FIGURE 1. Distribution of temporary health-care clinics reporting to the Internally Displaced Person Surveillance System (IDPSS)* and location of IDP camps,† by commune --- Haiti, May 2010
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Rapid Establishment of an Internally Displaced Persons Disease Surveillance System After an Earthquake --- Haiti, 2010
On January 12, 2010, a 7.0-magnitude earthquake in Haiti disrupted infrastructure and displaced approximately 2 million persons, causing increased risk for communicable diseases from overcrowding and poor living conditions. Hundreds of nongovernmental organizations (NGOs) established health-care clinics in camps of internally displaced persons (IDPs). To monitor conditions of outbreak potential identified at NGO camp clinics, on February 18, the Haiti Ministry of Public Health and Population (MSPP), the Pan-American Health Organization (PAHO), and CDC implemented the IDP Surveillance System (IDPSS). The Inter-Agency Standing Committee (IASC) "cluster approach" (1) was used to coordinate the Haiti humanitarian response. One of 11 clusters, the Global Health Cluster (GHC), builds global capacity, whereas the country-level cluster (in this case, the Haitian Health Cluster [HHC], led by PAHO) responds locally. During the Haiti response, HHC engaged NGOs serving large camps, established IDPSS, followed trends of reportable conditions, undertook epidemiologic and laboratory investigations, and fostered implementation of control measures. This report describes the design and implementation of IDPSS in the post-earthquake period. The primary challenges to implementing IDPSS were communication difficulties with an ever-changing group of NGO partners and limitations to the utility of IDPSS data because of lack of reliable camp population denominator estimates. The IDPSS experience reinforces the need to improve local communication and coordination strategies. Improving future humanitarian response requires advance development and distribution of easily adaptable standard surveillance tools, development of an interdisciplinary strategy for an early and reliable population census, and development of communication strategies using locally available Internet and cellular networks.
Pre- and post-earthquake capacity
In 2009, before the earthquake, an estimated 55% of Haitians were living in extreme poverty (2). A total of 45% of the population lacked access to safe water, and 83% lacked access to sufficient sanitation (3). The public health-care system had inadequate infrastructure and no emergency medical system. NGOs provided much of Haiti's health services. A January 2010 World Health Organization (WHO) risk assessment of public health services in Haiti estimated that approximately 250 NGOs were operating within the health sector before the earthquake (3).
Before the earthquake, public health surveillance in Haiti was carried out by two independent systems. The Haitian Health Information System was implemented in 749 health facilities serving the general population. The primary purpose of this system was to monitor health service provision and administrative indicators; data flow was too encumbered to provide timely surveillance. The HIV Monitoring, Evaluation, and Surveillance Interface (MESI) is limited to monitoring the health events of human immunodeficiency virus (HIV)-infected patients.
Haitian government officials estimated that the earthquake resulted in approximately 230,000 immediate deaths and caused 1.5 million persons, approximately 15% of the nation's population, to be displaced to IDP camps. Within days, nearly 900 overcrowded camps were established spontaneously in Port-au-Prince, and an additional 400 further west in Leogane, Jacmel, and Petit-Goâve (Figure 1). Health-care services and humanitarian aid were provided by a huge influx of international and local NGOs. Although approximately 400 health organizations registered officially with the Haitian government, an additional unknown number of organizations also were providing services. Services ranged from general outpatient care to specialized surgical services. Most medical care was provided in temporary tented structures or mobile clinics operating in or around the large camps. The majority of clinics did not possess laboratory capacity, and specimen collection materials were scarce.
The cluster approach was developed by IASC after the 2004 Indian Ocean tsunami to strengthen partnerships among humanitarian organizations and to improve coordination of humanitarian response activities during an emergency (1). The approach has 11 global clusters to be activated locally, as needed, in an emergency: Health, Camp Coordination and Camp Management (CCCM), Water/Sanitation/Hygiene (WASH), Agriculture, Logistics, Early Recovery, Nutrition, Education, Protection, Emergency Shelter, and Emergency Telecommunications. WHO is the lead agency for GHC, which includes 31 United Nations agencies and NGOs. In Haiti, all 11 clusters at the local level were activated.
