Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Measles — Horn of Africa, 2010–2011
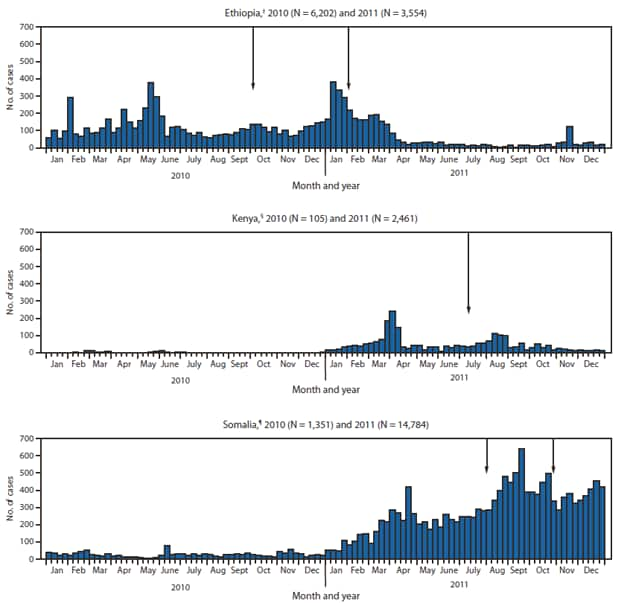
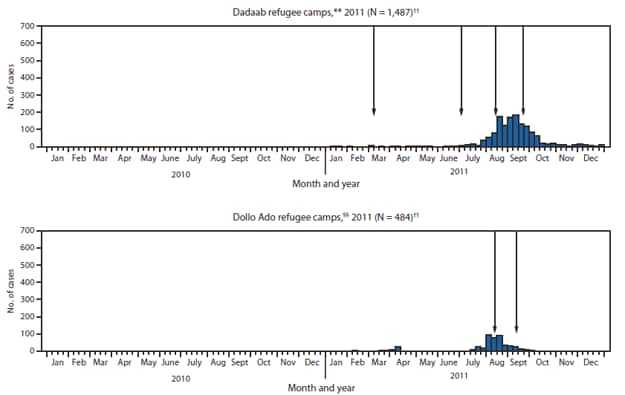
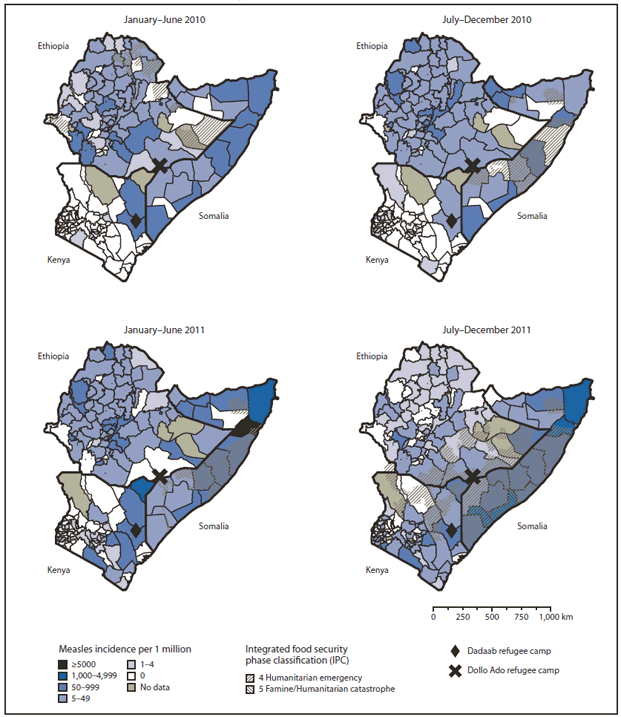
Member states of the World Health Organization (WHO) African (AFR) and Eastern Mediterranean (EMR) regions have set goals for measles elimination by 2020 and 2015, respectively. The two WHO regions include AFR member states Ethiopia and Kenya, and EMR member state Somalia. All three countries are in the Horn of Africa, where measles remains endemic, with periodic outbreaks despite efforts to achieve elimination goals (1). This report describes outbreaks that occurred in the Horn of Africa during 2010–2011. The outbreaks were exacerbated by a complex humanitarian emergency in Somalia, with an influx of an estimated 600,000 refugees into camps in Kenya and Ethiopia near the borders with Somalia. During 2010–2011, a total of 9,756 measles cases were reported in Ethiopia and 2,566 in Kenya, with wide age distributions, and 16,135 were reported in Somalia, with 78% occurring among children aged <5 years. Cases occurred predominantly in unvaccinated persons. Outbreak response immunization (ORI) strategies were implemented; however, outbreaks continued. To reach AFR and EMR measles elimination targets, uniform high coverage with 2 doses of measles-containing vaccine (MCV) must be achieved and maintained in Horn of Africa countries, including in refugee camps.
