Health Equity Indicators for Cardiovascular Disease (CVD) Toolkit
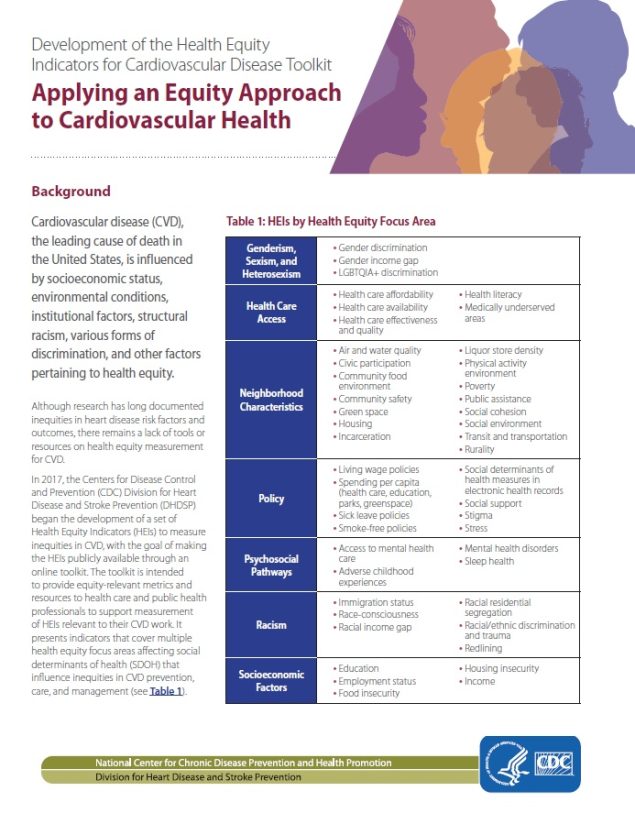
Applying an Equity Approach to Cardiovascular Health
Download this visual two-page summary: Health Equity Indicators for Cardiovascular Disease Toolkit: A Spotlight [PDF – 405 KB].
Download the Executive Summary: Applying an Equity Approach to Cardiovascular Disease [PDF – 307 KB].
Download the full Toolkit: Health Equity Indicators for Cardiovascular Disease Toolkit [PDF – 58 MB].
Cardiovascular disease (CVD) remains the leading cause of death in the United States. Despite advances in clinical care and treatment, stark inequities in cardiovascular risk factors [PDF – 561 KB] and outcomes persist by race and ethnicity, socioeconomic status, geography, and other factors.
Extensive research has shown that social, economic, and environmental factors shape health outcomes even more than what happens inside clinic walls. Therefore, measurement and evaluation approaches need to consider these factors, especially the systems and structures that influence them.
This toolkit presents health equity indicators (HEIs) across eight focus areas, or health equity themes, which influence inequities in cardiovascular disease prevention, care, and management as outlined in the HEI Conceptual Framework for CVD.
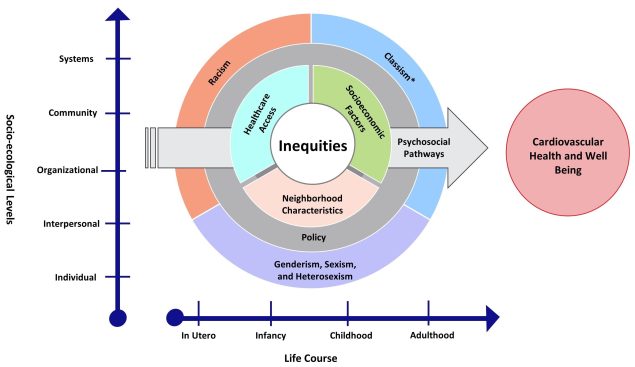
HEI Conceptual Framework for CVD
The Framework is based on the Social-Ecological Model and provides a model for understanding health inequities in CVD by graphically representing how HEIs are interconnected and occur through structural and socioenvironmental drivers, across socio-ecological levels, and throughout the lifespan.
Image description: A chart with X and Y axes showing nested circles. The X axis represents life course stages from left to right: in utero, infancy, childhood, and adulthood. The Y axis represents socioecological levels, from bottom to top: individual, interpersonal, organizational, community, and systems. The nested circles contain four layers that represent the health equity focus areas. The outer layer of the circle contains racism; classism; and genderism, sexism, and heterosexism; the next layer is policy; the third layer contains neighborhood characteristics, healthcare access, and socioeconomic factors. The innermost layer of the circle is labeled inequities. An arrow cuts across the nested layers to represent the psychosocial pathways focus area. The arrow points to the right, towards a circle labeled Cardiovascular Health and Well Being, to illustrate how cardiovascular health and well-being are affected by inequities across the 8 focus areas. The health equity focus area layers overlap each other to indicate that these areas are interconnected across socio-ecological levels and throughout the lifespan to influence cardiovascular health.
An indicator profile is available for each focus area (except for classism1) to describe the relevance of the indicators and provide specific measures that health departments or health care organizations may use to support their health equity efforts.
Learn more about the HEI Conceptual Framework for CVD
Inequities are greatly shaped by the consequences of historical and current societal norms, policies, and practices that systematically reduce access to resources for groups that have been marginalized.
The framework recognizes systemic inequities (e.g., racism, genderism/sexism/heterosexism, classism) that have produced policies that created or worsened socioeconomic deprivation, segregation of neighborhoods and schools, and unjust disparities in the quality of and access to health care. The discrimination, inequities, and barriers brought by these factors can create toxic stressors (acute and chronic) that affect psychosocial well-being across the course of an individual’s life.