Establishment of IDPSS
Although some NGOs routinely conduct disease surveillance internally during disaster response operations, no system for sharing and tracking illness data among NGOs existed after the Haiti earthquake. MSPP, CDC, and PAHO created IDPSS in response to the need to establish monitoring of communicable diseases identified in temporary clinics serving IDPs. Disease surveillance was one of the activities of HHC, and required interaction with the local CCCM and WASH clusters. IDPSS is a voluntary passive surveillance system, monitoring 19 priority conditions: six requiring immediate public health notification to MSPP; an additional 10 suspected communicable diseases of outbreak potential; and three programmatic indicators (Table). Total clinic visits per day also were recorded so that surveillance data for each of the 19 priority conditions could be reported as the proportion of all visits in each clinic. Reporting procedures were kept as simple as possible to facilitate voluntary reporting from busy NGO camp clinics, and reportable diagnoses were limited to those posing the greatest public health risk to the displaced population facing overcrowding, poor hygiene and sanitation, malnutrition, exposure to mosquitoes, and incomplete vaccination coverage. MSPP and WHO case definitions (4) were adapted to reflect syndromic diagnoses. This process of adapting reporting forms and data management tools delayed the system's implementation.
To enroll camp clinics in IDPSS, the CDC team contacted 31 of the government-registered NGOs that were serving the largest camps and planning to provide long-term health services. Through telephone calls, periodic clinic visits, and HHC meetings, MSPP, PAHO, and CDC representatives trained NGO providers about IDPSS reporting procedures. NGO clinics were asked to submit their global positioning system (GPS) coordinates to show their location in relation to IDP camps and other clinics (Figure 1).
NGO camp clinics voluntarily submitted reports on a daily basis, whether or not reportable conditions were observed. Although lack of reporting might have occasionally been attributed to a lack of reportable conditions seen on a given day, the primary reason was noncompliance. Individual NGOs were contacted or clinics visited to determine reasons for nonreporting and to offer assistance in facilitating improved compliance. As of epidemiologic week 14 (7 weeks after IDPSS implementation), the reporting requirement shifted from daily to weekly to accommodate clinics, many of which were already submitting weekly because of lack of time and resources.
Because the turnover of personnel at the NGOs was high, and because the NGO camp clinics were located across a wide geographic area, the Haiti IDP Surveillance System Google Group was established to improve communication. This type of publicly accessible Internet forum allows members to exchange messages either with the entire group or a specific member. Electronic files can be posted or downloaded by any member. The IDPSS Google Group was effective in encouraging timely and reciprocal communication between IDPSS coordinators and NGOs and also among NGO colleagues interested in informally comparing observed disease trends and reporting challenges at their respective clinic locations. Each week, feedback reports were available to NGOs on the website and included analysis of trends of proportions of each reportable condition out of total clinic visits (i.e., 100 × [specific condition / total visits per week]).
Surveillance results
IDPSS officially began on February 18, 37 days after the earthquake occurred; however, 33 clinics reported data during February 2--18. By April 24, 91 NGO camp clinics had reported at least one time to IDPSS (mean and median: 35 clinics per week, range: 12--48 clinics per week) (Figure 2). The total number of new clinic visits during February 18--April 24 was 96,472. A total of 23,183 new visits were reported for the 19 reportable conditions, which represents 24% of the total number of clinic visits. Of all clinic visits, the most commonly reported diagnoses were acute respiratory infection (ARI) (n = 8,878 [9%]), suspected malaria (n = 4,899 [5%]), and watery diarrhea (n = 4,549 [5%]) (Table). Although clusters of suspected typhoid fever and malaria were investigated, IDPSS detected no major disease outbreaks through April 24, 2010. Consistent with previous disasters, communicable disease outbreaks were rare (5,6), and ARI was the most commonly reported condition (7).
Lessons learned
Implementation of IDPSS included logistical and operational challenges similar to those described during other humanitarian emergencies: coordinating multiple, geographically dispersed organizations providing clinical services; rapid health-care provider turnover; inadequate infrastructure; and a dynamic situation. The primary challenge was coordinating the multiple and geographically scattered NGO partners.
