Uganda’s Disease Detectives Play Critical Role in Stopping Ebola
April 12, 2023
An Ebola outbreak confirmed in Uganda on September 20, 2022, was declared over by the Ugandan Ministry of Health and the World Health Organization on January 11, 2023. Over the course of the outbreak, 142 confirmed cases and 55 deaths were reported.
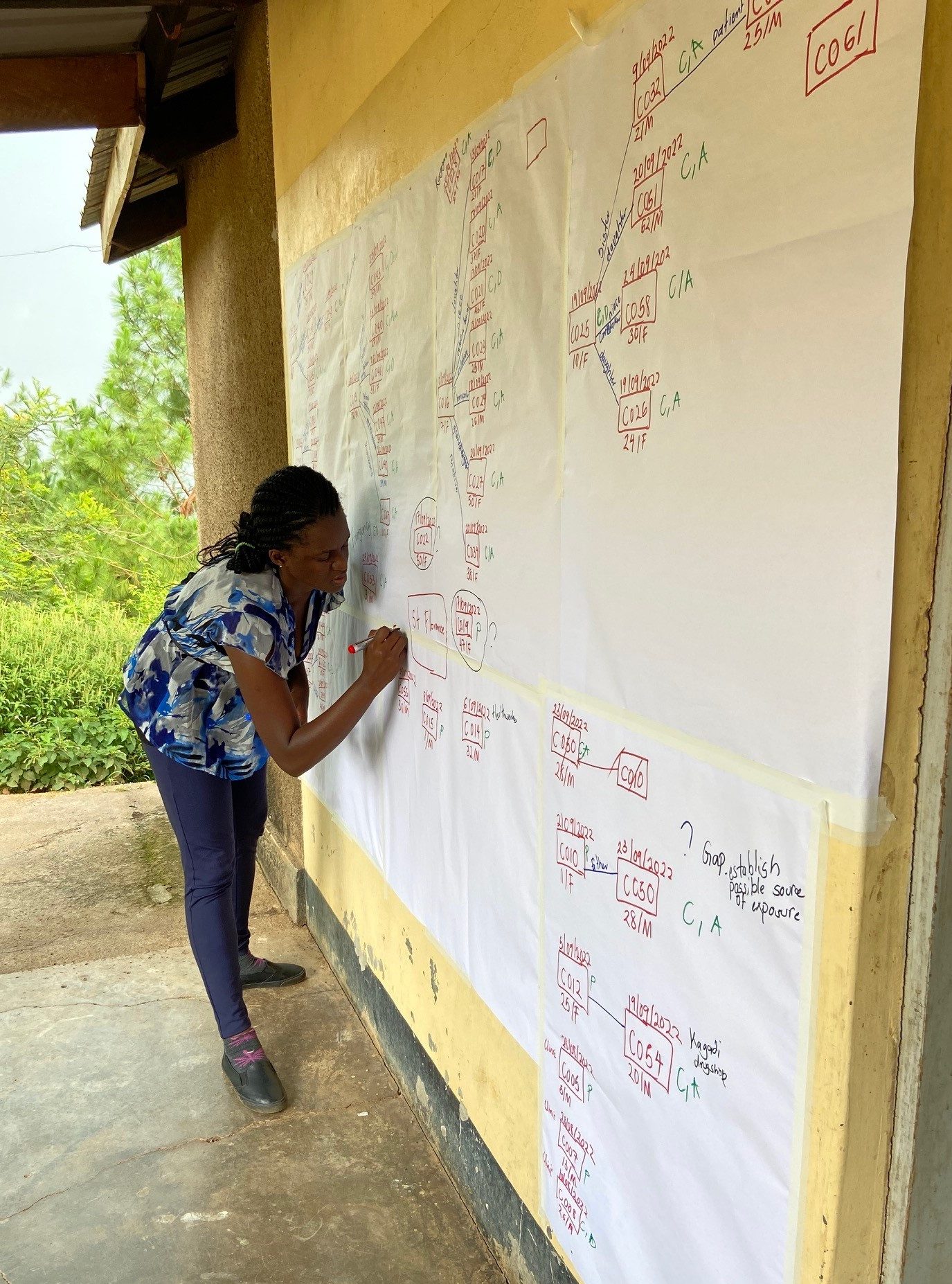
Ms. Mercy Wanyana, an Advanced Field Epidemiology Training Program Fellow in Uganda, assembles the first transmission chain for the 2022 Ebola virus outbreak in Uganda in October 2022. Photo: Julie Harris/CDC Uganda
Uganda is home to an extraordinary CDC-supported Field Epidemiology Training Program (FETP), referred to locally as the Public Health Fellows Program (PHFP). These PHFP fellows and graduates have been instrumental in bringing Uganda’s most recent Ebola outbreak to a close. The program, which began in 2015, boasts Advanced, Intermediate, and Frontline-level trainings. In 2022, the Advanced FETP included a total of 29 fellows. This post-master’s, full-time program trains multi-disciplinary burgeoning disease detectives who come into the program with experience ranging from human and veterinary medicine, biostatistics, epidemiology, pharmacy, environmental health, laboratory science, and wildlife health.
