FIGURE 1. Chlamydia prevalence among sexually active* persons, by age group --- United States, 1999--2008†
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
CDC Grand Rounds: Chlamydia Prevention: Challenges and Strategies for Reducing Disease Burden and Sequelae
This is another in a series of occasional MMWR reports titled CDC Grand Rounds. These reports are based on grand rounds presentations at CDC on high-profile issues in public health science, practice, and policy. Information about CDC Grand Rounds is available at http://www.cdc.gov/about/grand-rounds.
Chlamydia, a sexually transmitted infection caused by the bacterium Chlamydia trachomatis, is the most commonly reported nationally notifiable disease. A total of 1,244,180 cases were reported in 2009 (1). However, many infections are not detected, and an estimated 2.8 million infections occur each year (2). The burden of infection is greatest among sexually active adolescents and young adults; chlamydia prevalence among sexually active persons aged 14--24 years is nearly three times the prevalence among those aged 25--39 years (National Health and Nutrition Examination Survey 1999--2008 [NHANES], unpublished data, 2011) (Figure 1). Substantial racial/ethnic disparities in chlamydial infection exist, with prevalence among non-Hispanic blacks approximately five times the prevalence among non-Hispanic whites. Among sexually active females aged 14--19 years, chlamydia prevalence is 6.8% overall (4.4% among non-Hispanic whites and 16.2% among non-Hispanic blacks).
The majority of genital chlamydial infections in both males and females are asymptomatic (3). When symptoms do occur, lower urogenital tract infection can manifest as cervicitis in females and urethritis in males and females. Whether symptomatic or asymptomatic, untreated chlamydia can ascend to the upper genital tract. In males, this can cause epididymitis, which is not thought to be an important cause of long-term sequelae. However, in females, upper tract infection can result in pelvic inflammatory disease (PID), a spectrum of clinical disorders involving infection and inflammation of the uterus, fallopian tubes, ovaries, or adjacent peritoneum. Both clinically diagnosed PID and subclinical upper genital tract infection can result in fibrosis, scarring, and loss of tubal function, which can in turn lead to serious long-term reproductive consequences, including tubal factor infertility (inability to conceive because of structural or functional fallopian tube damage), ectopic pregnancy, and chronic pelvic pain.
Available natural history data have limitations but suggest that 10%--15% of untreated chlamydial infections result in diagnosed clinical PID (4,5). Once clinical PID occurs, up to 10%--15% of cases might lead to tubal factor infertility (4). Chlamydia also can lead to tubal infection that is not diagnosed as PID; thus, an even greater proportion of untreated infections likely lead to infertility. Approximately 750,000 PID cases are diagnosed each year in the United States (6). However, PID has multiple infectious etiologies, and the burden of chlamydia-related PID is difficult to determine. Infertility is a major public health problem; in 2002, 7.4% of married females aged 15--44 years were infertile, and nearly one in five females aged 40--44 years reported receiving a medical service for infertility at some point (7). The proportion of all infertility that is tubal factor varies by clinical setting, ranging from 10% to 40% (8,9). Chlamydia is the leading preventable cause of tubal factor infertility (8). Direct medical costs of chlamydia, including diagnosing and treating chlamydia-associated infertility, are estimated at $701 million annually (in 2010 U.S. dollars) (3).
Prevention Challenges and Solutions
Chlamydia prevention programs have been implemented to reduce the burden of reproductive sequelae resulting from chlamydial infection. Because most reproductive complications of chlamydia occur in females and most infections are asymptomatic, the cornerstone of chlamydia prevention is screening young females for infection. Chlamydia is easily diagnosed and treated. Nucleic acid amplification tests are the preferred diagnostic tests because of their superior sensitivity, and they can be performed on easily collected specimens, such as urine or vaginal swabs. Highly efficacious treatment options include single-dose oral azithromycin or a 1-week course of doxycycline. National chlamydia screening recommendations were first released in 1993. Currently, CDC, the U.S. Preventive Services Task Force (USPSTF), and numerous professional medical associations recommend annual chlamydia screening for all sexually active females aged <25 years and for females aged ≥25 years if they are at increased risk for infection (e.g., if they have new or multiple sex partners) (10). USPSTF defines chlamydia screening of sexually active young females as an A-rated recommended preventive service (strongest recommendation), based on randomized controlled trial data demonstrating that screening reduces PID incidence (2).
