How CDC Enhances Laboratory Quality
CDC laboratories follow our pledge to produce the highest quality scientific data, while ensuring the safety of its staff and the nation.
Supporting CDC Laboratories in Laboratory Quality Efforts
CDC laboratories conduct unique science and provide critical health information that protects the United States against dangerous health threats. High quality laboratory science is essential for CDC to meet its mission.
Scientific data generated or supported by CDC’s laboratories forms the basis of critical public health decision making and policy. CDC has a responsibility to ensure that all CDC laboratory research and development activities, testing processes, and data are the highest quality possible and are traceable, reproducible, documented with appropriate rigor, and meet all applicable regulatory requirements.
In 2019, CDC enacted an agency-wide laboratory quality management policy. This policy formalizes CDC’s commitment to scientific excellence and safety by establishing quality standard requirements for all CDC laboratories. Implementing this policy has further increased CDC’s core capability within its laboratories to prevent, detect, and remedy errors; increase efficiency; and create safer work environments for laboratory scientists and staff.
To ensure first-rate laboratory quality, CDC has developed and is implementing a Laboratory Quality Plan. The Laboratory Quality Plan is the result of collaboration between the Laboratory Quality Office (LQO), the Office of Laboratory Science and Safety (OLSS), and Centers within CDC that have laboratories. The Plan will have these major components when fully implemented:
- Three quality management systems: one for CDC infectious disease laboratories, one for CDC non-infectious disease laboratories and one for CDC NIOSH laboratories. Separate quality systems permit more detailed quality specifications tailor-made for different types of CDC laboratories.
- Development of a Quality Manual for Microbiological Laboratories (QMML) that describes quality standards for CDC clinical, surveillance and research infectious disease laboratories.
- An Infectious Disease Test Review Board (IDTRB) that will review laboratory tests developed within CDC before they are shared outside of CDC to be sure the tests meet excellent quality standards and are suitable for their intended purpose.
- An example of the value of enhanced review occurred in the spring and summer of 2020 when CDC developed and validated a test to detect infection with influenza A and B and SARS-CoV-2, the virus that causes COVID-19. Test kit material performance was verified by multiple additional CDC laboratories to make sure that all the parts of the test performed as expected and were effective and accurate at identifying infectious agents. Three public health laboratories also verified the new test before it was distributed widely to confirm that the test worked well and was user-friendly. The test was successfully used by state and local public health laboratories during the 2020-2021 flu season, allowing them to conserve testing materials in short supply by simultaneously testing for infection by all three viruses.
- Method expert groups that are developing first-rate method validation standards and excellent method documentation requirements for each type of method (e.g., RT-PCR, ELISA) used in CDC infectious disease laboratories.
- An electronic Quality Management System (eQMS) that will be flexible, easy to use and facilitates CDC laboratory quality activities such as documenting and managing non-conforming events, corrective and preventive actions, training, equipment maintenance, standard operating procedures and more.
- Biannual external review of all CDC laboratories (clinical, surveillance, and research); clinical laboratories will be audited to meet CLIA requirements by Center for Medicaid and Medicare Services approved auditors.
The Laboratory Quality Plan sets a framework that encourages continuous quality improvement, while providing the quality assurance checks that ensure excellent test results.
In March 2023, CDC Advisory Committee to the Director (ACD) Laboratory Workgroup released their report on CDC policies, practices, and systems that should be established to meet CDC’s goal of ensuring the agency’s laboratories maintain a gold-standard level of quality using advanced laboratory science. The ACD Laboratory Workgroup provided input to the CDC regarding agency-wide activities related to implementation of improvements to strengthen the quality of work within CDC laboratories. The report offered 10 recommendations from the ACD Laboratory Workgroup, offering new, positive insights into effective implementation of CDC agency-wide laboratory quality improvements, many of the recommendations are consistent with those included within the CDC Laboratory Quality Plan and are either completed or being implemented and the CDC Moving Forward Initiative.
Building Laboratory Quality Capacity
CDC has ongoing targeted activities to build capacity and advance laboratory quality management across the agency, including piloting electronic tools for the advancement of laboratory quality system management in CDC laboratories.
CDC also provides trainings for laboratory scientists at the agency, in domestic and international public health laboratories, and in clinical laboratories.
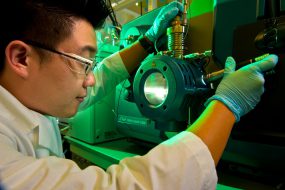
A CDC laboratory training facility prepares scientists for future work with infectious agents by training on required safety measures at all biosafety levels, including in two mock high-containment laboratory settings, Biosafety Levels 3 and 4.
CDC is committed to ensuring that Americans can rely on the agency to protect the public’s health and produce accurate, evidence-based science.