Decreased Smoking Disparities Among Vietnamese and Cambodian Communities — Racial and Ethnic Approaches to Community Health (REACH) Project, 2002–2006
Corresponding author: Youlian Liao, MD, Division of Community Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. Telephone: 770-488-5299; E-mail: ycl1@cdc.gov.
Summary
Since 1964, smoking prevalence in the United States has declined because of nationwide intervention efforts. However, smoking interventions have not been implemented uniformly throughout all communities. Some of the highest smoking rates in the United States have been reported among Southeast Asian men, and socioeconomic status has been strongly associated with smoking. To compare the effect in reducing racial and ethnic disparities between men in Southeast Asian (Vietnamese and Cambodian) communities and men residing in the same states, CDC analyzed 2002–2006 data from The Racial and Ethnic Approaches to Community Health (REACH) project. The prevalence of current smoking significantly decreased and the quit ratio (percentage of ever smokers who have quit) significantly increased in REACH Vietnamese and Cambodian communities, but changes were minimal among all men in California or all men in Massachusetts (where these communities were located). The smoking rate also declined significantly, and the quit ratio showed an upward trend in U.S. men overall; however, the changes were significantly greater in REACH communities than in the nation. Stratified analyses showed decreasing trends of smoking and increasing trends of quit ratio in persons of both high and low education levels in Vietnamese REACH communities. The relative disparities in the prevalence of smoking and in the quit ratio decreased or were eliminated between less educated Vietnamese and less educated California men and between Cambodian and Massachusetts men regardless of education level.
Eliminating health disparities related to tobacco use is a major public health challenge facing Asian communities. The decline in smoking prevalence at the population level in the three REACH Vietnamese and Cambodian communities as described in this report might serve as a model for promising interventions in these populations. The results highlight the potential effectiveness of community-level interventions, such as forming community coalitions, use of local media, and enhancing communities' capacity for systems change. The Office of Minority Health and Health Equity selected this intervention analysis and discussion to provide an example of a program that might be effective for reducing tobacco use-related health disparities in the United States.
Introduction and Background
Despite an overall decline in smoking prevalence in the United States since 1964, prevalence remains high in some groups (1), particularly among Asian American men, including Vietnamese, Cambodian, Laotian, Korean, and Filipino Americans (2). The National Latino and Asian American Study in 2002–2003 found smoking prevalences of 23.6% in Chinese men, 24.4% in Filipino men, and 29.5% in Vietnamese men (3). Smoking is a social and cultural norm for men in Asian countries (4), and review of tobacco industry documents indicated that the tobacco industry has targeted and developed specific strategies to promote tobacco-use among immigrants and Asian American communities (5). Since 1985, a limited number of tobacco-control interventions were targeted to Asian American communities (6–10).
A 2010 study documented overall decreasing trends in the prevalence of smoking among men in Asian communities served by the Racial and Ethnic Approaches to Community Health (REACH) project (11). REACH is a CDC effort to eliminate racial/ethnic disparities in health by supporting community coalitions to design, implement, and evaluate community-driven strategies (12). Because some of the highest smoking rates in the United States have been reported among Southeast Asian men (2,3), 5-year trends in smoking prevalence during 2002–2006 were examined among men in three REACH Southeast Asian communities: two Vietnamese communities in California (one each in Los Angeles/Orange counties and Santa Clara County) and one Cambodian community in Lowell, Massachusetts. Trends were compared with those in the total population of men living in the respective states and in the total U.S. male population. Because smoking is strongly associated with socioeconomic status (2,3,13), rates stratified by education levels were compared.
CDC's Office of Minority Health and Health Equity selected the intervention analysis and discussion that follows to provide an example of a program that might be effective in reducing smoking-related disparities in the United States. Criteria for selecting this program are described in the Background and Rationale for this supplement (14).
Methods
Intervention
In 1999, CDC launched REACH 2010 to help 42 minority communities across the United States eliminate health disparities (12). With the intent to promote widespread change in risk or protective behaviors and reduce health disparities, REACH emphasized changes in policy and community environments, in community resources to remove barriers to healthy behavior, and in social norms. In each of the 42 competitively selected and funded communities, REACH targeted at least one of the following racial/ethnic groups: blacks, Hispanic Americans, Asian Americans/Pacific Islanders, and American Indians/Alaska Natives. Each intervention program focused on one or more of the following health priority areas: cardiovascular disease, diabetes, breast and cervical cancer screening and management, infant mortality, vaccinations, and human immunodeficiency virus/acquired immunodeficiency syndrome. This report examines two Vietnamese communities in California (one in Los Angeles/Orange Counties and one in Santa Clara County) and a Cambodian community in the city of Lowell, Massachusetts.
