Million Hearts: Prevalence of Leading Cardiovascular Disease Risk Factors — United States, 2005–2012
, DPT1, , MPH1, , MS1, , MD1, , MBBS2 (Author affiliations at end of text)
Each year, approximately 1.5 million U.S. adults have a heart attack or stroke, resulting in approximately 30 deaths every hour and, for nonfatal events, often leading to long-term disability (1). Overall, an estimated 14 million survivors of heart attacks and strokes are living in the United States (1). In 2011, the U.S. Department of Health and Human Services, in collaboration with nonprofit and private organizations, launched Million Hearts (http://www.millionhearts.hhs.gov), an initiative focused on implementing clinical and community-level evidence-based strategies to reduce cardiovascular disease (CVD) risk factors and prevent a total of 1 million heart attacks and strokes during the 5-year period 2012–2016 (2,3). From 2005–2006 to the period with the most current data, analysis of the Million Hearts four "ABCS" clinical measures (for aspirin, blood pressure, cholesterol, and smoking) showed 1) no statistically significant change in the prevalence of aspirin use for secondary prevention (53.8% in 2009–2010), 2) an increase to 51.9% in the prevalence of blood pressure control (in 2011–2012), 3) an increase to 42.8% in the prevalence of cholesterol management (in 2011–2012), and 4) no statistically significant change in the prevalence of smoking assessment and treatment (22.2% in 2009–2010). In addition, analysis of two community-level indicators found 1) a decrease in current tobacco product smoking (including cigarette, cigar, or pipe use) prevalence to 25.1% in 2011–2012 and 2) minimal change in mean daily sodium intake (3,594 mg/day in 2009–2010). Although trends in some measures are encouraging, further reductions of CVD risk factors will be needed to meet Million Hearts goals by 2017.
Data Sources
Data from the National Health and Nutrition Examination Survey (NHANES*) for 2005–2012 were used to calculate prevalence estimates for managed low-density lipoprotein cholesterol (LDL-C†) among hyperlipidemic adults aged ≥20 years and estimates for controlled blood pressure§ among hypertensive adults aged ≥18 years. The 2005–2010 NHANES data were the most recent available to estimate the mean daily sodium intake (mg/day¶) among adults aged ≥18 years. Data from the 2005–2010 National Ambulatory Medical Care Survey (NAMCS**) were combined into 2-year cycles to estimate the prevalence of office visits to primary care physicians and cardiologists where aspirin or other antiplatelet medication was prescribed to adults aged ≥18 years with ischemic vascular disease.†† Additionally, NAMCS data were used to estimate the prevalence of office visits where smoking treatment was prescribed among adults aged ≥18 years who were identified as current tobacco users.§§ Data from the 2005–2012 National Survey on Drug Use and Health (NSDUH¶¶) were combined into 2-year cycles to estimate the prevalence of current tobacco product smoking*** among adults aged ≥18 years. This newly adopted measure of current tobacco smoking has been included because it measures all combustible tobacco product use, which is a major CVD risk factor (1) and not just cigarette use, as was the case with previous measures.
Up to four survey cycles (2005–2006, 2007–2008, 2009–2010, and 2011–2012) were examined using sex-, age-, and race/ethnicity-adjusted linear trends analyses (p<0.05). Sex-, age-, and race/ethnicity-adjusted t-tests were used to examine 1) prevalence changes comparing the two most recent data cycles (p<0.05) and 2) differences between sex, age, and race-ethnicity groups within the most recent data cycle (p<0.05).
ABCS Clinical Measures
In 2009–2010, prevalence of recommended aspirin use was greater among men (58.5%) than women (48.0%) and greater among non-Hispanic whites (55.7%) compared with Hispanics (43.6%) (Table 1). The prevalence of blood pressure control improved from 43.4% in 2005–2006 to 51.9% in 2011–2012 (Figure 1); in 2011–2012, the prevalence was greater among women (54.6%) than men (48.9%) and greater among adults aged 45–64 years (56.3%) compared with those aged 18–44 (42.2%) and ≥75 years (41.7%).