During the first 7 weeks of IDPSS, infrequent reporting was observed, even from the largest, well-established NGOs. The number of daily reports submitted by any given NGO camp clinic during a 54-day period was highly variable, ranging from one to 50 (median: three reports), making it difficult to follow meaningful trends by geographic location. Improving reporting frequency required consistent technical support, frequent communication with reporters, and a shift to weekly reporting.
Analysis of IDPSS data was limited by the lack of denominator information, making calculation of incidence rates (reportable cases per population) impossible. Instead, trends of proportionate clinic-based morbidity (reportable cases per total clinic visits) were followed. Trends in case counts for each condition also were monitored but were not informative because counts varied according to number of reports submitted and, therefore, primarily reflected clinic reporting behavior rather than disease patterns. In addition, the representativeness of these IDPSS data is unknown. Data on the size and distribution of camps and NGO health-care services being provided were incomplete. Reliable estimates of the population served by each NGO camp clinic did not exist because of incomplete camp census data from responsible cluster partners and lack of information on the catchment area of each clinic. Substantial mobility of IDPs between camps and the fact that nondisplaced Haitians were using services intended for IDPs made population census and catchment area estimates difficult.
Current situation
Six months after the earthquake, frequency of reporting to IDPSS has been increasing. The possibility of disease outbreaks among IDPs remains an active concern for the disaster relief community. Currently, the IDPSS Google Group has 177 members, who represent nearly 60 different NGOs and coordinating agencies. IDPSS continues to function reliably, providing these members weekly reports of baseline trends and news of cluster investigations. IDPSS will become more useful as reporting continues to increase and improved denominator data becomes available from cluster partners responsible for IDP camp census, thus allowing for incidence-based comparisons with national surveillance data.
Recommendations
Emergency preparedness activities should involve partnering with NGOs to develop standard operating procedures, forms, and data management tools that are easily modifiable for surveillance activities in potential humanitarian emergency settings. Advance distribution of these tools and their guidelines would speed implementation and improve system performance.
In settings with similar communication challenges, focus should be both on interactive, Internet-based forums (e.g., the IDPSS Google Group) and in-person meetings. Although telephone and Internet access were disrupted in the days after the earthquake, these networks were reestablished quickly and proved essential for coordination of humanitarian response. All NGOs had Internet access in coordinating offices, whereas access on-site at temporary clinics varied substantially. Cellular telephone access was available throughout earthquake-affected areas, including within camps. These reliable networks should be taken advantage of, and innovative strategies for their use should be formalized for partner communication and surveillance data submission.
The IDPSS experience supports several of IASC recommendations made on the basis of a recent evaluation of the cluster approach in six countries, including Haiti (8). These IASC recommendations address 1) reinforcing the role of international NGOs in clusters; 2) facilitating participation of national and local NGOs to strengthen capacities; and 3) improving mechanisms to deal with multidisciplinary issues and inter-cluster gaps.
Reported by
R Magloire, MD, Ministry of Public Health and Population, Haiti. K Mung, MD, Pan American Health Organization, World Health Organization. ST Cookson, MD, J Tappero, MD, Haiti Transition Office, Center for Global Health; E Barzilay, MD, K Dominguez, MD, C Dubray, MD, K Lindblade, PhD, Emergency Operations Center, Office of Public Health Preparedness and Response; ES Jentes, PhD, M Willis, MD, RA Tohme, MD, AG Sprecher, MD, C El Bcheraoui, PhD, JA Walldorf, MD, EIS officers, CDC.
Acknowledgments
This report is based, in part, on contributions by local and international participating NGOs; EJ Baptiste, N Barthélemy, C Hectivert, PA Joseph, D Lafontant, Haiti Ministry of Public Health and Population; M Wellman, Geospatial Research, Analysis, and Svcs Program, ATSDR; S Blank, T Chiller, K Tomashek, S Wiktor, Emergency Operations Center, Office of Public Health Preparedness and Response; and O Bilukha, Div of Global Disease Detection and Emergency Response, Center for Global Health, CDC.
References
- Inter-Agency Standing Committee. Guidance note on using the cluster approach to strengthen humanitarian response. Geneva, Switzerland: Inter-Agency Standing Committee; 2006. Available at http://www.humanitarianreform.org/humanitarianreform/portals/1/resources%20&%20tools/iascguidancenoteclusterapproach.pdf. Accessed July 29, 2010.
