Preventing Histoplasma Exposures in the Workplace
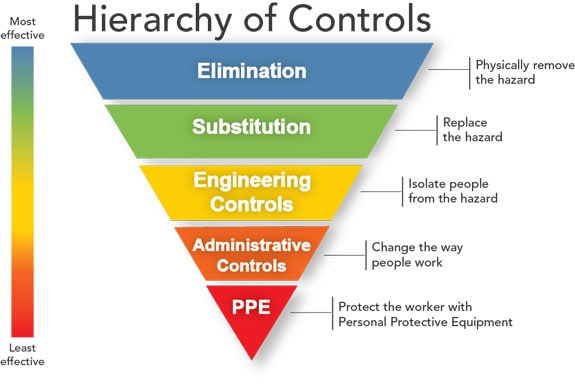
Figure 1: Hierarchy of Controls
Occupational health and safety specialists use the hierarchy of controls [Figure 1] to determine how to implement feasible and effective control solutions to occupational hazards. This framework can be used to prevent exposure to histoplasmosis in the workplace.1,2 Elimination (removing the hazard) and substitution (replacing the hazard) are the most effective ways to reduce occupational hazards but can be difficult to implement for infectious agents such as Histoplasma. In some cases, large amounts of bird or bat droppings should be cleaned up by a professional company that specializes in handling hazardous waste.
Developing a site-specific safety and health plan is an important step in minimizing workplace exposures.3 The plan should have input from management, employee representatives, and health and safety professionals. A comprehensive plan includes the identification of potential hazards and a description of the necessary measures to prevent, control, and reduce those hazards. Measures should include engineering and administrative controls and use of PPE.
Excluding bats or birds from a building
Because work-related histoplasmosis often involves disruption of bird or bat droppings1, the best way to prevent exposure to Histoplasma is to prevent the accumulation of bird or bat droppings in the first place.
To move bats away from an occupied roost in a building:2-3
- Identify and seal entry and exit points. Seal even the smallest holes because some types of bats can squeeze through an opening as small as a dime.
- Install and maintain lights in the roosting area. This will force bats to seek another daytime roosting site.
- Construct bat houses near former roosts. This is a common practice for the welfare of evicted bats and may also keep the bats from colonizing in nearby buildings.
Ultrasonic devices and chemical repellents are not effective for eliminating bats from a roosting area.4
To exclude birds from a building:5
- Identify and seal entry and exit points.
- Consider visual deterrents (balloons, flags, lights, and replicas of hawks and owls) and noises, which may scare birds away but may not have long-lasting effects.
- Use nontoxic, chemical bird repellents like liquids, aerosols, and nondrying films. Disadvantages of these materials are that some are messy, and none are permanent. Even the most effective ones require periodic reapplication.
- Use mechanical anti-roosting systems consisting of angled and porcupine wires made of stainless steel. These systems may require some occasional maintenance to clear nesting material or other debris from the wires.
Controlling dust generation when removing bat or bird droppings
Once a roosting site has been discovered in a building or other location, make plans to restrict the area and determine the extent of contamination. When deciding about removing accumulations, consider factors like the amount and location of the material, the structural integrity or soundness of the building or structure, weather conditions, and whether people are near it. When an accumulation of bat or bird dropping is discovered, removing the material may not always be the next step. Simply leaving the material alone may be the best course of “action” if human activity around the location is unlikely.
If the material must be removed, work practices and dust control measures that eliminate or reduce dust generation will lower risk of infection. For example, carefully spraying dry, dusty material with water instead of shoveling or sweeping it, can reduce the amount of aerosolized material (or material dispersed or spread into the air).6 Adding a surfactant (also called a wetting agent, like a detergent) to the water might reduce further the amount of aerosolized material. Once the material is wetted, it can be collected in a secure container for immediate disposal. An alternative method is to use an industrial vacuum cleaner with a high-efficiency filter to collect potentially contaminated material. Truck-mounted or trailer-mounted vacuum systems are recommended for areas with large accumulations of bat or bird manure. See the personal protective equipment section for workers involved in these activities.
In most cases, environmental sampling to confirm Histoplasma is no longer present after removal of bird or bat droppings is unnecessary. However, before a removal activity is considered finished, the cleaned area should be visually inspected to ensure no residual dust or debris remains.