The prevalence of cholesterol management increased from 33.0% in 2009–2010 to 42.8% in 2011–2012 (Figure 1); in 2011–2012, the prevalence was greater among adults aged 65–74 years (59.6%) and lower among those aged 20–44 (11.6%) compared with those aged 45–64 years (44.1%) (Table 1). Additionally, the prevalence was higher among non-Hispanic whites (47.4%) compared with non-Hispanic blacks (35.5%) and Hispanics (23.0%). In 2009–2010, the prevalence of smoking assessment and treatment (e.g., cessation medication or counseling) was greater among adults aged 45–64 years (25.3%) compared with those aged 18–44 (20.0%) and ≥65 years (18.9%).
Community-Level Risk Factor Measures
Current tobacco product (cigarettes, cigars, or a pipe) smoking prevalence decreased from 28.2% in 2005–2006 to 25.1% in 2011–2012 (Figure 2). This 11% decline corresponded with a decrease of 11% in current cigarette smoking prevalence from 20.9% in 2005–2006 to 18.5% in 2011–2012, measured using National Health Interview Survey data.††† In 2011–2012, current tobacco product smoking was greater among men (30.3%) than women (20.4%), adults aged 18–44 years (30.5%) compared with those aged 45–64 (24.6%) or ≥65 years (11.4%), and non-Hispanic whites (27.1%) compared with non-Hispanic blacks (26.2%) and Hispanics (18.1%) (Table 2).
The mean daily sodium intake decreased slightly from 3,619 mg/day in 2005–2006 to 3,594 mg/day in 2009–2010 (Figure 2). The most current data show mean daily sodium intake was greater among men (4,225 mg) than among women (2,976 mg), greater among adults aged 18–44 years (3,770 mg) compared with those aged 45–64 (3,640 mg) and ≥65 years (2,992 mg), and greater among non-Hispanic whites (3,631 mg) compared with non-Hispanic blacks (3,352 mg) and Hispanics (3,431 mg) (Table 2).
Discussion
To reach the goal of preventing 1 million heart attacks and strokes during 2012–2016, Million Hearts set population-level goals of achieving ≥65% prevalence for each ABCS clinical measure as well as a 20% reduction in sodium intake (to approximately 2,900 mg/day) and a 10% reduction in current tobacco product smoking prevalence (to approximately 23.6%) (2). A goal to decrease mean daily trans-fatty acid intake is still being promoted (e.g., by supporting ongoing efforts to remove artificial trans-fats from the food supply); however, regular measurement has been deemphasized because of the considerable recent decreases in trans-fat consumption (4) and the cost of regularly obtaining population estimates of consumption. Million Hearts has focused on improving performance in specific clinical and community-level CVD risk factors because interventions in these areas have been shown to be effective ways to greatly decrease CVD morbidity and mortality (2).
Current estimates from 2005–2012 for certain Million Hearts measures serve as baseline values for achieving the initiative's 2017 goals. Additional progress needs to be made in all reported measures important to cardiovascular health, especially among those groups with the smallest prevalence of desired characteristics. For example, the most recently available data show that, compared with those aged ≥45 years, younger adults were more likely to have uncontrolled blood pressure and poorly managed cholesterol, and to smoke tobacco products; younger adults were less likely to receive smoking assessment and treatment, and had greater mean daily sodium intakes. These differences place younger adults at considerable risk for developing CVD and suffering a CVD-related event during their lifetime; persons with two or more major CVD risk factors by age 50 years have more than 10 times the risk for developing atherosclerotic CVD compared with those who are free from major CVD risk factors at that age (5).