Evidence is insufficient to recommend routine chlamydia screening for males because of several factors, including feasibility, impact, and cost-effectiveness in preventing sequelae in females (10). However, targeted male screening in high prevalence settings (e.g., correctional facilities) should be considered when resources permit and such screening does not hinder chlamydia screening efforts in females (10). Male partners of females infected with chlamydia have the highest prevalence of infection and should be the top priority for chlamydia testing and treatment efforts among males.
National screening recommendations have been in place for 18 years. Assessing the success of chlamydia prevention programs in reducing chlamydial infections and associated sequelae is critical. Traditionally, sexually transmitted disease (STD) trends have been monitored through case reports, and reported chlamydia case rates have climbed steadily during the past 2 decades (1). However, reported case rates do not necessarily reflect actual trends in incidence of infection. Increased case rates most likely are attributed to increased detection of infection through greater screening and use of more sensitive tests. In fact, prevalence data from several sources indicate that national chlamydia prevalence has not increased during the past decade and might actually be decreasing (11,12). For example, in a study conducted among women and men entering the National Job Training Program, the adjusted odds of a positive chlamydia test decreased by 19% in women and 8% in men during 2003--2007 (12). In addition, although PID has multiple causes, several data sources demonstrate that PID rates have been decreasing (1,6,13). After substantial declines in PID rates during the late 1980s and 1990s (6), a 25% decline in PID rates during 2001--2005 was observed using a sample of national insurance claims data (13). Overall, available ecologic evidence suggests that current chlamydia prevention programs, focused primarily on screening young females, are having some impact on chlamydia prevalence and PID, but not enough.
Screening females aged <25 years is ranked by the National Commission on Prevention Priorities as one of the 10 most beneficial and cost-effective prevention services, but it also is among the most underutilized (14). Screening coverage increased during 2001--2009 but still was less than 60%; in 2009, coverage was 43% among eligible females enrolled in commercial health-care plans and 57% among the Medicaid population (Figure 2) (15). Expanding chlamydia screening will be critical to reducing disease burden and associated reproductive sequelae. In addition, other prevention strategies also should play an important role, including behavioral interventions, rescreening of infected persons, and partner treatment efforts.
Behavioral risk reduction efforts, such as promoting correct and consistent condom use, can have an impact not only on chlamydia, but also on other STDs, including human immunodeficiency virus (HIV) infection, and on unintended pregnancy (10). Because repeat chlamydial infection is common, CDC recommends rescreening persons with chlamydia 3 months after treatment (10). Finally, treating male sex partners of infected females is critical in preventing repeat infections in females, and modeling work has shown that it also is essential in interrupting chlamydia transmission in the population (16). A safe, effective partner treatment tool endorsed by CDC and many medical associations is expedited partner therapy (EPT) (17). EPT involves providing prescriptions or medications to a patient to take to his/her partner, without examining the partner. EPT has been shown to be useful in ensuring partner treatment among males and reducing repeat infections among females (17).
Barriers exist in implementing chlamydia prevention strategies. Young females might lack knowledge about the need for screening and might be reluctant to seek STD services because of fears related to disclosing sexual activity to health-care providers and the societal stigma related to STDs. In addition, young adults (i.e., those aged 20--29 years) remain the largest uninsured group in the United States, with associated underutilization of health care (18). When young females do seek care, many health-care providers fail to take a sexual history and offer chlamydia screening. Clinicians might have limited knowledge about STDs and screening recommendations, might lack information about community STD rates, and might believe their patients are not at high risk (19). High deductibles and copayments for clinic visits, laboratory services, and medications might be another important barrier. For adolescents, maintaining confidentiality is of particular concern. All 50 states and the District of Columbia currently allow minors to seek care for STD diagnosis and treatment without parental consent; however, maintaining confidentiality in the billing and insurance claims process is challenging. Many states mandate commercial health plans to provide written statements to the primary insured, usually parents or guardians, listing services rendered and those reimbursed by the health plan. Thus, "confidential" services could potentially be disclosed.