In 2010, the World Health Assembly endorsed targets to be met by 2015 as milestones toward eventual global measles eradication. These included 1) increasing first dose coverage with MCV (MCV1) to ≥90% nationally and ≥80% in every district, 2) reducing to and maintaining an annual measles incidence of <5 cases per million population, and 3) reducing estimated measles mortality by ≥95% in comparison with 2000 estimates (2). WHO recommends 2 MCV doses for all children and emphasizes on-time delivery of the first dose at age 9 months in countries with ongoing measles virus transmission (3). In Ethiopia, Kenya, and Somalia, MCV1 is provided in the routine childhood vaccination schedule at age 9 months, and a second dose of MCV is provided through periodic supplemental immunization activities (SIAs). In Somalia, MCV also is provided to children aged 9–59 months during child health days or SIAs. In refugee settings, Sphere standards for humanitarian response* recommend providing MCV to ≥95% of new arrivals aged 6 months–15 years and SIAs to prevent outbreaks (4). Infants that receive MCV1 at age <9 months should receive 2 additional doses at least 1 month apart and according to the national immunization schedule (3).
WHO and the United Nations Children's Fund (UNICEF) annually estimate MCV1 coverage administered through routine immunization services among children aged 1 year. Countries annually report the number of districts with ≥80% MCV1 coverage (5). In refugee camps, MCV coverage is monitored by the United Nations High Commissioner for Refugees using administrative records and nutrition surveys (6). Countries report annual measles surveillance data to WHO and UNICEF (7). In Kenya and Ethiopia, measles surveillance is case-based with laboratory confirmation of suspected measles (8). In Somalia, case-based surveillance with laboratory testing is limited to sentinel sites; an integrated disease surveillance system collects aggregated case counts of clinically confirmed measles cases nationally.
Ethiopia
Estimated MCV1 coverage in Ethiopia was 56% in 2010 and 57% in 2011; the percentage of districts reporting ≥80% MCV1 coverage was 45% in 2010 and 43% in 2011. A nationwide measles SIA targeting approximately 9.1 million children aged 9–47 months was conducted in two phases; seven regions were targeted in October 2010 and the four remaining regions in February 2011 (Figure 1). Administrative coverage† was 106%, and coverage based on a population-based survey was 88.2% (95% confidence interval [CI] = 85.1%–90.6%); 87 (91%) districts reported >95% administrative coverage. During 2010–2011, annual reported measles incidence decreased from 75 to 42 per 1 million population; the percentage of reported cases among children aged <5 years decreased from 45% to 31% (Table,
Figure 2).
Kenya
Estimated MCV1 coverage in Kenya was 86% in 2010 and 87% in 2011. The percentage of districts reporting ≥80% MCV1 coverage was 66% in 2010 and 65% in 2011. The most recent nationwide measles SIA in 2009 reached approximately 82% of an estimated 5.5 million children aged 9–59 months. During 2010, 105 measles cases were reported, primarily in the northeast during the first half of the year. Starting in January 2011, measles cases increased throughout the country, first occurring in the Northeast Province and among the Somali community in Nairobi. National reported measles incidence increased from 3 per 1 million population in 2010 to 59 per 1 million population in 2011 (Table). During July–August 2011, ORIs were conducted in five districts in the Northeast Province; however, cases coinciding with outbreaks in Dadaab refugee camps and in southern Somalia continued to occur (Figures 1 and
2).