The findings in this report are subject to at least seven limitations. First, new cholesterol management guidelines recently released by the American College of Cardiology (ACC) and American Heart Association (AHA) focus on providing treatment with appropriate types and doses of cholesterol-lowering medications (statins) rather than routine treatment to cholesterol targets (6). The cholesterol management rates reported here are based on the previous guidelines in place when the data were collected and the initiative was launched. Second, debate continues over what population-level thresholds should be used to demonstrate adequate blood pressure control, particularly among older adults (7). This report uses the thresholds recommended for the general population by the Seventh Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, because the recommendations remain endorsed by organizations including the ACC, AHA, and the National Institutes of Health and aligns with Healthy People 2020 measures. Third, response rates for the three different surveys ranged from 58.3% to 77.4%, and the results might be subject to nonresponse bias. Fourth, each survey used excludes certain population segments. For example, NHANES surveys include only the noninstitutionalized U.S. population and do not include military personnel. Fifth, one of the smoking cessation medications, bupropion, has multiple indications; however, all bupropion prescriptions were considered as cessation treatment, representing approximately 10% of all documented cessation interventions. Sixth, NAMCS-based visit estimates rely on health-care providers' intervention documentation, for which the quality might vary over time, thereby affecting trend analyses. Finally, the aspirin measure describes the health-care provider's recommended use of aspirin or other antiplatelet medication at a visit and not actual medication use; the indication for use is also not collected. Measures of patient-reported aspirin use are being explored.
Million Hearts strategies (2,3,8) that address these CVD risk factors include promoting use of standardized hypertension treatment protocols (9), effective use of health information technology (2), and self-measured blood pressure monitoring with clinical support.§§§ Other strategies that Million Hearts supports include the following: use of CVD-related clinical quality measures and their incorporation into quality reporting initiatives (10); supporting the Tips From Former Smokers campaign¶¶¶; comprehensive smoke-free policy adoption; implementation of The Community Preventive Services Task Force recommendations, including use of team-based care and reduction of out-of-pocket prescription medication costs****; and population dietary sodium reduction efforts.†††† Additional focus on both clinical-level efforts that support consistent and coordinated patient care and community-level efforts that promote environments that encourage healthy behaviors and reduce unhealthy exposures is needed to continue progress towards meeting Million Hearts goals by 2017.
Acknowledgments
Beth Han, MD, PhD, Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration.
1Division for Heart Disease and Stroke Prevention; 2Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, CDC (Corresponding author: Matthew Ritchey, mritchey@cdc.gov, 770-488-7232)
References
- Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation 2014;129:e28–292.
- Frieden TR, Berwick DM. The "Million Hearts" initiative—preventing heart attacks and strokes. N Engl J Med 2011;365:e27.
- CDC. CDC Grand Rounds: the Million Hearts initiative. MMWR 2012;61:1017–21.
- Vesper HW, Kuiper HC, Mirel LB, Johnson CL, Pirkle JL. Levels of plasma trans-fatty acids in non-Hispanic white adults in the United States in 2000 and 2009. JAMA 2012;307:562–3.
- Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic impact goal through 2020 and beyond. Circulation 2010;121:586–613.
- Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2013. Available at http://circ.ahajournals.org/content/early/2013/11/11/01.cir.0000437738.63853.7a.citation.
- Wright JT Jr, Fine LJ, Lackland DT, Ogedegbe O, Dennison Himmelfarb CR. Evidence supporting a systolic blood pressure goal of less than 150 mm Hg in patients aged 60 years or older: the minority view. Ann Intern Med 2014;160:499–503.
- CDC. Million Hearts: strategies to reduce the prevalence of leading cardiovascular disease risk factors—United States, 2011. MMWR 2011;60:1248–51.
- Frieden TR, King SM, Wright JS. Protocol-based treatment of hypertension: a critical step on the pathway to progress. JAMA 2014;311:21–2.
- Patel MM, Datu B, Roman D, et al. Progress of health plans toward meeting the Million Hearts clinical target for high blood pressure control—United States, 2010–2012. MMWR 2014;63:127–30.
