Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Chikungunya Outbreak — Cambodia, February–March 2012
Please note: An erratum has been published for this article. To view the erratum, please click here.
Chikungunya virus (CHIKV) is an alphavirus transmitted to humans through the bite of infected Aedes mosquitoes (1). CHIKV causes fever and usually is not fatal, but can cause debilitating joint pains or, in rare instances, severe illness. The East/Central/South African strain of chikungunya has been emerging in Asia since 2006, first in the Indian subcontinent, then Thailand. This report describes the characteristics of a local outbreak linked with chikungunya reemergence in a rural Asian setting. Sporadic cases of chikungunya were identified in Cambodia in 2011 (2). Antibodies to CHIKV have been detected in serum collected in Cambodia in 2007, but the strain could not be identified for those cases (U.S. Naval Medical Research Unit 2, unpublished data, 2012). On March 7, 2012, several cases of rash with fever were reported among village residents of Trapeang Roka in Kampong Speu Province, Cambodia. Subsequent field investigation revealed that four of six blood samples from affected persons were positive for CHIKV by polymerase chain reaction (PCR) at U.S. Naval Medical Research Unit 2 in Phnom Penh. Investigators from the Cambodian Communicable Disease Control Department, National Malaria Center, Institut Pasteur du Cambodge (IPC), local health centers, and village authorities conducted a seroprevalence study of village residents on March 26 to gather information for response planning and control efforts. The outbreak affected families throughout the village, and 44.7% of the population tested had evidence of infection by CHIKV, which affected all age groups. Public health agencies and policymakers in affected and nearby unaffected areas of Asia and elsewhere should be alert to the potential spread and reemergence of CHIKV.
Trapeang Roka has a population of approximately 695 persons in 134 houses; most adults are farmers or factory workers. For the survey, the village was divided into six sectors created by the roads crossing through it. One team of investigators was assigned to each sector, and a central blood-sampling station was established. Teams worked outward from the center of the village, going from house-to-house. In each house, all occupants present were interviewed. Those who were in the field or factory rather than at home were interviewed when they returned to the village in the evening. Informed consent was obtained in the Khmer language from all adult residents and parents or guardians of children; none refused to participate. A standardized questionnaire was used to gather information on demographics and recent (since the February 14–15 rains) or current self-reported symptoms including joint pains, fever >38°C (axillary or subjective), and rash. A clinical case was defined as one or more of these symptoms in a person from this village with onset after February 14 through March 26, 2012. Blood specimens were obtained for serologic testing; dried blood spots were collected from all persons surveyed and venous samples were collected from febrile patients. Confirmed cases had a positive laboratory test.
At IPC's Virology Unit, immunoglobulin M (IgM) antibody capture enzyme-linked immunosorbent assay (MAC-ELISA) testing was performed to detect anti-CHIKV IgM (3). Serologic testing also was performed by MAC-ELISA for recent infection by dengue (DENV) and Japanese encephalitis B (JEV) viruses (4). Positive serology for DENV and JEV pointed to recent flavivirus infection, which might present similar symptoms. Patients who were febrile at investigation also were tested by real-time reverse transcriptase PCR for CHIKV and also DENV and JEV. The 91 persons with recent or current symptoms who were negative for CHIKV IgM were screened for malaria by PCR.
The survey included 98 (73.1%) households distributed throughout the village. The team interviewed 425 persons (61.1% of village population; male:female ratio = 0.82); mean age was 26.4 years (range: 1 month–87 years; interquartile range: 10–39 years). Among the 425 persons interviewed were 96 (22.6%) farmers, 89 (20.9%) students, 91 (21.4%) factory workers, and 73 (17.2%) persons who stayed at home; the remaining 76 persons were preschool-aged children, construction workers, vendors, or pig farmers.
Of the 425 persons interviewed, 312 (73.4%) reported that they had at least one of the three defining symptoms since the rains of February 14–15, 2012 (Table). Among those 312 persons, 173 (55.4%) took leave from school or work. One death during that period was identified retrospectively in a woman aged 33 years with no known underlying disease. The woman had fever and intense joint pain, developed neurologic signs, and died within 2 hours of hospital admission. No samples were available for testing. Her two children were symptomatic, CHIKV IgM-positive, and seronegative for dengue and JEV.