REACH was a multicomponent community intervention, not a tobacco intervention trial. Although different communities selected different diseases and conditions as their priority areas, the overall goal was to build a healthy community through increased knowledge and motivation to live a healthy lifestyle. The intervention of these three communities followed a logic model developed by CDC (15) that included three stages:
1. Capacity building. Community-based coalitions were formed to address community health issues. Each coalition comprised a community-based organization and at least three other organizations, of which at least one was a local or state health department, university, or research organization. These coalitions were operated primarily by residents of the community at every stage of the program (planning, implementation, and evaluation). For example, the Vietnamese REACH for Health Initiative Coalition in Santa Clara County was a partnership of 16 community groups, county health providers, and researchers at the University of California, San Francisco. The coalition planned and implemented a Community Action Plan that included multimedia campaigns, outreach activities by lay health workers, patient navigation assistance, and continuing medical education for Vietnamese health-care professionals.
2. Targeted actions. Interventions included culturally tailored and language-appropriate health communications campaigns, education, and health promotion programs. The communities created local radio and cable TV talk shows in Vietnamese and Khmer languages (e.g., the Public Service Announcement program "Quitting Smoking for Your Kids" in Lowell). The coalitions also distributed educational audiotapes and CDs to low-literacy residents and distributed posters, newsletters, and fact sheets in stores, restaurants, churches and temples, community meetings, health fairs, worksites, health clinics, and senior centers. Educational classes, seminars, health-focused field trips, and workshops also were offered to community members. Education topics varied by community, with different chronic disease emphases. However, because smoking is a common risk factor for many chronic diseases, many interventions addressed it in that light. For example, active and passive exposure to cigarette smoke is a risk factor for cervical cancer (16). Although Vietnamese American women have a low prevalence of active smoking, passive smoke exposure is a problem for them because of the high prevalence of smoking by Vietnamese men (2,3).
3. Community and systems change. REACH focused on reducing the barriers to health promotion information and access to health care for poor and underserved persons and ensured nondiscriminatory and culturally competent health education. For example, in Lowell, the coalitions worked with Buddhist monks, families, and community leaders to promote smoke-free environments. Communities also provided continuing education on cardiovascular disease and breast and cervical cancer prevention for health-care providers. Hospitals and health clinics provided free health promotion and health education sessions. A key intervention strategy was to create change agents among community leaders, such as community health advocates, advisors, health promoters, ministers, and Buddhist monks, by changing their knowledge, attitudes, beliefs, and behaviors with the intent of diffusing similar changes to the broader community. The coalitions reached out to community leaders, invited them to participate in the coalition activities, and provided them with health information and knowledge. REACH helped community leaders act as catalysts for change in the community. These communities used lay health workers/advisors to reach the most disadvantaged population subgroups. Lay health workers, trained by the programs, assisted residents through health education and health promotion efforts, and they responded to their needs, including linking community members to health-related services, including smoking-cessation programs.
Evaluation
As part of the REACH 2010 evaluation, CDC conducted annual risk factor surveys of adults in each of the five project years during 2002–2006 (17). The surveys were conducted by telephone (except for 2002 in Lowell, where interviews were conducted in person). In the telephone surveys, a dual frame sample design (i.e., a combination of random-digit–dial frame and listed telephone frame) was used, except in Santa Clara County, where only a listed telephone frame was used. The listed telephone frames included the telephone numbers listed under Vietnamese or Cambodian surnames in area telephone directories. For 2002 in Lowell, an area probability sample was drawn. All eligible women aged 40–64 years and up to two other adults in the household were invited to participate in the surveys. The mean response rate for household screening was 65% for the contacted households and 57% for family members interviewed among the eligible members.
The same questionnaire was used in all communities and in all survey years. Interviews were conducted in English, Vietnamese, or Khmer in accordance with the respondent's choice. Respondents were first asked, "Have you smoked at least 100 cigarettes in your entire life?" Those who answered "yes" to the first question were then asked: "Do you now smoke cigarettes every day, some days, or not at all?"