* NHANES is a complex survey of a multistage probability sample of the civilian, noninstitutionalized U.S. population that combines interviews and physical examinations. During 2005–2012, unweighted response rates ranged from 69.5% to 77.4%. Additional information is available at http://www.cdc.gov/nchs/nhanes.htm.
† Defined as LDL-C fasting values in line with the treatment goals established by the National Cholesterol Education Program (NCEP) Adult Treatment Panel-III (ATP-III) guidelines of <160 mg/dL, <130 mg/dL, and <100 mg/dL for low-, intermediate-, and high-risk groups, respectively. LDL-C was used because it is identified by NCEP as the primary target for lipid-lowering therapy. During 2005–2012, of the 21,858 adults aged ≥18 years interviewed for NHANES, 3,155 were included in the LDL-C analyses.
§ Defined as systolic blood pressure of <140 mm Hg and diastolic blood pressure of <90 mm Hg, based on the average of up to three measurements. Among the participants, approximately 95% had two or three blood pressure measurements during a single physical examination at the mobile examination center. For the 5% with only one blood pressure measurement, that single measurement was used in place of an average. During 2005–2012, of the 21,858 persons aged ≥18 years interviewed for NHANES, 7,591 were included in the blood pressure analyses.
¶ The statistics in this report are estimated from Day 1 dietary recall interviews. The data processing step of "adjusting sodium content for salt added during food preparation" was discontinued in 2009–2010; equivalent unadjusted estimates for the 2005–2006 and 2007–2008 cycles are based on the default sodium values in the United States Department of Agriculture's Food and Nutrient Databases for Dietary Studies (FNDDS) 3.0 and 4.1. Additional information is available at http://www.ars.usda.gov/ba/bhnrc/fsrg. During 2005–2012, of the 21,858 adults aged ≥18 years interviewed for NHANES, 16,643 were included in the sodium analyses.
** NAMCS is based on a nationally-representative sample of visits to non-federally employed office-based physicians who are primarily engaged in direct patient care. During 2005–2010, unweighted response rates ranged from 58.3% to 61.6%. Additional information available at http://www.cdc.gov/nchs/ahcd/about_ahcd.htm.
†† The percentage of physician office visits to primary care physicians and cardiologists by adult patients aged ≥18 years with ischemic vascular disease (i.e., history of myocardial infarction, angina, stroke, or other vascular diseases) where physicians had prescribed aspirin or other antiplatelet medication. Visits were excluded if the patient had a condition or medication that contraindicated use of antiplatelet medications. Also excluded were obstetrics and gynecology visits. During 2005–2010, of the 149,027 visits by persons aged ≥18 years included in the NAMCS population, 5,657 were included in the aspirin analyses.
§§ The percentage of physician office visits by adult patients aged ≥18 years who screened positive for current tobacco use (i.e., currently smoke cigarettes/cigars or use snuff or chewing tobacco) where tobacco cessation counseling or cessation medications were ordered or provided. During 2005–2010, of the 149,027 visits by persons aged ≥18 years included in the NAMCS population, 17,631 were included in the smoking assessment and treatment analyses.
¶¶ NSDUH is an annual nationwide survey among persons aged ≥12 years. During 2005–2012, weighted response rates ranged from 73.0% to 75.6%. Additional information is available at http://oas.samhsa.gov/nsduh.htm.
*** The percentage of adults aged ≥18 years who reported smoking cigarettes on at least 1 day during the preceding 30 days and ≥100 cigarettes in their lifetime, or who reported smoking cigars or a pipe on at least 1 day during the preceding 30 days. During 2005–2012, of the 304,125 persons aged ≥18 years included in the NSDUH population, 303,523 were included in the current tobacco smoking analyses.