- United Nations Development Programme. Human development report 2009. Overcoming barriers: human mobility and development. Table I-1: human and income poverty. New York, NY: United Nations Development Programme; 2009: 178. Available at http://hdr.undp.org/en/media/HDR_2009_EN_Complete.pdf. Accessed June 29, 2010.
- World Health Organization. Public health risk assessment and interventions. Earthquake: Haiti. Geneva, Switzerland: World Health Organization; 2010. Available at http://www.who.int/diseasecontrol_emergencies/publications/haiti_earthquake_20100118.pdf. Accessed June 29, 2010.
- World Health Organization. Communicable disease control in emergencies: a field manual. Geneva, Switzerland: World Health Organization; 2005. Available at http://www.who.int/infectious-disease-news/iddocs/whocds200527/isbn_9241546166.pdf. Accessed July 29, 2010.
- Watson J, Gayer M, Connolly M. Epidemics after natural disasters. Emerg Infect Dis 2007;13:1--5.
- Guha-Sapir D, van Panhuis W. Health impact of the 2004 Andaman Nicobar earthquake and tsunami in Indonesia. Prehosp Disaster Med 2009;24:493--9.
- Bellos A, Mulholland K, O'Brien K, Qazi S, Gayer M, Checchi F. The burden of acute respiratory infections in crisis-affected populations: a systematic review. Confl Health 2010;4:3.
- Inter-Agency Standing Committee. Cluster approach evaluation phase 2. Synthesis report. Geneva, Switzerland: Inter-Agency Standing Committee; 2010. Available at http://www.humanitarianinfo.org/iasc/pageloader.aspx?page=content-products-common&tempid=99. Accessed June 29, 2010.
What is already known on this topic?
After the January 2010 earthquake in Haiti, a huge influx of nongovernmental organizations (NGOs) began providing needed health-care services in camps of internally displaced persons (IDPs), but no common disease surveillance system among NGOs existed.
What does this report add?
This report describes how the Haitian Ministry of Public Health and Population, CDC, the Pan-American Health Organization, and NGOs established the IDP Surveillance System and devised strategies to overcome coordination and communication difficulties in gathering, analyzing, and disseminating findings with the many NGO partners involved.
What are the implications for public health practice?
Improving future humanitarian response requires advance development and distribution of easily adaptable standard surveillance tools, development of an interdisciplinary strategy for an early and reliable population census to allow analysis of disease incidence, and development of communication strategies using locally available Internet and cellular networks.
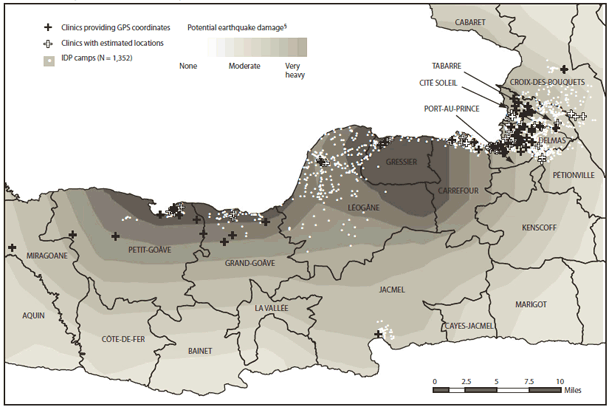
Sources: CDC, Haiti Ministry of Public Health and Population, Pan-American Health Organization, Camp Coordination and Camp Management Cluster (CCCM), United Nations Stabilization Mission in Haiti (MINUSTAH), Geocommons, U.S. Geological Survey.
* Clinics reporting to IDPSS at least once as of May 31, 2010.
† Based on CCCM data, as of May 3, 2010. Available at http://groups.google.com/group/cccmhaiti/web/mapping-and-gis?_done=%2fgroup%2fcccmhaiti%3f.
§ Based on data from the U.S. Geological Survey, available at http://pubs.usgs.gov/tm/2005/12A01.