Data from the REACH 2010 Risk Factor Survey were compared with data from the Behavioral Risk Factor Surveillance System (BRFSS), a state-based annual health survey conducted in the 50 states and the District of Columbia (18). The survey uses multistage, random-digit dialing to gather a representative sample from each state's noninstitutionalized residents aged ≥18 years. During 2002–2006, the response rates ranged from 37% to 45% in California, 36% to 45% in Massachusetts, and median rates of 51% to 58% in the United States.
Data Analysis
A total of 14,540 adult residents (43% men) were interviewed in the REACH 5-year surveys. Excluding men with missing information about smoking (0.4%), the average sample sizes in each year were 904 Vietnamese men (range: 748–1,055) and 334 Cambodian men (range: 135–418). The average numbers of men participating each year in BRFSS during 2002–2006 were 2,000 and 3,500 in California and Massachusetts, respectively.
Persons who had smoked at least 100 cigarettes in their entire lifetime were defined as ever smokers. Those who smoked cigarettes every day or some days at the time of the interview were defined as current smokers. Those who had smoked at least 100 cigarettes but did not smoke at the time of the interview were defined as former smokers. Quit ratio, an indicator of proportion of smokers quitting (19), was calculated as the percentage of former smokers among ever smokers.
The prevalence of current smoking and the quit ratio were calculated for each survey year and were age-standardized by the direct method to the 2000 U.S. census. In REACH communities, the measures were also standardized by the language used during the interview, using percentage distributions of the combined 5 years of data as the standard. The prevalences of current smoking and quit ratio were also stratified by two education levels (less than high school/high school graduate or higher) and by two income levels (<$25,000/≥$25,000 per year). Chi-square test was used to compare baseline (2002) characteristics between REACH communities and comparison states. P<0.05 was considered as statistically significant.
Logistic regression was performed by using person-level data to examine the trend in the prevalence of current smoking and quit ratio during 2002–2006. Age (categorized into 5 groups) and the language used in the interview were included in the model as covariates. The β coefficient of the year term was determined for each target and each comparison population. The 2-sided z test was then used to determine whether the β coefficients for the trend in the target and comparison populations significantly differed from one another. P<0.05 was considered as statistically significant.
To better compare the relative changes over time among different populations with different absolute baseline levels of smoking measures, the average annual percentage change was used in this report, instead of the absolute percentage point change, which was used previously (11). Natural log transformation of the age-standardized current smoking prevalence and quit ratios at each survey year was performed and then linear regressions on the year term (values of 1 through 5) was performed. The average annual percentage change in the dependent variable was calculated as 100*(eβ- 1), where β is the regression coefficient of the year term derived from the linear regression (20).
Relative disparity was used as an indicator to measure disparity between REACH communities and comparison states. A value >1.0 indicated disparity in tobacco use (e.g., higher smoking prevalence or lower quit ratio) in the REACH community, compared with the corresponding states and vice versa. A value of 1.0 indicated no disparity. Relative disparity in current smoking was the ratio of the standardized prevalence of current smoking in REACH communities versus comparison states, whereas relative disparity in quit ratio was the reverse (i.e., the ratio of the standardized quit ratio in comparison states versus REACH communities). Relative disparity was calculated for two education and two income levels separately.
All analyses were performed by using SUDAAN to account for the complex sampling designs in both REACH and BRFSS. In Lowell, where the survey mode changed (i.e., face to face in year 1 and telephone in subsequent years), additional analyses were repeated using years 2-5 only.
Results
Adult men in Vietnamese and Cambodian communities participating in the REACH Risk Factor Survey were compared with men in California and Massachusetts and all U.S. men in 2002 from BRFSS data (Table 1). In the Vietnamese and Cambodian communities, approximately one third of the interviews were administered in English. Vietnamese men in REACH were generally older than California men overall (p<0.001), whereas Cambodian men were younger than Massachusetts men overall and the total U.S. population of men (p<0.001). Cambodian men had the lowest education level. Men in REACH communities had substantially lower annual family income than men in the comparison states and the total population of U.S. men (p<0.001).