††† Current smokers were defined as those adults aged ≥18 years who had smoked at least 100 cigarettes in their lifetime and now smoke every day or some days. Additional information available at http://www.cdc.gov/nchs/nhis/tobacco/tobacco_statistics.htm.
§§§ Additional information available at http://millionhearts.hhs.gov/docs/mh_smbp.pdf.
¶¶¶ Additional information available at http://www.cdc.gov/tobacco/campaign/tips/about/campaign-overview.html.
**** Additional information available at http://www.thecommunityguide.org.
†††† Additional information available at http://www.cdc.gov/vitalsigns/sodium.
What is already known on this topic?
Approximately 1.5 million U.S. adults have a heart attack or stroke each year. These events often lead to long-term disability or death. In 2011, the U.S. Department of Health and Human Services, in collaboration with other key partners, launched Million Hearts, an initiative focused on implementing clinical and community evidence-based strategies to prevent 1 million heart attacks and strokes for the 5-year period 2012–2016.
What is added by this report?
From 2005–2006 to the period with the most current data, prevalence of the Million Hearts "ABCS" of clinical care showed no significant change for aspirin use for secondary prevention (53.8% in 2009–2010), improved to 51.9% for blood pressure control and to 42.8% for cholesterol management (in 2011–2012), and showed no significant change for smoking assessment and treatment (22.2% in 2009–2010). Analysis of two community-level indicators found a decrease in current tobacco product (cigarettes, cigars, or a pipe) smoking prevalence to 25.1% (in 2011–2012) and minimal change in mean daily sodium intake (3,594 mg/day in 2009–2010).
What are the implications for public health practice?
Although trends in some measures are encouraging, additional efforts to reduce cardiovascular risk factors are needed to meet the 2017 Million Hearts goals.
|
TABLE 1. (Continued) Current prevalence of implementation of Million Hearts "ABCS" clinical strategies to prevent cardiovascular disease among adults — United States, 2009–2010, 2011–2012 |
|||
|---|---|---|---|
|
Clinical strategy |
%* |
(95% CI) |
p-value using adjusted t-test† |
|
Smoking assessment and treatment (2009–2010)†† |
|||
|
Total |
22.2 |
(20.2–24.4) |
— |
|
Men |
21.1 |
(18.8–23.6) |
referent |
|
Women |
23.2 |
(20.4–26.2) |
0.157 |
|
Age group (yrs) |
|||
|
18–44 |
20.0 |
(17.1–23.3) |
0.003 |
|
18–24 |
17.3 |
(12.6–23.3) |
0.006 |
|
25–44 |
20.6 |
(17.6–24.0) |
0.011 |
|
45–64 |
25.3 |
(22.5–28.3) |
referent |
|
≥65 |
18.9 |
(15.7–22.5) |
0.002 |
|
65–74 |
20.0 |
(16.2–24.4) |
0.025 |
|
≥75 |
16.5 |
(11.1–24.0) |
0.031 |
|
Race/Ethnicity |
|||
|
White, non–Hispanic |
21.9 |
(19.6–24.4) |
referent |
|
Black, non–Hispanic |
25.9 |
(19.7–33.3) |
0.237 |
|
Hispanic |
22.7 |
(16.7–30.1) |
0.685 |
|
Other |
15.0 |
(8.5–25.2) |
0.190 |
|
Abbreviations: ABCS = aspirin use for secondary prevention, blood pressure control, cholesterol management, smoking assessment and treatment; CI = confidence interval. * Weighted, unadjusted estimates. † t-test for statistically significant differences among demographic subgroups, adjusted for sex, age group, and race/ethnicity, using linear/logistic regression. § Source: National Ambulatory Medical Care Survey (NAMCS). Includes office visits to primary care physicians and cardiologists by patients aged ≥18 years with ischemic vascular disease in which aspirin or other antiplatelet medications are prescribed. Excludes visits by patients with a contraindicated condition or medication and obstetric and gynecologic visits. ¶ Source: National Health and