Somalia
Estimated MCV1 coverage in Somalia was 46% in both 2010 and 2011. The percentage of districts reporting ≥80% MCV1 coverage was 20% in 2010 and 35% in 2011. During three rounds of child health days conducted during May 2010–January 2011, southern and central regions were inaccessible because of armed conflict, and national administrative coverage was 39%–62%. During 2010–2011, reported measles incidence increased from 145 to 1,542 cases per 1 million population (Table,
Figure 2). ORIs were implemented, but cases continued to occur in 2011 (Figure 1).
Refugee Camps
In 1991, the Hagadera, Ifo, and Dagahaley camps were established in the Dadaab refugee complex in northeastern Kenya to house Somali refugees fleeing civil war. During 2005–2011, the estimated refugee population increased from 127,387 to 443,974 in Dadaab. To accommodate approximately 75,000 refugees in unplanned settlements, Ifo-extension and Kambioos camps were added in August 2011. In the Dollo Ado region of southern Ethiopia, Bokolmanyo and Malkadida refugee camps were established in response to refugees arriving from Somalia during 2009–2010. In 2011, the estimated population of the Dollo Ado camps increased from 46,000 to 142,233, and Kobe, Hilaweyn, and Bur-Amino camps were opened to accommodate the influx of refugees.
In the Dadaab refugee camps, sporadic measles cases occurred during January–June 2011 (Figure 1). In July 2011, an outbreak began, coinciding with a large influx of refugees and the measles outbreak in Somalia; 59% of cases were among refugees aged ≥15 years. During 2011, ORIs were conducted during March 28–April 7, targeting children aged 9 months–14 years; during August 1–5, targeting children aged 6 months–5 years; and during September 12–17, targeting adults aged 15–29 years. In addition, in August 2011, measles vaccination was provided to new arrivals aged 6 months–29 years, all hospitalized pediatric patients, and unvaccinated household contacts aged 6 months–14 years. Beginning in October, reported cases decreased as the numbers of newly arriving refugees also decreased. During March–April 2011, a cluster of measles cases occurred in the Dollo Ado refugee camps, followed by an outbreak involving 436 cases during July–October; 44% of cases were among refugees aged ≥15 years (Figure 1). In September 2011, routine measles vaccination was expanded to include new arrivals aged 6 months–29 years. Beginning in September, the number of new arrivals and reported cases decreased.
Reported by
Assegid Kebede, MD, Expanded Program on Immunization, WHO Somalia, Somalia Liaison Office, Nairobi, Kenya; Hinda Ahmed, PhD, Vaccine Preventable Diseases and Immunization, Regional Office for the Eastern Mediterranean, Cairo, Egypt; Balcha G. Masresha, MD, Immunization and Vaccine Development Program, Regional Office for Africa, Brazzaville, Republic of Congo; Robert T. Perry, MD, Dept of Immunization, Vaccines, and Biologicals, Geneva, Switzerland, World Health Organization. Ann Burton, MBBS, MPH, United Nations High Commissioner for Refugees, Dadaab, Kenya. Paul Spiegel, MD, Div of Programme Management and Support, United Nations High Commissioner for Refugees, Geneva, Switzerland. Curtis Blanton, PhD, Farah Husain, DMD, Div of Global Disease Detection and Emergency Response, James L. Goodson, MPH, James P. Alexander, MD, Global Immunization Div, Center for Global Health; Div of Viral Diseases, National Center for Immunization and Respiratory Diseases, CDC. Corresponding contributor: James L. Goodson, jgoodson@cdc.gov, 404-639-8170.