In 2002, approximately one third (30.3%) of Vietnamese and nearly half (49.3%) of Cambodian men were current smokers, whereas approximately one fifth of California (19.4%) or Massachusetts (20.3%) men and one fourth (25.4%) of the overall U.S. male population smoked (Table 2). Logistic regression analysis indicated that the prevalence of current smoking significantly decreased in both Vietnamese and Cambodian communities during 2002–2006 but not in California or Massachusetts, the states where these communities were located. As a result of these different trends, the smoking prevalence among Vietnamese men, which exceeded that of California men by 10.9 percentage points in 2002, exceeded the California prevalence by only 5.9 percentage points in 2006; the excess smoking prevalence among Cambodian men versus Massachusetts men decreased from 29.0 percentage points in 2002 to 7.9 percentage points in 2006.
Although smoking prevalence declined significantly in U.S. men overall, the decline in the REACH communities was greater: the magnitude of the negative values of the β coefficient for the year term in the logistic regression equations was significantly larger for Vietnamese and Cambodians than for U.S. men overall (p<0.05 by z tests). The annual decrease in the Vietnamese communities (-6.4%), and the Cambodian community (-13.9%) was larger than in U.S. men overall (-3.8%).
Stratified analyses indicated that the prevalence of current smoking decreased significantly in both education levels among the Vietnamese communities (both p<0.05) (Table 2). Within the Cambodian community, smoking rates significantly decreased in men with higher education (p = 0.001) but not in those with lower education level (p = 0.203). In California and Massachusetts none of the β coefficients in the stratified logistic regressions were significant.
Quit ratios in 2002 were lower in REACH communities than in the comparison states and in the nation (Table 3). Although there was a downturn in 2006, quit ratios increased significantly during 2002–2006 in Vietnamese (p<0.001, 9.6% annually) and Cambodian (p = 0.002, 19.0% annually) communities. In contrast, the quit ratio changed little (-0.7% to 0.1% annually) in the comparison states. Although a significant upward trend also was found in U.S. men overall, the change (1.4% annually) was much smaller than those in REACH communities (p<0.01 by z test).
Stratified analyses showing significant increases in the quit ratio were observed in both education levels in REACH communities but not in the comparison states (Table 3). The quit ratio significantly increased in U.S. men for both low and high education levels (2.1% and 1.4% annually, respectively). However, the changes were significantly smaller than those among REACH communities (p<0.01).
To control for changes in survey interview methods after year 1, only data from years 2–5 in the Cambodian community in Lowell were analyzed. The downward trend of prevalence of current smoking and the upward trend of quit ratio remained stable.
A downward trend in the disparity of current smoking was apparent in both Vietnamese and Cambodian communities and for both education levels (Figure). At year 5 (2006), the relative disparity was <1.0 in Vietnamese men with lower education (0.55) and Cambodian men with higher education (0.78). Downward disparity trends were similar for quit ratio (Figure). In 2006, the disparity was eliminated among men with lower education in Vietnamese communities (relative disparity = 1.0) and reverse among men with higher education in the Cambodian community (relative disparity = 0.90). However, at year 5, disparity in the prevalence of current smoking and quit ratio still existed between Vietnamese men and comparison men in California with higher education level (Figure).
The trends in relative disparity stratified by income level were, in general, similar to those stratified by education level. Downward trends of the disparities in prevalence of smoking and quit ratios were observed for both income levels and for both REACH communities during the 5-year period, except the disparity in prevalence of smoking for Vietnamese men with higher income compared with the corresponding state. In 2006, the relative disparity in current smoking was <1.0 among men with lower income level in Vietnamese communities (0.91) and in the Cambodian community (0.72 and 0.94 for low and high income level, respectively). Relative disparity in quit ratio was also <1.0 among men with lower income level in Cambodian community (0.94). Trends in absolute disparities by education level were similar to those of relative disparities in both prevalence of current smoking and quit ratio.
Discussion
This study describes community interventions to encourage a healthy lifestyle among Asian Americans. These communities included tobacco use and secondhand exposure as a targeted behavior within a comprehensive local health program. The apparent effectiveness of the interventions at reducing disparities in three communities in two states illustrates the likelihood of the interventions' transferability. Approximately one third of Vietnamese and nearly half of Cambodian men smoked at baseline in 2002. However, the prevalence of current smoking significantly decreased, and the quit ratio (percentage of ever smokers who have quit) significantly increased in Vietnamese and Cambodian communities in the REACH 2010 project from 2002 to 2006; during this period, minimal changes were observed in the comparison states where the communities were located. In general, the decreasing trends of smoking and increasing trends of quit ratio were observed in both high and low education levels in REACH communities. Although there was also a trend of decreasing prevalence of smoking and increasing quit ratio in men nationwide, the trends observed in REACH communities were much larger. The relative disparities in smoking were decreased or eliminated between less educated Vietnamese and California men and between Cambodian and Massachusetts men, regardless of education levels.