Several initiatives are under way to expand chlamydia screening efforts. To address the stigma and the lack of information about chlamydia and other STDs, CDC and its partners, MTV Networks, the Kaiser Family Foundation, and the Planned Parenthood Federation of America, are in the third year of a national campaign known as GYT (Get Yourself Tested).* The goals are to increase awareness among adolescents and young adults, normalize conversations about STD prevention, and promote sexual health and STD testing. The campaign includes public service announcements, videos, an STD testing service locator that can be accessed via website or mobile phone, and tips on generating conversations about STD testing. The Patient Protection and Affordable Care Act of 2010 expands insurance access for young adults and eliminates chlamydia screening copayments for young females who sign up for new insurance plans.† The National Chlamydia Coalition is training medical professionals, endorsing screening by professional medical associations, developing tools to facilitate office-based screening, disseminating information through lectures, articles, and webinars, and promoting quality measures to improve the care of adolescents.§ The coalition also is working to address racial/ethnic disparities in chlamydia prevalence, for example, by using mini-grants to develop community-level prevention approaches in areas with a disproportionate burden. The American Academy of Pediatrics and the Society for Adolescent Health and Medicine have developed coding and billing tools to maximize provider reimbursement while minimizing potential disclosure of confidential services through health plan billing statements.¶
One of the primary barriers to improving partner treatment services for chlamydia has been concerns about the legality of EPT in various jurisdictions. National advocacy efforts have been successful in removing many EPT legal and health systems barriers. In 2006, EPT was legally permissible in 12 states; as of November 2010, it was permissible in 27 states and one city. California was one of the first states to legalize EPT. In monitoring chlamydia partner services, California has found the highest levels of partner treatment with EPT, as well as with an alternative partner treatment strategy, "bring your own partner" (BYOP) (Figure 3) (20). With BYOP, at the time clinic staff members contact patients regarding their positive chlamydia test results and the need for timely treatment, staff members encourage patients to bring their partners with them when they come for treatment. For all partner treatment strategies, cost remains a major barrier to implementation. Ensuring coverage of the partner's prescribed treatment is critical. Effective partner treatment is an evidence-based prevention intervention that can reduce the risk for reinfection in females and ongoing transmission of chlamydia in the population.
Summary and Next Steps
A substantial burden of chlamydia exists in the United States. Chlamydia is an important preventable cause of infertility and other adverse reproductive health outcomes. Effective prevention interventions are available to reduce the burden of chlamydia and its sequelae, but they are underutilized. Although prevention programs appear to be having some impact on chlamydia prevalence and PID, improvements can be made in raising awareness about chlamydia, increasing screening coverage, and enhancing partner services, including EPT. In addition, efforts should focus on reaching disproportionately affected racial/ethnic groups. Improving measurement of program implementation and outcomes also is critical. Chlamydia prevention presents many challenges but also opportunities for improvement. To break the cycle of chlamydia transmission in the United States, health-care providers should encourage annual chlamydia screening for all sexually active females aged <25 years, maximize use of effective partner treatment services, and rescreen infected females and males 3 months after treatment.
Reported by
CL Satterwhite, MSPH, MPH, SL Gottlieb, MD, R Romaguera, DMD, Div of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, CDC. G Bolan, MD, Center of Infectious Diseases, California Dept of Public Health. G Burstein, MD, Dept of Pediatrics, Univ at Buffalo; Women and Children's Hospital of Buffalo, Buffalo, New York. C Schuler, PhD, Div of Respiratory Disease Studies, National Institute of Occupational Health; T Popovic, MD, PhD,* Office of the Director, CDC. *Corresponding contributor: Tanja Popovic, Office of the Director, CDC, 404-639-7220, tpopovic@cdc.gov.
References
- CDC. Sexually transmitted disease surveillance, 2009. Atlanta, GA: US Department of Health and Human Services, CDC; 2010. Available at http://www.cdc.gov/std/stats09/default.htm. Accessed March 25, 2011.
- US Preventive Services Task Force. Screening for chlamydial infection: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2007;147:128--34.
- Chesson H, Blandford J, Gift T, et al. The estimated direct medical cost of sexually transmitted diseases among American youth, 2000. Perspect Sexual Reprod Health 2004;36:11--9.
- Haggerty C, Gottlieb S, Taylor B, et al. Risk of sequelae after Chlamydia trachomatis genital infection in women. J Infect Dis 2010;201(Suppl 2):S134--55.