MAC-ELISA tests identified CHIKV IgM in 188 (44.2%) of the 425 persons. Of the six febrile persons, venous blood samples could be analyzed from four: two had positive PCR results for CHIKV, bringing the total that were laboratory confirmed to 190 (44.7%) CHIKV-positives (Table). One person with fever and joint pains was positive for DENV-4. PCR results found traces of Plasmodium spp. nucleic acid indicative of incubating or recent malaria in one afebrile person. Of the 190 CHIKV-positive persons identified, 10 (5.3%) reported having none of the three defining symptoms.
The onset of the epidemic was protracted. Among 140 persons with self-reported fever who recalled an onset date and who had positive results for CHIKV (IgM or PCR), most reported onset occurring approximately 3–5 weeks after a 2-day period of rain (Figure 1). The epidemic curve suggested that the CHIKV outbreak began 3 weeks after the rains, lasted about 3 weeks, and was on the verge of ending when this serosurvey was conducted on March 26, 2012.
Laboratory results were analyzed by age group (Figure 2). The analysis revealed a 40% IgM seroprevalence among persons aged ≤5 years; for persons aged 6–45 years, IgM seroprevalence was approximately 50%, declining sharply for each age group after that. Circulation of at least two other viruses was identified, including 11 cases of DENV, seven cases of JEV, and 15 cases of undistinguishable flaviviruses (among these, 10, four, and eight cases, respectively, occurred among CHIKV-positive cases).
During a small-scale entomologic assessment conducted during March 29–30, 2012, 123 mosquitoes were collected in Trapeang Roka and 651 mosquitoes were collected from a wider area, including two nearby villages that also reported cases, based on syndromic data. Aedes aegypti comprised 41.4% and 53% of mosquitoes collected in the two areas, respectively, and Culex species comprised 21.1% and 13.8%, respectively; the rest were Anopheles species, and no Aedes albopictus were identified.
Reported by
Sowath Ly, PhD, Sopheak Sorn, MA, Arnaud Tarantola, MD, Epidemiology and Public Health Unit; Lydie Canier, MSc, Molecular Epidemiology and Malariology Unit; Philippe Buchy, PhD, Veasna Duong, PhD, Virology Unit, Institut Pasteur du Cambodge, Phnom Penh, Cambodia. Ilin Chuang, MD, Steven Newell, PhD, U.S. Naval Medical Research Unit 2, Phnom Penh, Cambodia. Sovann Ly, MD, Touch Sok, MD, Vandy Som, MD, Communicable Disease Control Dept; Meng Chuor Char, MD, Chantha Ngan, MD, National Center for Malaria Control, Parasitology and Entomology, Ministry of Health of Cambodia. Leakhann Som, MD, Kampong Speu Provincial Health Dept, Kampong Speu, Cambodia. Maria Concepcion Roces, MD, World Health Organization, Phnom Penh, Cambodia. Corresponding contributor: Arnaud Tarantola, atarantola@pasteur-kh.org, +855 (0) 23 426 009, ext. 206.
Editorial Note
The serosurvey in Trapeang Roka on March 26, 2012, documented a CHIKV outbreak in a medium-size rural Cambodian community of 695 residents. It is the first CHIKV serosurvey in Cambodia since the initial isolation of CHIKV in 1961, and the first known serosurvey conducted during a chikungunya outbreak in Southeast Asia. The experience of at least one symptom since the rains was reported by 73.4% of interviewees. CHIKV prevalence was 44.7%, and the prevalence of asymptomatic CHIKV infection was 5.3%. A temporal association was noted between an unusually large rainfall on February 13–14 and the subsequent outbreak of cases of CHIKV beginning 3 weeks later and lasting for 3 weeks.