Over several decades, the United States has experienced a large reduction in the prevalence of major cardiovascular and cancer risk factors. However, this progress has not occurred uniformly in all segments of society (21). Although progress has been achieved in reducing cigarette smoking in the nation, less progress has been made in reducing disparities in cigarette use among persons of low socioeconomic status (13). REACH communities focused on improving the health of the most disadvantaged segments of society (e.g., those who were new immigrants and those with language barriers).
This study documents overall decreasing disparities in smoking in Southeast Asian REACH communities for men of two education and income levels. However, the findings underscore segments in the Vietnamese communities where disparities in smoking remain wide, especially among men with higher education or income levels. A recent study had suggested higher education was associated with no intention to quit smoking among Vietnamese male current smokers in California (22). Differential associations between income and current smoking have been reported across multiple Asian American communities, with evidence suggesting a positive association between income and current smoking among Vietnamese in contrast to a negative association between income and smoking among Filipinos and no significant association among Chinese Americans (23). To effectively eliminate disparities in smoking in Vietnamese communities, tobacco-control efforts might need to target efforts for smokers of higher socioeconomic status using a different set of cultural and social factors relevant to smoking and quitting.
REACH interventions have several unique features in support of the generalizability and scalability of the project. REACH was not a small-scale clinical trial under controlled conditions. It was an intervention implemented under real-world conditions reaching a large proportion of minority populations. Orange, Los Angeles, and Santa Clara counties in California have the three largest populations of Vietnamese Americans in the United States, and Lowell, Massachusetts, has the second highest population of Cambodian Americans in the United States. REACH did not use a standardized intervention protocol across all sites as in a typical research setting but was sufficiently flexible to enable community choices based on available resources and local realities. Culturally sensitive interventions were tailored for minorities and diverse segments of communities. Not all REACH communities focused on the same behavior or disease, but increasing the knowledge and motivation to live a healthy lifestyle was a common objective of the communities. For example, although the Vietnamese communities focused on breast and cervical cancer screening, they also addressed cigarette smoking. REACH was a grassroots community participatory program. It engaged members of the communities to be active participants in their own health and was able to create a sense of ownership for the project by drawing on community groups to create and implement the Community Action Plan. This report on the REACH project offers promising strategies that might help future health interventions in other Asian communities succeed.
Limitations
The findings in this report are subject to at least four limitations. First, the community interventions were evaluated through an annual telephone survey of representative samples of the community. Households without telephone service or with wireless-only telephones were excluded, which might have resulted in under-coverage bias. Adults with wireless-only service are more likely to be current smokers (24). However, such bias also existed in the comparison data from BRFSS. Second, the response rates of the surveys were somewhat lower than optimal, which might result in nonresponse bias. In the nation, there was a consistently downward trend of response rate in the telephone survey over the past decades (18). In REACH, multiple eligible adults in the household were recruited. Hence, a lower response rate was expected. Third, unlike a typical clinical trial, control communities with the same racial groups were not available. Therefore, the net effect of intervention on the significant decline in smoking prevalence observed in the REACH communities was not able to be estimated. Finally, the estimates were based on self-reported data and subject to recall errors/bias or social desirability effects.
Conclusion
Eliminating health disparities related to tobacco use is a major public health challenge facing Asian American communities. The smoking prevalence decrease at the population level in the REACH Vietnamese and Cambodian communities as described in this report is a model for successful interventions in these populations. Analysis of behavioral and health status outcome data from REACH communities has consistently demonstrated improvements across a broad range of outcomes, from reductions in amputations among persons with diabetes to increasing physical activity (25–31). The findings presented here add to the evidence from these previous REACH reports that community-based programs can improve multiple health outcomes and decrease health disparities if they build community partnerships, recognize cultural influences, and develop tailored interventions.