Each fellow is expected to carry out a well-rounded array of projects during the two-year program to promote a deeper understanding of epidemiological study design, outbreak investigation, quality improvement strategies, manuscript writing, leadership, public health economics, and scientific communication.
For Uganda’s FETP fellows, the intersection of wildlife and the dense population in the country provides ample opportunities to engage in a variety of outbreak investigations. In an average year, Uganda experiences outbreaks of anthrax, Rift Valley Fever, rabies, measles, Crimean-Congo Hemorrhagic Fever, poisonings, malaria, and tuberculosis—as well as chronic diseases and HIV. When the Uganda Ministry of Health began receiving reports of a new viral hemorrhagic fever outbreak, quickly identified as Ebola, the FETP fellows immediately began conducting case investigations to understand where cases were located and how they were becoming ill, and to ensure that sick people could be isolated as soon as possible.
The FETP fellows started by working backwards, identifying cases linked to specific healthcare facilities. One such facility in Mubende turned out to be an important amplifier of early infections in the Ebola outbreak, and other smaller, private clinics with limited infection prevention and control were also revealed to be sites of disease spread. Over the course of the Ebola outbreak, a strong network of FETP fellows and graduates took on key leadership roles in the response, working tirelessly to run efforts that ranged from contact tracing at district, regional, and national levels, to the establishment of databases and an alert management system, to conducting rapid studies to inform interventions to stop the outbreak.
Fellows built the first transmission tree, which both pieced together the early stage of the outbreak and facilitated the rapid linking of new cases to known chains of transmission. They also studied healthcare worker infections to better understand stigma, post-traumatic stress disorder among patients and their families, and specific risks encountered in patients’ homes. More than 30 studies are still underway and anticipated to provide meaningful insights to inform future prevention and mitigation strategies for the myriad harms caused by Ebola.

Dr. Julie Harris, CDC Uganda FETP Resident Advisor, sitting outside the Mubende District Health offices showing FETP fellows how to connect Ebola cases using exposure periods and onset periods into a transmission tree. Photo: CDC Uganda
Saudah Kizito, PhD, a second-year fellow, shared the following about her experience working on this outbreak: “Being one of the first people on the scene of the Ebola outbreak in Mubende made me feel like a soldier on the frontline. The work was hard and I sometimes felt like giving up, but the PHFP family’s leadership and organized strategy kept me going. I was able to use all of my disease detective talents in our case investigations. I went to churches, a gold mine, and shrines for the first time. The call from one of the first Ebola survivors, who ecstatically said, “Musawo (doctor), I have cheated death,” was the most gratifying moment. I am grateful to the fellowship program for transforming a clinical microbiologist and health manager into a passionate field epidemiologist.”
Julie Harris, PhD, the CDC Uganda Resident Advisor for FETP, is a strong believer in the power of the FETP program. “I am so proud of the fellows and that they were able to help control the Ebola outbreak with the Ministry of Health in Uganda. All of the work we’ve put into the training really came to fruition with this Ebola response. It would have taken much longer to control the outbreak without this army of disease detectives.”
Beyond the invaluable contributions of the FETP fellows to ending this Ebola outbreak, the CDC Uganda country office also dedicated 23 of its staff to supporting the response and 51 CDC deployers with Ebola response experience supported the Ministry of Health’s efforts through the duration of the outbreak.
CDC Uganda will continue to support the Ugandan Ministry of Health though PHFP to help ensure Uganda has a well-trained workforce ready to rapidly detect and respond to any future Ebola cases or other disease outbreaks.