- Oakeshott P, Kerry S, Aghaizu A, et al. Randomised controlled trial of screening for Chlamydia trachomatis to prevent pelvic inflammatory disease: the POPI (prevention of pelvic infection) trial. BMJ 2010;340:c1642.
- Sutton M, Sternberg M, Zaidi A, et al. Trends in pelvic inflammatory disease hospital discharges and ambulatory visits, United States, 1985--2001. Sex Transm Dis 2005;32:778--84.
- Chandra A, Martinez G, Mosher W, et al. Fertility, family planning, and reproductive health of U.S. women: data from the 2002 National Survey of Family Growth. Vital Health Stat 2005;23(25).
- Macaluso M, Wright-Schnapp TJ, Chandra A, et al. A public health focus on infertility prevention, detection, and management. Fertil Steril 2010;93:16.e1--10.
- Feinberg EC, Larsen FW, Catherino WH, Zhang J, Armstrong AY. Comparison of assisted reproductive technology utilization and outcomes between Caucasian and African American patients in an equal-access-to-care setting. Fertil Steril 2006;85:888--94.
- CDC. Sexually transmitted diseases treatment guidelines, 2010. MMWR 2010;59(No. RR-12).
- Datta SD, Sternberg M, Satterwhite C, et al. Trends in Chlamydia trachomatis prevalence in the United States, 1999--2006: results from the National Health and Nutrition Examination Survey (NHANES). Presented at the 48th Annual Interscience Conference on Antimicrobial Agents and Chemotherapy / Infectious Diseases Society of America 46th Annual Meeting, Washington, DC, October 25--28, 2008.
- Satterwhite CL, Tian LH, Braxton J, Weinstock H. Chlamydia prevalence among women and men entering the National Job Training Program: United States, 2003--2007. Sex Transm Dis 2010;37:63--7.
- Bohm MK, Newman L, Satterwhite CL, et al. Pelvic inflammatory disease among privately insured women, United States, 2001--2005. Sex Transm Dis 2010;37:131--6.
- Maciosek M, Coffield A, Edwards N, et al. Priorities among effective clinical preventive services: results of a systematic review and analysis. Am J Prev Med 2006;31:52--61.
- National Committee for Quality Assurance. The state of health care quality. Washington, DC: National Committee for Quality Assurance; 2010. Available at http://www.ncqa.org/portals/0/state%20of%20health%20care/2010/sohc%202010%20-%20full2.pdf. Accessed March 25, 2011.
- Kretzschmar M, Satterwhite CL, Leichliter JS, et al. Analysis of chlamydia screening in the United States using a stochastic simulation model. Presented at the British Association for Sexual Health and HIV / American STD Association Third Joint Conference, Brooklyn, NY, May 7--10, 2008.
- CDC. Expedited partner therapy in the management of sexually transmitted diseases. Atlanta, GA: US Department of Health and Human Services, CDC; 2006. Available at http://www.cdc.gov/std/treatment/eptfinalreport2006.pdf. Accessed March 25, 2011.
- CDC. Access to and utilization of medical care for young adults aged 20--29 years: United States, 2008. NCHS Data Brief 2010;29:1--8.
- Wiesenfeld H, Dennard-Hall K, Cook R, et al. Knowledge about sexually transmitted diseases in women among primary care physicians. Sex Transm Dis 2005;32:649--53.
- Yu Y, Frasure J, Bolan G, et al. Evaluation of partner services for treatment of Chlamydia trachomatis in California family planning clinics. Presented at the 2008 National STD Prevention Conference, Chicago, IL, March 10--13, 2008. Available at http://cdc.confex.com/cdc/std2008/webprogram/Paper14526.html. Accessed March 28, 2011.
* Additional information available at http://www.gytnow.org.
† Additional information available at http://edocket.access.gpo.gov/2010/pdf/2010-17242.pdf.
§ Additional information available at http://ncc.prevent.org.
¶ Additional information available at http://www.adolescenthealth.org/clinical_care_resources/2304.htm.