Acknowldgments
The authors acknowledge the following organizations that participated in the REACH Risk Factor Survey: Division of Adult and Community Health, National Center for Chronic Disease Prevention and Health Promotion, CDC, Atlanta, GA; Lowell Community Health Center, Lowell, MA; Orange County Asian and Pacific Islander Community Alliance, Garden Grove, CA; Vietnamese Community Health Promotion Project (Suc Khoe La Vang!) at the University of California, San Francisco; and Vietnamese Reach for Health Coalition, Santa Clara County, CA.
References
- CDC. Prevalence of cigarette use among 14 racial/ethnic populations—United States, 1999–2001. MMWR 2004;53:49–52.
- Kim SS, Ziedonis D, Chen KW. Tobacco use and dependence in Asian Americans: a review of the literature. Nicotine Tob Res 2007;9:169–84.
- Chae DH, Gavin AR, Takeuchi DT. Smoking prevalence among Asian Americans: findings from the National Latino and Asian American Study (NLAAS). Public Health Rep 2006;121:755–63.
- Corrao MA GG, Sharma N, Shokoohi DF, ed. Tobacco control country profiles. Atlanta, GA: American Cancer Society; 2000.
- Acevedo-Garcia D, Barbeau E, Bishop JA, Pan J, Emmons KM. Undoing an epidemiological paradox: the tobacco industry's targeting of US Immigrants. Am J Public Health 2004;94:2188–93.
- Lawrence D, Graber JE, Mills SL, Meissner HI, Warnecke R. Smoking cessation interventions in U.S. racial/ethnic minority populations: an assessment of the literature. Prev Med 2003;36:204–16.
- Fang CY, Ma GX, Miller SM, Tan Y, Su X, Shive S. A brief smoking cessation intervention for Chinese and Korean American smokers. Prev Med 2006;43:321–4.
- Wu D, Ma GX, Zhou K, Zhou D, Liu A, Poon AN. The effect of a culturally tailored smoking cessation for Chinese American smokers. Nicotine Tob Res 2009;11:1448–57.
- McDonnell DD, Kazinets G, Lee HJ, Moskowitz JM. An internet-based smoking cessation program for Korean Americans: results from a randomized controlled trial. Nicotine Tob Res 2011;13:336–43.
- Zhu SH, Cummins SE, Wong S, Gamst AC, Tedeschi GJ, Reyes-Nocon J. The effects of a multilingual telephone quitline for Asian smokers: a randomized controlled trial. J Natl Cancer Inst 2012;104:299–310.
- Liao Y, Tsoh JY, Chen R, et al. Decreases in smoking prevalence in Asian communities served by the Racial and Ethnic Approaches to Community Health (REACH) project. Am J Public Health 2010;100:853–60.
- Giles WH, Tucker P, Brown L, et al. Racial and ethnic approaches to community health (REACH 2010): an overview. Ethn Dis 2004;14(3 Suppl 1):S5-8.
- CDC. Cigarette smoking—United States, 1965–2008. In: CDC health disparities and inequalities report—United States, 2011. MMWR 2011;60(Suppl, January 14, 2011).
- CDC. Background and rationale. In: Strategies for reducing health disparities—selected CDC-sponsored interventions, United States, 2014. MMWR 2014;63(Suppl 1).
- Tucker P, Liao Y, Giles WH, Liburd L. The REACH 2010 logic model: an illustration of expected performance. Prev Chronic Dis 2006;3:A21.
- Appleby P, Beral V, Berrington de Gonzalez A, et al. Carcinoma of the cervix and tobacco smoking: collaborative reanalysis of individual data on 13,541 women with carcinoma of the cervix and 23,017 women without carcinoma of the cervix from 23 epidemiological studies. Int J Cancer 2006;118:1481–95.
- CDC. REACH 2010 surveillance for health status in minority communities—United States, 2001–2002. MMWR 2004;53(No. SS-6).
- CDC. Public health surveillance for behavioral risk factors in a changing environment: recommendations from the Behavioral Risk Factor Surveillance Team. MMWR 2003;52(No. RR-9).
- US Department of Health and Human Services, Office of the Surgeon General. Reducing the health consequences of smoking: 25 years of progress. A report of the Surgeon General. Atlanta: US Department of Health and Human Srevices, CDC; 1989.
- Vittinghoff E, Glidden D, Shiboski S, McCulloch C. Regression methods in biostatistics: linear, logistic, survival, and repeated measures models. New York: Springer Science; 2005.
- Kanjilal S, Gregg EW, Cheng YJ, et al. Socioeconomic status and trends in disparities in 4 major risk factors for cardiovascular disease among US adults, 1971—2002. Arch Intern Med 2006;166:2348–55.