Editorial Note
Severe drought, famine, war, large-scale population movements, and overcrowded refugee camps led to a complex emergency in the Horn of Africa during 2010–2011. In Somalia, low MCV coverage in areas where immunization services could not be provided for nearly 2 years led to a massive measles outbreak, primarily among children aged <5 years. Population movements, including large influxes of refugees from southern and central areas of Somalia into camps in Kenya and Ethiopia near the Somalia borders led to measles virus transmission among refugees and to outbreaks in Ethiopia and Kenya. After ORIs, the number of cases decreased in the refugee camps; the decrease coincided with a decrease in the number of arriving refugees. However, large outbreaks continued in Kenya and Somalia.
In Somalia, a decades-long civil war and the absence of a centralized government crippled efforts to provide basic public health services, including delivering vaccinations to children. Strategies to achieve high vaccination coverage in such settings should use "days of tranquility" to implement vaccination and child health days (9), and should be designed to ensure that every child receives 2 MCV doses, in accordance with WHO recommendations (3). In 2012, the measles outbreak has continued, and additional vaccination activites should be implemented.
In Kenya, 41% of cases nationally occurred among children aged <5 years, indicating that substantial numbers of children were missed by ORIs and SIAs during the past 4 years. In 2011, an ORI was implemented 6 months after the start of the outbreak, targeting a narrow age group in a limited geographic area, but cases continued to occur. A nationwide follow-up measles SIA is planned for 2012, and efforts are needed to ensure a high-quality campaign.
In Ethiopia, although estimated MCV1 coverage nationally was ≤50% before 2009, measles incidence decreased from 2010 to 2011, which might be related to achieving high coverage in the nationwide SIA targeting children aged 9–47 months during 2010–2011. A comprehensive review of surveillance data and SIA implementation conducted in March 2010 led to the development of SIA "best practices," which were implemented during the 2010–2011 SIA, including involving local leaders in microplanning and social mobilization, focusing on hard-to-reach areas, improving training, and house-to-house canvassing during the SIA.
To prevent large measles outbreaks and ultimately reach measles elimination goals in EMR by 2015 and in AFR by 2020, vaccination strategies must be implemented to achieve and maintain uniformly high 2-dose MCV coverage to reach the 93%–95% population immunity threshold that can provide herd immunity in all countries. In refugee settings, Sphere minimum standards for humanitarian response should highlight the need to provide 1) 2 MCV doses to every child, 2) close monitoring of 2-dose MCV coverage, and 3) inclusion of informal settlements and host communities in vaccination plans. Outbreak preparedness should be maintained to ensure high-quality surveillance for measles cases, appropriate case management, and rapid ORI strategies that reach susceptible populations, based on the age distribution of infected persons in a particular outbreak (10).
References
- CDC. Progress in global measles control, 2000–2010. MMWR 2012;61:73–8.
- World Health Organization. Global eradication of measles: report by the Secretariat. Geneva, Switzerland: World Health Organization; 2010. Available at http://apps.who.int/gb/ebwha/pdf_files/wha63/a63_18-en.pdf. Accessed August 12, 2012.
- World Health Organization. Measles vaccines: WHO position paper. Wkly Epidemiol Rec 2009;84:349–60.
- The Sphere Project. Humanitarian charter and minimum standards in humanitarian response. 3rd ed. Geneva, Switzerland: Sphere Project; 2011. Available at http://www.sphereproject.org/handbook. Accessed August 12, 2012.
- World Health Organization. WHO-UNICEF estimates of MCV coverage. Geneva, Switzerland: World Health Organization; 2012. Available at http://apps.who.int/immunization_monitoring/en/globalsummary/timeseries/tswucoveragemcv.htm. Accessed August 1, 2012.
- United Nations High Commissioner for Refugees. Standards and indicators report. Geneva, Switzerland: United Nations High Commissioner for Refugees; 2012. Available at http://www.unhcr.org/pages/4a0183436.html. Accessed August 24, 2012.