Disinfecting potentially contaminated material
Disinfectants have occasionally been used to treat contaminated soil and accumulations of bat droppings when removal was not practical or as a precaution before a removal process was started. However, there are no Environmental Protection Agency-approved products registered specifically as soil disinfectants or as being effective against Histoplasma. In past histoplasmosis outbreak settings, formaldehyde was used to decontaminate material contaminated with Histoplasma.7-9 This is not recommended because formaldehyde can cause a variety of health problems.10
Disposing of waste
Any material removed from a work site that might be contaminated with Histoplasma should be disposed of properly and safely and should not be moved to another area where it could still be a health hazard. State and local requirements for the removal, transportation, and disposal of potentially contaminated material should be followed. If state or local landfill regulations define material contaminated with Histoplasma to be infectious waste, incineration or another disposal method may also be required. If disposing in a landfill, arrangements should be made with a landfill operator.
Controlling aerosolized dust during construction, excavation, and demolition
Even in the absence of large accumulations of bat and bird droppings, Histoplasma spores can be aerosolized (or dispersed or spread into the air) during construction, excavation, or demolition. Once airborne, spores can be carried easily by wind currents over long distances, and these spores could infect people outside of the work site. Regardless of whether a work site is in an area where Histoplasma is common, take precautions to prevent dust aerosolization from active and inactive bird or bat roosts.11
Water sprays or other dust suppression techniques should be used to reduce the amount of dust aerosolized during construction, excavation, or demolition in regions where Histoplasma is common.12 During windy periods or other times when typical dust suppression techniques are ineffective, earthmoving activities should be interrupted. All earthmoving equipment (bulldozers, trucks, and front-end loaders) should have enclosed cabs with air-conditioning and HEPA filtration (if available) to protect their operators. Air filters on air-conditioners should be inspected on a regular schedule and cleaned or replaced as needed. During filter cleaning or replacement of exceptionally dusty air filters, maintenance workers should wear respiratory protection if there is a potential for the dust to be aerosolized. Truck beds carrying dirt or debris from a work site should be covered, and all trucks should pass through a wash station before leaving the site. When at a dump site, a truck operator should ensure that people in the vicinity will not be exposed to aerosolized dust while the truck is emptied.
References
- Benedict K, Mody RK [2016]. Epidemiology of histoplasmosis outbreaks, United States, 1938-2013. Emerg Infect Dis 22(3):370–378.
- DePerno, CS [2020]. Animal Damage Control. In: 2020 N.C. Agricultural Chemicals Manual. North Carolina Department of Forestry and Environmental Resources.
- Bat Conservation International, Inc. [1996]. Exclusion experts promote pest control industry changes. Bats 14(2):10–11.
- Tuttle MD [2005]. America’s neighborhood bats. Austin, TX: University of Texas Press.
- Williams DE, Corrigan RM [1994]. Pigeons (rock doves). In: Prevention and control of wildlife damage. [https://agri.nv.gov/uploadedFiles/agrinvgov/Content/Protection/Resource_Protection/Pigeon.pdf]
- Stobierski MG, Hospedales CJ, Hall WN, Robinson-Dunn B, Hoch D, Sheill DA [1996]. Outbreak of histoplasmosis among employees in a paper factory—Michigan, 1993. J Clin Microbiol 34(5):1220–1223.
- Bartlett PC, Vonbehren LA, Tewari RP, Martin RJ, Eagleton L, Isaac MJ, Kulkarni PS [1982]. Bats in the belfry: an outbreak of histoplasmosis. Am J Public Health 72:1369–1372.
- Bartlett PC, Weeks RJ, Ajello L [1982]. Decontamination of Histoplasma capsulatum-infested bird roost in Illinois. Arch Environ Health 37:221–223.
- Tosh FE, Weeks RJ, Pfeiffer FR, Hendricks SL, Greer DL, Chin TDY [1967]. The use of formalin to kill Histoplasma capsulatum at an epidemic site. Am J Epidemiol 85:259–265.
- Agency for Toxic Substances and Disease Registry [1999]. Toxicological profile for formaldehyde. Atlanta, GA: U.S. Department of Health and Human Services, Public Health Service. [https://www.atsdr.cdc.gov/toxprofiles/tp111.pdf]. Date accessed: November 2020.