Most persons who were CHIKV-positive cases had clinical signs and symptoms consistent with chikungunya. The level of seroprevalence in this outbreak is consistent with levels from CHIKV serosurveys conducted during outbreaks on Reunion Island (35%) (5,6) and Mayotte (38%–45%) (7), but lower than that of Lamu Island, Kenya (75%) (8). Seroprevalence was lower in persons aged ≥45 years. This might be the result of immunity acquired when the CHIKV Asian strain circulated in Cambodia in the 1960s. The only other published CHIKV serologic study from the Mekong region was conducted in the Bangkok area in 1998–1999 (9), before the emergence of the East/Central/South African genotype. In that study, the prevalence in mothers (using cord blood) was 31.6% and 45% in women aged >35 years. This new genotype, which emerged in Africa in 2004 and is emerging in Cambodia, is well known to have an E226V mutation that is more efficiently transmitted by Ae. albopictus.
The findings in this report are subject to at least four limitations. First, cocirculating arboviruses (i.e., dengue and JEV) share the same vector and cause similar symptoms. Some symptoms might have been caused by dengue or JEV infection. Some of the clinical cases, therefore, could have been caused by undetected viruses other than CHIKV, and this could explain why clinical cases outnumbered laboratory-confirmed cases. Second, CHIKV IgM seroprevalence might have been underestimated because of suboptimal sensitivity of tests performed on dried blood spots. Third, IgM screening might miss infection still in the incubation period. Finally, the presence of a large team of medical investigators in a rural village might have stimulated over-reporting of symptoms. These also might account for the difference between the clinical attack rate and CHIKV IgM-positive prevalence (approximately 30%).
CHIKV affects all age groups. While conducting the survey, investigators also provided education to help control the outbreak, which had nearly ended. The main vector identified in the historic Reunion Island outbreak was Ae. albopictus, the Asian tiger mosquito, but none were found in the current study area. The fact that Ae. aegypti were found, but not Ae. albopictus, is important for researchers working on biomolecular aspects of transmission of the new variant chikungunya. Awareness of the location and extent of chikungunya virus infection can help guide health planning efforts and prioritization of resources for control, both in Cambodia and nearby, currently unaffected countries such as Laos or Vietnam.
Acknowledgments
Khon Khiev, Touch Kuy, Sophath Sang, Trapeang Roka, Cambodia. Tai Chak, Chantha Heng, Chantry Houng, Tithary Kong, Van Nuth, Rotha Pen, Ministry of Health of Cambodia; Ny Che, Sovann Chhoy, Bunthol Net; Sothoun Sang, Kong Pisey Health Center; Suosdey Din, Phalmony Has, World Health Organization/Applied Epidemiology Training; Lydie Canier, Siam Chan, Malen Chan, Ann Conan, Vicheth Duong, Sophie Goyet, Sopheap Hem, Saraden In, Vanney Keo, Nimol Khim, Raya Khom, Chanthy Leng, Olivier Marcy, Didier Menard, Kunthy Nguon, Sivuth Ong, Yaty Pho, Manil Saman, Kim Onn Sok, Naysim Te, Saravoin Touch, Bunthin Y, Institut Pasteur du Cambodge (IPC); Kimsan Souv, IPC/National Center for Parasitology, Entomology and Malaria Control; Hout Bora, Kurusarttra Somwang, Heang Vireak, Naval Medical Research Unit 2, Phnom Penh, Cambodia.
References
- Jupp PG, McIntosh BM. Chikungunya virus disease. In: Monath TP, ed. Arbovirus: epidemiology and ecology. Boca Raton, FL: CRC Press; 1988:137–57.
- Duong V, Andries A-C, Ngan C, et al. First detection of Central/East African genotype of chikungunya virus in Cambodia. Emerg Infect Dis. In press.
- Rossi CA, Ksiazek TG. Enzyme-linked immunosorbent assay (ELISA). In: Lee HW, ed. Manual of hemorrhagic fever renal syndrome and hantavirus pulmonary syndrome. Seoul, Korea: WHO Collaborating Center for Virus Reference and Research (hantaviruses); 1998:87–91.