- World Health Organization. Measles reported cases. Geneva, Switzerland: World Health Organization; 2011. Available at http://apps.who.int/immunization_monitoring/en/globalsummary/timeseries/tsincidencemea.htm. Accessed August 1, 2012.
- World Health Organization. WHO-recommended standards for surveillance of selected vaccine-preventable diseases. Geneva, Switzerland: World Health Organization; 2003. Available at http://www.who.int/vaccines-documents/docspdf06/843.pdf. Accessed August 24, 2012.
- Mirza I, Kamadjeu R, Assegid K, Mulugeta A. Somalia: supporting the child survival agenda when routine health service is broken. J Infect Dis 2012;205(Suppl 1):S126–33.
- World Health Organization. Response to measles outbreaks in measles mortality reduction settings. Geneva, Switzerland: World Health Organization; 2009. Available at http://whqlibdoc.who.int/hq/2009/who_ivb_09.03_eng.pdf. Accessed August 24, 2012.
What is already known on this topic?
The member states of the World Health Organization's African Region (AFR) and Eastern Mediterranean Region (EMR) have set goals for measles elimination by 2020 and 2015, respectively. After implementation of measles vaccination strategies, estimated coverage with the first dose of measles-containing vaccine (MCV1) in 2010 was 76% in AFR and 85% in EMR. However, reported measles cases in AFR increased from 37,012 to 199,174 during 2008–2010. Reported measles cases in EMR increased from 12,120 to 36,605 during 2008–2009 but declined to 10,072 in 2010. During 2010, reported measles incidence per 1 million population was 238 in AFR and 17 in EMR.
What is added by this report?
Estimated MCV1 coverage for Ethiopia, Kenya, and Somalia in the Horn of Africa was 56%, 86%, and 46% in 2010, and 57%, 87%, and 46% in 2011, respectively. Measles outbreaks occurred in the region and were exacerbated by a complex humanitarian emergency in Somalia. During 2010–2011, annual reported measles incidence in Somalia increased from 145 to 1,542 cases per 1 million, and an influx of refugees from Somalia into border camps in Kenya and Ethiopia resulted in outbreaks in the camps. Outbreak response immunization campaigns were implemented but with limited effect.
What are the implications for public health practice?
To reach AFR and EMR measles elimination targets, uniform high coverage with 2 doses of measles-containing vaccine (MCV) must be achieved and maintained in Horn of Africa countries, including in refugee camps where Sphere standards for humanitarian response should be fully implemented. To reach global measles reduction targets, strengthened vaccination strategies including supplemental immunization activity "best practices," uniform 2-dose MCV coverage, and improved outbreak preparedness and response among displaced populations are necessary to achieve immunity to measles in 93%–95% of the population.
FIGURE 1. Reported measles cases* by epidemiologic week — Horn of Africa, 2010–2011
Alternate Text: The figure above shows reported measles cases by epidemiologic week, in the Horn of Africa during 2010-2011. Estimated measles-containing vaccine, increasing first dose coverage (MCV1) coverage in Ethiopia was 56% in 2010 and 57% in 2011; the percentage of districts reporting ≥80% MCV1 coverage was 45% in 2010 and 43% in 2011. A nationwide measles SIA targeting approximately 9.1 million children aged 9-47 months was conducted in two phases; seven regions were targeted in October 2010 and the four remaining regions in February 2011.