- Tsoh JY, Tong EK, Gildengorin G, et al. Individual and family factors associated with intention to quit among male Vietnamese American smokers: implications for intervention development. Addict Behav 2011;36:294–301.
- Li S, Delva J. Social capital and smoking among Asian American men: an exploratory study. Am J Public Health 2012;102:S212–21.
- Blumberg SJ, Luke JV, Cynamon ML. Telephone coverage and health survey estimates: evaluating the need for concern about wireless substitution. Am J Public Health 2006;96:926–31.
- Jenkins C, McNary S, Carlson BA, et al. Reducing disparities for African Americans with diabetes: progress made by the REACH 2010 Charleston and Georgetown Diabetes Coalition. Public Health Rep 2004;119:322–30.
- CDC. REACHing across the divide: finding solutions to health disparities. Atlanta, GA: US Department of Health and Human Services, CDC; 2007.
- Plescia M, Herrick H, Chavis L. Improving health behaviors in an African American community: the Charlotte Racial and Ethnic Approaches to Community Health project. Am J Public Health 2008;98:1678–84.
- Nguyen TT, Le G, Nguyen T, et al. Breast cancer screening among Vietnamese Americans: a randomized controlled trial of lay health worker outreach. Am J Prev Med 2009;37:306–13.
- Larson CO, Schlundt DG, Patel K, Wang H, Beard K, Hargreaves MK. Trends in smoking among African-Americans: a description of Nashville's REACH 2010 initiative. J Community Health 2009;34:311–20.
- Liao Y, Tucker P, Siegel P, Liburd L, Giles WH. Decreasing disparity in cholesterol screening in minority communities—findings from the racial and ethnic approaches to community health 2010. J Epidemiol Community Health 2010;64:292–9.
- Miles I, Kruger J, Liao Y, Carlson S, Fulton J. Walking increases among African American adults following a community-based physical activity intervention: racial and ethnic approaches to community health, 2002–2005. Journal of Health Disparities Research Practice 2011;5:43–54.
FIGURE. Five-year trends of relative disparity in the age- and language-standardized prevalence of current smoking (Panel A) and quit ratio (Panel B) stratified by education level among adult men — Vietnamese and Cambodian communities, REACH 2010, and in California, Massachusetts, and United States, 2002–2006
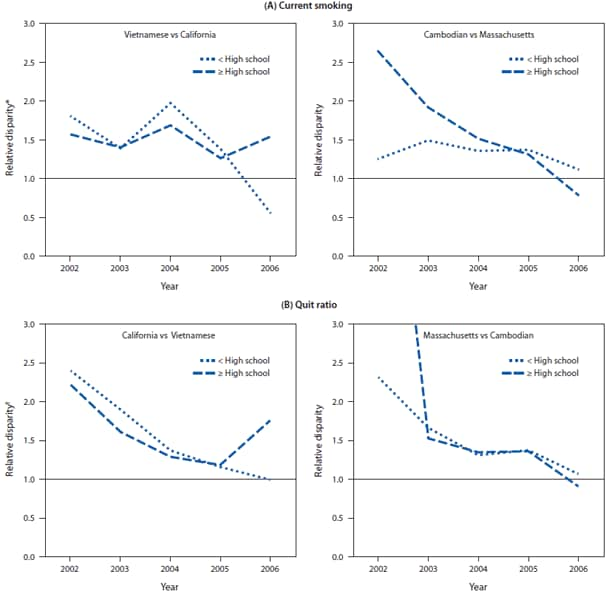
* Relative disparity in current smoking was the ratio of the standardized prevalence of current smoking among Vietnamese or Cambodian men in REACH communities versus all men in comparison states.
† Relative disparity in quit ratio was the ratio of standardized quit ratio among all men in comparison states versus Vietnamese or Cambodian men in REACH communities. Quit ratio was calculated as the percentage of former smokers among ever smokers.
Alternate Text: The figure presents four line graphs that present five-year trends in smoking, from 2002 to 2006. The first two panels compare the disparity in age- and language-standardized prevalence of current smoking between Vietnamese men and other men in California and between Cambodian men and other men in Massachusetts. The final two panels present the quit ratio stratified by education level between Vietnamese men and other men in California and Cambodian men and other men in Massachusetts.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