Alternate Text: The figure above shows the distribution of temporary health-care clinics reporting to the Internally Displaced Person Surveillance System (IDPSS) and location of IDP camps, by commune, in Haiti, during May 2010.
|
TABLE. (Continued) Number of reported cases of 19 priority conditions monitored by the Internally Displaced Persons Surveillance System (IDPSS) --- Haiti, February 2--April 24, 2010* |
|||
|---|---|---|---|
|
Priority condition |
Case definition† |
No. of reported cases (N = 23,183) |
% of total clinic visits (N = 96,472) |
|
Bloody diarrhea |
Acute diarrhea with visible blood in the stool |
497 |
0.5 |
|
Acute febrile illness with jaundice |
Acute onset of jaundice and fever ≥100.4°F (≥38°C) with the absence of any known precipitating factors |
110 |
0.1 |
|
Tetanus |
In an adult with a wound history or a visible infection entry point: jaw contracture with impossibility to eat and to talk, painful muscular contractions, generalized muscle spasms, rigidity In a neonate: any neonate with normal ability to suck and cry during the first 2 days of life who from 3 and 28 days of age cannot suck normally and becomes stiff or has convulsions |
18 |
0.02 |
|
Suspected whooping cough |
Cough for >2 weeks and at least one of the following symptoms: paroxysms (i.e., fits) of coughing, inspiratory whooping, posttussive vomiting (i.e., vomiting immediately after coughing) without other apparent cause |
13 |
0.01 |
|
Suspected cutaneous anthrax |
Skin lesion evolving over 1--6 days: papular through vesicular stage, to depressed black eschar invariably accompanied by edema that might be mild or extensive |
0 |
--- |
|
Programmatic indicators |
|||
|
Tuberculosis (TB) patient with interrupted treatment |
Any patient who has active TB and is currently out of care or experiencing an interruption in TB treatment |
57 |
0.06 |
|
HIV/AIDS§ patient with interrupted antiretroviral therapy (ART) |
Any HIV-infected patient who states that he or she has experienced an interruption in HIV care or ART |
16 |
0.02 |
|
Third trimester pregnancy without previous or pregnancy complications |
Pregnant woman in the third trimester without any previous antenatal care and/or a pregnant woman at any trimester with a complication such as premature rupture of membranes, preeclampsia, eclampsia, bleeding, infection, and complicated abortion |
210 |
0.2 |
|
* Although the official launching of the IDPSS was February 18, 2010, several nongovernment organizations were submitting reports before that date. † Haiti Ministry of Public Health and Population and World Health Organization case definitions were adapted to reflect syndromic diagnoses. § Human immunodeficiency virus/acquired immunodeficiency syndrome. |
|||
FIGURE 2. Number of clinics reporting to the Internally Displaced Persons Surveillance System (IDPSS), by epidemiologic week --- Haiti, February 2--April 24, 2010*
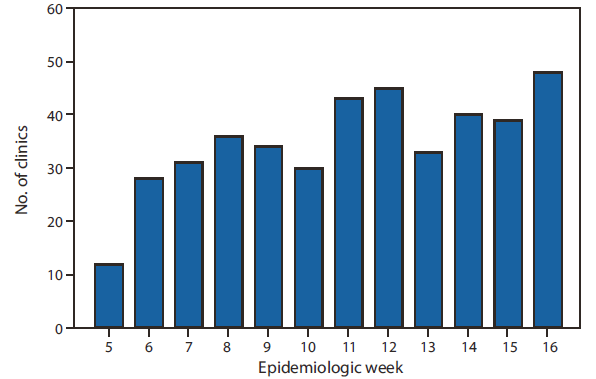
* Although the official launching of the IDPSS was February 18, 2010, several nongovernmental organizations were submitting reports before that date.
Alternate Text: The figure above shows the number of clinics reporting to the Internally Displaced Persons Surveillance System (IDPSS), by epidemiologic week, in Haiti, during February 2-April 24, 2010. IDPSS officially began on February 18, 37 days after the earthquake occurred; however, 33 clinics reported data during February 2-18. By April 24, 91 camp clinics had reported at least one time to IDPSS (mean and median: 35 clinics per week, range: 12-48 clinics per week).
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