- Morse DL, Gordon MA, Matte T, Eadie G [1985]. An outbreak of histoplasmosis in a prison. Am J Epidemio 122(2):253–261.
- Huhn GD, Austin C, Carr M, Heyer D, Bourdeau P, Gilbert G, Eimen T, Lindsley MD, Cali S, Conover CS, Dworkin MS [2005]. “Two outbreaks of occupationally acquired histoplasmosis: more than workers at risk.” 113(5): 585-589.
Posting health risk warnings
Areas known or suspected to be contaminated with Histoplasma, like bird or bat roosts, attics, or entire buildings that contain accumulations of bat or bird droppings, should be posted with signs to warn people of the health risk. Each sign should provide the name and telephone number of a person to contact with questions about the area. In some situations, fences or locks may be needed to prevent people from entering.
Hazard communication and training
Before starting an activity that could disturb any material that might be contaminated by Histoplasma, workers should understand the potential risks and how to protect themselves. Employers should inform and train workers on potential work hazards and associated safe practices, procedures, and protective measures. A written hazard communication program about histoplasmosis should include:
- What histoplasmosis is and what causes it
- Signs and symptoms of histoplasmosis
- Treatment for histoplasmosis
- Who can get histoplasmosis
- Risk factors for developing symptomatic histoplasmosis
- Where Histoplasma lives
- Jobs and activities with risks for Histoplasma exposure
- How to prevent Histoplasma exposure
In addition to elimination, engineering and administrative controls, personal protective equipment (PPE) including respirators can be used to protect workers from exposures to Histoplasma.
Respiratory protection
There are no occupational exposure limits for Histoplasma. Respirators are designed to reduce the concentrations of dust and harmful airborne pathogens in the wearer’s breathing air. Respirators are generally divided into two main categories: air-purifying respirators (filter contaminated air) and atmosphere-supplying respirators (provide an alternative supply of breathable air). Workers needing protection against Histoplasma should use particulate-filtering air-purifying respirators (Figure 1). These include:
- Filtering facepiece respirators (e.g., N95)
- Elastomeric respirators (half facepiece or full facepiece)
- Powered air-purifying respirators (PAPRs) (tight fitting and loose fitting)
Respirators must be NIOSH-approved and properly selected and used. If the filters become damaged or the respirator becomes difficult to breathe through or, in the case of a PAPR, the airflow falls below the minimum level, the worker should immediately move to a non-contaminated area and replace the filter. Failure to do so might defeat the protective role of the respirator.
Research is limited on the effectiveness of respirators in protecting workers from breathing in dust and Histoplasma. However, respirators are expected to offer some level of protection since the diameter of Histoplasma spores ranges from 1 µm to 5µm.1-3 NIOSH-approved respirators will collect all types of workplace aerosols, including airborne infectious organisms with very high efficiency.
 [PDF - 182 KB]
[PDF - 182 KB]Figure 1. Types of air purifying respirators
Respirators must be selected based on:
- The level of risk for histoplasmosis while performing the job
- The required assigned protection factor (APF; the level of workplace protection that each class of respirators is expected to provide to employees when the employer implements a continuing, effective respiratory protection program) needed to reduce the level of risk to an acceptable level OSHA assigned protection factors are found in Table 1 of the OSHA Respiratory Protection Standard.
- The advantages and disadvantages of each respirator class
In areas where Histoplasma is common,
Consider use of half-facepiece respirators, including filtering facepiece respirators, during medium risk activities like:
- Working outdoors, particularly involving soil or plant matter disruption (demolition, excavation, farming)
- Working with live poultry or other birds (except where large accumulations of droppings exist, which pose a higher risk)
Consider use of a loose-fitting or tight-fitting PAPR equipped with any of the approved filters (HE, PAPR100-N, and PAPR100-P) or a full facepiece with 100 series filters to be worn before and throughout high-risk activities like:
- Remediating sites with documented Histoplasma or those linked to human illnesses
- Disrupting or cleaning up large accumulations of bird or bat droppings
- Removing trees or other plant material at large bird roosting sites
- Entering caves or tunnels where bats live when there is a possibility of disrupting bat droppings
If PAPRs and full facepiece respirators with 100 series filters are not available, consider using filtering facepiece respirators. It should be noted that filtering facepiece respirators only have an assigned protection factor of 10 so they only provide 20% of the protection afforded by PAPRs (APF 25–50) and full facepiece APRs (APF 50). A filtering facepiece respirator will provide some protection. The respiratory protection program manager will need to determine whether this is enough protection depending upon the wearer’s environment.