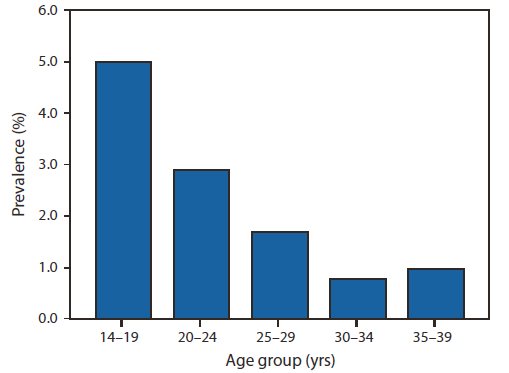
Source: Unpublished data from National Health and Nutrition Examination Survey cycles 1999--2008, combined to provide stable estimates for all subgroups. Additional information available at http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.
* Based on a "yes" response to the question, "Have you ever had sex?" Sex was defined as vaginal, anal, or oral sex.
† All relative standard errors <30%.
Alternate Text: The figure above shows the Chlamydia prevalence among sexually active persons, by age group in the United States from 1999-2008. The burden of infection is greatest among sexually active adolescents and young adults; chlamydia prevalence among sexually active persons aged 14-24 years is nearly three times the prevalence among those aged 25-39 years, according to unpublished 2011 data from the National Health and Nutrition Examination Survey, 1999-2008.
FIGURE 2. Percentage of sexually active* females aged 16--24 years† screened for chlamydia, by health plan type --- United States, 2001--2009
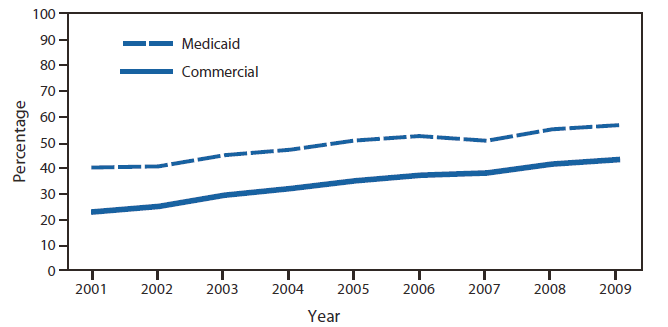
Source: Healthcare Effectiveness Data and Information Set. Available at http://www.ncqa.org/tabid/136/default.aspx.
* Defined as persons who had a claim or visit for pregnancy; contraception; diagnosis, screening, or treatment for a sexually transmitted disease; or cervical cancer screening.
† Aged 16--26 years during 2001--2002, 16--25 years during 2003--2007, and 16--24 years during 2008--2009.
Alternate Text: The figure above shows the percentage of sexually active females aged 16-24 years screened for chlamydia, by health plan type in the United States from 2001-2009. Screening coverage increased during 2001-2009, but was still less than 60%; in 2009, coverage was 43% among eligible females enrolled in commercial health-care plans and 57% among the Medicaid population.
FIGURE 3. Percentage of chlamydia patients reporting that their sex partners also received treatment, by partner management strategy --- eight family planning clinics, California, 2005--2006
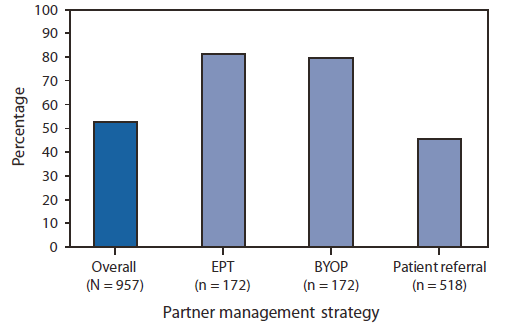
Abbreviations: EPT = expedited partner therapy; BYOP = bring your own partner.
Source: Yu Y, Frasure J, Bolan G, et al. Evaluation of partner services for treatment of Chlamydia trachomatis in California family planning clinics. Presented at the 2008 National STD Prevention Conference, Chicago, IL, March 10--13, 2008. Available at http://cdc.confex.com/cdc/std2008/webprogram/Paper14526.html.
Alternate Text: The figure above shows the percentage of chlamydia patients reporting that their sex partners also received treatment, by partner management strategy from eight family planning clinics in California during 2005-2006. California has found the highest levels of partner treatment for chlamydia with expedited partner therapy (EPT), as well as with an alternative partner treatment strategy, "bring your own partner" (BYOP).
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