- Buchy P, Vo VL, Bui KT, et al. Secondary dengue virus type 4 infections in Vietnam. Southeast Asian J Trop Med Public Health 2005;36:178–85.
- Renault P, Solet JL, Sissoko D, et al. A major epidemic of chikungunya virus infection on Reunion Island, France, 2005–2006. Am J Trop Med Hyg 2007;77:727–31.
- Gerardin P, Guernier V, Perrau J, et al. Estimating chikungunya prevalence in La Réunion Island outbreak by serosurveys: two methods for two critical times of the epidemic. BMC Infect Dis 2008;8:99.
- Sissoko D, Ezzedine K, Moendandze A, Giry C, Renault P, Malvy D. Field evaluation of clinical features during chikungunya outbreak in Mayotte, 2005–2006. Trop Med Int Health;15:600–7.
- Sergon K, Njuguna C, Kalani R, et al. Seroprevalence of chikungunya virus (CHIKV) infection on Lamu Island, Kenya, October 2004. Am J Trop Med Hyg 2008;78:333–7.
- Watanaveeradej V, Endy TP, Simasathien S, et al. The study transplacental chikungunya virus antibody kinetics, Thailand. Emerg Infect Dis 2006;12:1770–2.
What is already known on this topic?
The East/Central/South African strain of chikungunya has been emerging in Asia since 2006, first in the Indian Subcontinent, then Thailand. Little is known of the transmission dynamics of this chikungunya reemergence in Asia.
What is added by this report?
This report describes the epidemiology of a chikungunya outbreak in a Cambodian village. The outbreak occurred 3 weeks after rains and lasted 3 weeks. The outbreak affected the entire village and all age groups; 44.7% of the population tested had evidence of infection by chikungunya virus (CHIKV). The investigation found an end-of-outbreak clinical attack rate of 73.4%, and a 5.3% proportion of asymptomatic infections.
What are the implications for public health practice?
Awareness of the location and extent of CHIKV infection can help guide health planning efforts and prioritization of resources for control, both in Cambodia and nearby, currently unaffected countries such as Laos or Vietnam.
FIGURE 1. Onset of fever among village residents who recalled an onset date and had laboratory confirmed cases of chikungunya virus (CHIKV) infection* — Trapeang Roka, Cambodia, February and March 2012
* Among these 140 persons with self-reported fever who recalled an onset date and who had positive laboratory results for CHIKV, most reported onset occurring approximately 3–5 weeks after a 2-day period of rain.
Alternate Text: The figure above shows onset of fever among village residents who recalled an onset date and had laboratory confirmed cases of chikungunya (CHIKV) virus infection in Trapeang Roka, Cambodia, during February and March 2012. The onset of the epidemic was protracted. Among 140 persons with self-reported fever who recalled an onset date and who had positive results for CHIKV (immunoglobulin M or polymerase chain reaction), most reported onset occurring approximately 3-5 weeks after a 2-day period of rain.
FIGURE 2. Prevalence of chikungunya immunoglobulin M (IgM) or polymerase chain reaction (PCR) positivity, by age group — Trapeang Roka, Cambodia, March 2012
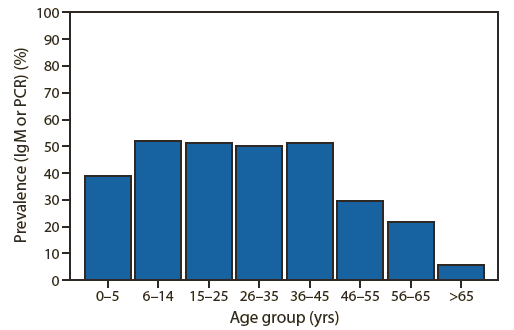
Alternate Text: The figure above shows the prevalence of chikungunya immunoglobulin M (IgM) or polymerase chain reaction (PCR) positivity, by age group in Trapeang Roka, Cambodia, during March 2012. Laboratory results were analyzed by age group. The analysis revealed a 40% IgM seroprevalence among persons aged ≤5 years; for persons aged 6-45 years, IgM seroprevalence was approximately 50%, declining sharply for each age group after that.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