Each of these factors affects and is affected by interpersonal relationships and social networks; the organizations that provide services or information to individuals; the built environments and communities in which individuals live, work, and play; and the broader systems or enabling environments that govern societal norms and policies. These domains, in and of themselves and in combination with other domains, shape and constrain the ability to engage in healthy behaviors and raise the risks of cardiovascular disease and mortality.
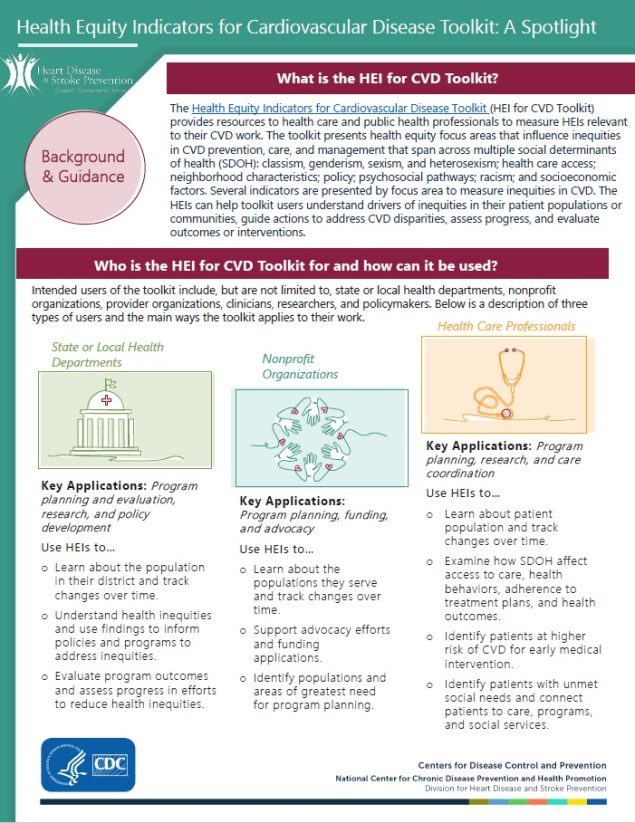
What is the HEI for CVD Toolkit?
The Health Equity Indicators for Cardiovascular Disease (HEI for CVD) toolkit includes a wide range of health equity indicators (HEIs) that can serve as a resource and inspire health care and public health professionals to incorporate health equity–relevant metrics and processes into strategic planning, site selection, and evaluation.
Health equity is the state in which everyone has a fair and just opportunity to attain their highest level of health.2 HEIs represent measurable constructs that have been shown to be important for understanding the causes of inequities in cardiovascular disease (CVD) and can be used to measure health inequities.
The toolkit includes the following components:
- Health Equity Indicator Profiles provide definitions and measurement guidance for each HEI. Case Examples and Field Notes are included throughout.
- Glossary of Terms provides definitions for frequently used terms and concepts in the HEI for CVD Toolkit.
- Related Resources are other CDC and external resources that support health equity measurement and evaluation and advance health equity work.
Who is the HEI for CVD Toolkit for?
The toolkit provides local health jurisdictions, city governments, health care organizations, and other agencies with information about equity promoting activities and associated measures to improve cardiovascular health in disproportionately affected communities.
What is the intended use of the HEI for CVD Toolkit?
Indicators profiled in this toolkit can be used to understand inequities at institutional and structural levels and measure efforts to reduce inequities in CVD and mortality rates within specific populations.
These indicators can serve as a resource for health care and public health professionals who seek to incorporate equity-relevant metrics, measurement considerations, and inclusive community engagement processes into their work. However, they are not a comprehensive set of all measures that matter for cardiovascular equity.
Public health and health care professionals can use this toolkit to
- Identify gaps between what is currently measured and what can be measured.
- Consider new data collection methods for identifying root causes and key drivers of inequities.
- Consider upstream and structural factors that influence lifestyles and behaviors, environments and communities, and access to early detection and treatment of CVD.
- Identify possible indicators and measures that can bolster current evaluation efforts.
- Use resources and case examples to guide health equity measurement and evaluation.
How can I navigate the HEI for CVD Toolkit?
Visit specific focus areas that correlate with poor cardiovascular health (e.g., Policy) under each Health Equity Indicator Profile. Each focus area provides a definition of the focus area and lists indicators and measures for the focus area.
Case Examples and Field Notes are included throughout the Health Equity Indicator Profiles. The Case Examples and Field Notes include short summaries that describe an organization’s experience with gathering data for specific indicators and lessons learned.
Selecting an indicator (e.g., Spending Per Capita) from the focus areas shows users the definition of each indicator, presents evidence on the importance of the indicator related to health and CVD, lists measures for operationalizing the indicator, and lists case examples related to the indicator if applicable.3 To learn how to assess indicators, users can view the measures (e.g., Per Capita Spending on Health Care). Measure (e.g., Per Capita Spending on Health Care) provide users with data sources, measurement guidance, and relevant case examples (if applicable).
For additional resources on how to support health equity work, visit the Related Resources page. Users should refer to the Glossary of Terms page to find definitions for commonly used terms in the HEI for CVD Toolkit.
How was the HEI for CVD Toolkit developed?
References and Footnotes
- Although classism is an important determinant of CVD inequities, indicators of classism are similar to those specified for other focus areas (e.g., racism, socioeconomic factors, neighborhood characteristics, policy). Therefore, there is not a separate indicator profile for classism.
- Centers for Disease Control and Prevention. Advancing Health Equity in Chronic Disease Prevention and Management. Updated December 8, 2022. Accessed June 3, 2022.
- Not all indicators and measures have a relevant case example.