Find more information on respirator selection in the NIOSH Respirator Selection Logic document.
OSHA requires employers to develop and implement a written respiratory protection program with required worksite-specific procedures and elements for required respirator use (29 CFR 1910.134). The program establishes that the employee required to wear a respirator must be trained, medically evaluated, and fit tested, among other program requirements. Cleaning, disinfecting, and properly storing a respirator are also important to guarantee they protect the wearer efficiently.
Find more information on the OSHA respiratory protection program, including training videos, on the OSHA Respiratory Protection webpage.
Find additional information about respirators on the NIOSH Respirator webpage.
Other recommended PPE

Figure 2. Other recommended personal protective equipment for exposures to Histoplasma
Gloves should be worn when removing large amounts of droppings or when a person’s hands will touch contaminated soil or other material. Disposable gloves (vinyl, nitrile, PVC, or polyethylene) should be worn under regular cotton or leather work gloves. The use of eye protection (either eyecup or cover-type safety goggles) is recommended, especially when working in ventilated worksites.
Disposable protective clothing and shoe or boot coverings should be worn whenever regular work clothing and shoes might be contaminated with dust containing Histoplasma spores.46 This can reduce or eliminate the likelihood of transferring spores to places away from a work site, like a car or home. When spore-contaminated material is likely to fall from overhead, workers should wear disposable protective clothing (coveralls) with hoods6. Workers should wear disposable shoe coverings with ridged soles made of slip-resistant material to reduce the likelihood of slipping on wet or dusty surfaces. Since protective clothing can be more insulating than regular work clothing, precautions may need to be taken to control heat stress. After completion of work, workers should remove all protective clothing and shoe coverings and seal them in heavy duty plastic bags for disposal.
References
- Deepe GS Jr. [2000]. Chapter 254: Histoplasma capsulatum. In: Mandell GL, Bennett JE, Dolin R, eds. Principles and practices of infectious diseases. 5th ed. Philadelphia, PA: Churchill Livingstone, pp. 2718–2733.
- Cano MVC, Hajjeh RA [2001]. The epidemiology of histoplasmosis: a review. Semin. Respir. Infect. 16(2):109–118.
- Wheat LJ [2000]. Chapter 3: Histoplasmosis. In: Sarosi GA, Davies SF, eds. Fungal Diseases of the Lung. 3rd ed. Philadelphia, PA: Lippincott Williams and Wilkins, pp. 31–46.
- Storch G, Burford JG, George RB, Kaufman L, Ajello L [1980]. Acute histoplasmosis. Description of an outbreak in northern Louisiana. Chest 77:38–42.
- Leslie L, Arnette C, Sikder A, Adams J, Holbrook C, Bond J, King B, Roberts K, Patrick MS, Palmer C, Finger R, Tomford JW, Rushton T [1995]. Histoplasmosis— Kentucky, 1995. MMWR 44(38):701–703.
- Lenhart SW [1994]. Recommendations for protecting workers from Histoplasma capsulatum exposure during bat guano removal from a church’s attic. Appl Occup Environ Hyg 9:230–236.
- USAEHA [1992]. Managing health hazards associated with bird and bat excrement. Aberdeen Proving Ground, MD: U. S. Army Environmental Hygiene Agency, U. S.Army Environmental Hygiene Agency Technical Guide 142.
- Su CP, de Perio MA, Cummings KJ, McCague AB, Luckhaupt SE, Sweeney MH [2019]. Case investigations of infectious diseases occurring in workplaces, United States, 2006-2015. Emerg Infect Dis 2019;25(3):397–405.
- Armstrong PA, Beard JD, Bonilla L, Arboleda N, Lindsley MD, Chae SR, Castillo D, Nuñez R, Chiller T, de Perio MA, Pimentel R, Vallabhaneni S [2018]. Outbreak of severe histoplasmosis among tunnel workers-Dominican Republic, 2015. Clin Infect Dis 2;66(10):1550–1557.
- Raterman SM. Methods of control. In: Plog B ed. Fundamentals of Industrial Hygiene. Itasca: National Safety Council; 2000:585–605.