FIGURE 1. (Continued) Reported measles cases* by epidemiologic week — Horn of Africa, 2010–2011
Alternate Text: The figure above shows reported measles cases by epidemiologic week, in the Horn of Africa during 2010-2011. Estimated measles-containing vaccine, increasing first dose coverage (MCV1) coverage in Ethiopia was 56% in 2010 and 57% in 2011; the percentage of districts reporting ≥80% MCV1 coverage was 45% in 2010 and 43% in 2011. A nationwide measles SIA targeting approximately 9.1 million children aged 9-47 months was conducted in two phases; seven regions were targeted in October 2010 and the four remaining regions in February 2011.
|
Characteristic
|
Country
|
Refugee camp
|
|
Ethiopia
|
Kenya
|
Somalia
|
Dadaab
|
Dollo Ado
|
|
2010
|
2011
|
2010
|
2011
|
2010
|
2011
|
2011
|
2011
|
|
Measles cases*
|
6,202
|
3,554
|
105
|
2,461
|
1,351
|
14,784
|
1,487
|
484
|
|
Incidence per 1 million†
|
75
|
42
|
3
|
59
|
145
|
1,542
|
3,853
|
5,398
|
|
No.
|
(%)
|
No.
|
(%)
|
No.
|
(%)
|
No.
|
(%)
|
No.
|
(%)
|
No.
|
(%)
|
No.
|
(%)
|
No.
|
(%)
|
|
Sex
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Male
|
3,308
|
(53)
|
1,872
|
(54)
|
75
|
(73)
|
1,279
|
(52)
|
NA§
|
—
|
NA
|
—
|
728
|
(49)
|
182
|
(45)
|
|
Age group¶
|
|
<5 yrs
|
2,812
|
(45)
|
970
|
(31)
|
20
|
(20)
|
983
|
(41)
|
976
|
(72)
|
11,601
|
(78)
|
349
|
(24)
|
67
|
(16)
|
|
≥5 yrs
|
3,390
|
(55)
|
2,124
|
(69)
|
80
|
(80)
|
1,411
|
(59)
|
375
|
(28)
|
3,183
|
(22)
|
1,130
|
(76)
|
340
|
(84)
|
|
<9 mos
|
343
|
(6)
|
178
|
(6)
|
1
|
(1)
|
217
|
(9)
|
NA
|
—
|
NA
|
—
|
180
|
(12)
|
6
|
(1)
|
|
9 mos–4 yrs
|
2,469
|
(40)
|
792
|
(26)
|
19
|
(19)
|
766
|
(32)
|
NA
|
—
|
NA
|
—
|
169
|
(11)
|
61
|
(15)
|
|
5 yrs–9 yrs
|
1,464
|
(24)
|
702
|
(23)
|
30
|
(30)
|
553
|
(23)
|
NA
|
—
|
NA
|
—
|
153
|
(10)
|
123
|
(30)
|
|
10 yrs–14 yrs
|
843
|
(14)
|
423
|
(14)
|
35
|
(35)
|
277
|
(12)
|
NA
|
—
|
NA
|
—
|
106
|
(7)
|
39
|
(10)
|
|
≥15 yrs
|
1,083
|
(17)
|
999
|
(32)
|
15
|
(15)
|
581
|
(24)
|
NA
|
—
|
NA
|
—
|
871
|
(59)
|
178
|
(44)
|
|
Vaccination status**
|
|
None
|
2,937
|
(64)
|
1,497
|
(63)
|
53
|
(62)
|
1,023
|
(52)
|
NA
|
—
|
NA
|
—
|
1,111
|
(79)
|
NA
|
—
|
|
1 dose
|
1,309
|
(29)
|
670
|
(28)
|
12
|
(14)
|
697
|
(36)
|
NA
|
—
|
NA
|
—
|
293
|
(21)
|
NA
|
—
|
|
≥2 doses
|
321
|
(7)
|
225
|
(9)
|
20
|
(24)
|
234
|
(12)
|
NA
|
—
|
NA
|
—
|
0
|
(0)
|
NA
|
—
|
FIGURE 2. Annualized reported measles incidence,* by administrative area† — Horn of Africa, 2010–2011
Alternate Text: The figure above shows annualized reported measles incidence, by administrative area, in the Horn of Africa during 2010-2011. During 2010-2011, annual reported measles incidence decreased from 75 to 42 per 1 million population; the percent¬age of reported cases among children aged <5 years decreased from 45% to 31%.