Nutrition Examination Survey (NHANES). Blood pressure (BP) control is defined as an average systolic BP <140 mmHg and an average diastolic BP <90 mmHg. Calculated among adults aged ≥18 years with hypertension. Hypertension defined as an average systolic BP ≥140 mmHg, or an average diastolic BP ≥90 mmHg, or self-reported current use of BP-lowering medication, defined as an answer of "yes" to the following questions: "Because of your high blood pressure/hypertension, have you ever been told to take prescribed medicine?" and "Are you currently taking medication to lower your blood pressure?" Excludes pregnant women. ** Source: NHANES. Cholesterol control is defined as a fasting low-density lipoprotein cholesterol (LDL-C) value among adults aged ≥20 years below the target levels (<100 mg/dL for the high risk group, <130 mg/dL for the intermediate risk group, and <160 mg/dL for the low risk group). Calculated among those with LDL-C dyslipidemia, defined using National Cholesterol Education Program's Adult Treatment Panel III risk categories based on the risk for developing coronary heart disease in the next 10 years. Additional information available at http://www.nhlbi.nih.gov/guidelines/cholesterol/index.htm. Current use of cholesterol-lowering medication is defined as an answer of "yes" to the following questions: "To lower your blood cholesterol have you ever been told by a doctor or other health professional to take prescribed medicine?" and "Are you now following this advice to take prescribed medicine?" Excludes pregnant women. †† Source: NAMCS. Includes physician office visits by persons aged ≥18 years who screened positive for current tobacco use during which tobacco cessation counseling or cessation medications were provided. Additional stratification provided for adults aged 18–24 and 25–44 years because of higher prevalence of tobacco use among these age groups. |
|||
FIGURE 1. Prevalence of Million Hearts "ABCS" clinical strategies to prevent cardiovascular disease among adults — United States, 2005–2006 to 2011–2012
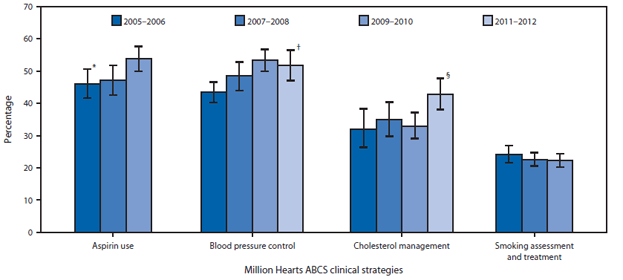
Abbreviation: ABCS = aspirin use for secondary prevention, blood pressure control, cholesterol management, smoking assessment and treatment.
* 95% confidence interval.
† Linear trend adjusted for sex, age group, and race/ethnicity was statistically significant from 2005–2006 through 2011–2012 (p<0.05).
§ Difference between 2009–2010 and 2011–2012 is statistically significant (p<0.05).
Alternate Text: The above figure is a vertical bar chart comparing the prevalence of the four Million Hearts ABCS clinical strategies to prevent cardiovascular disease among adults, for the survey periods 2005-2006, 2007-2008, 2009-2010, and 2011-2012. The four strategies are aspirin use, blood pressure control, cholesterol management, and smoking assessment and treatment.
FIGURE 2. Values for Million Hearts community-level risk factors for cardiovascular disease among adults — United States, 2005–2006 to 2011–2012
* 95% confidence interval.
† Linear trend adjusted for sex, age group, and race/ethnicity was statistically significant from 2005–2006 through 2011–2012 (p<0.05).
§ Linear trend adjusted for sex, age group, and race/ethnicity was statistically significant from 2005–2006 through 2009–2010 (p<0.05).
Alternate Text: The above figure is a vertical bar chart comparing values for two Million Hearts community-level risk factors for cardiovascular disease among adults, for the survey periods 2005-2006, 2007-2008, 2009-2010, and 2011-2012. The two risk factors are current tobacco smoking and mean daily sodium intake.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


