an external laboratory, contact the appropriate laboratory facility to determine shipping recommendations.
The primary receptacle and secondary packaging should maintain their integrity at the temperature of the refrigerant used, even if the refrigerant’s temperature changes. Packages containing dry ice should be designed to prevent pressure buildup, package rupture, and allow gas release. Personnel trained per U.S Department of Transportation (DOT) hazmat transportation training requirements should pack and ship specimens.
Ensure the outer package is appropriately marked and labeled as follows:
- Sender’s name and address
- Recipient’s name and address
- Biological substance label
- Proper shipping name, Biological substance, Category B
- UN identification number, UN 3373
- Name and telephone number of the person responsible for shipment (available during regular business hours; optional if the information is on the airway bill)
- Shipper’s Declaration is not required for UN 3373 Biological Substances Category B shipped specimens
- If an Air Waybill is used, the “Nature and Quantity of Goods” box should show “UN 3373 Biological Substance, Category B” and the number of packages
- Class 9 label, including UN 1845, and net weight, if packaged with dry ice and identified as Carbon Dioxide, solid, or Dry ice
Requirements for Shipping Specimens to CDC
In most situations, specimens should be sent to the appropriate state public health laboratory (SPHL) or a commercial laboratory for initial testing. If authorized to send directly to CDC for testing, see the requirements listed below. For more information, contact poxviruslab@cdc.gov regarding specimen types accepted, labeling, specimen storage, and shipping timeframes for testing specimens at CDC.
- CDC only accepts lesion material from dry swabs, swabs in VTM, and crust(s) from the lesion(s). Swabs in media labeled universal transport media or M4 transport media cannot be accepted for testing at CDC.
- Refrigerated specimens (2-8°C)
- Dry swabs, swabs in VTM, or lesion crust(s) must be tested within 7 days from collection
- Frozen specimens (-20°C or lower)
- Swabs in VTM or lesion crust(s) must be tested within 30 days from collection
- Dry swabs must be tested within 60 days from collection
- Refrigerated specimens (2-8°C)
- The temperature at arrival determines whether CDC can accept the specimen:
- Swabs in VTM or lesion crust(s) that arrive at -20°C or lower can be tested within 30 days from collection
- Dry swabs that arrive at -20°C or lower can be tested within 60 days from collection
- Specimens (dry swabs, swabs in VTM, or lesion crust(s)) that arrive between -20°C and 8°C can be tested within 7 days from collection
- Shipment using dry ice is highly recommended
- Specimens received outside of acceptable temperature ranges will be rejected
- Two unique specimen identifiers are required:
- Combination of full first and last name (patient initials are not permitted),
- Date of birth
- Sex and age (must be together to count as 1 identifier)
- A unique ID that is generated at the time of collection
NOTE: Specimen ID, laboratory information management system (LIMS) ID, state public health laboratory (SPHL) ID, or case ID are not acceptable identifiers. - Identifiers must be visible, and labels cannot cover the identifiers.
- Swabs cannot have foam or other material placed at the bottom.
- Specimens do not have to be transported in 2 mL O-ring tubes if the original container is sterile and leak-proof. Leaking specimens, and specimens contaminated by contact with a leaked specimen, will not be tested. Consider individually bagging specimens, if possible.
- Commercial laboratories must provide a State ID on the accessioning forms; CDC cannot provide a report to the SPHL without a State ID.
- Include CDC 50.34 forms for each specimen when submitting less than 20 specimens. If your laboratory is submitting bulk specimens (more than 20 specimens), use a global file accessioning template (GFAT). Contact poxviruslab@cdc.gov to receive this form.
For more information on specimen submission to CDC