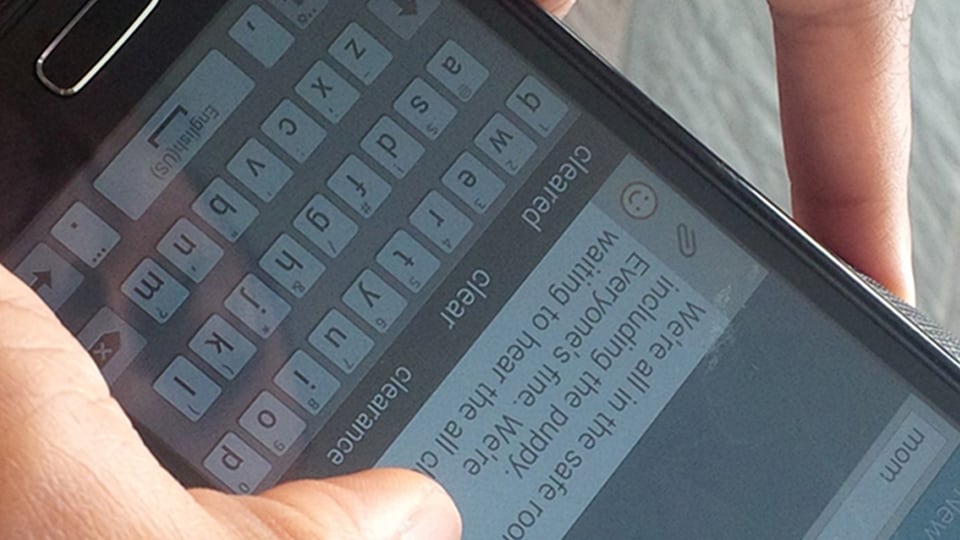
Ensure peace of mind during emergencies: plan communication and reunification with loved ones.
Featured
Gather supplies & learn skills to respond.
Plan, practice, and involve your family.
Prioritize community preparedness & resilience.
Learn More
Build resilience for a community through training, donations, and volunteerism.
- Practical skills encompass self-help and life-saving lessons.
- Arrange and secure your prescriptions in readiness for an emergency.
- Gather insurance cards, and personal identification, and have emergency action plans.
- Extended power outages pose great risks.
- Personal preparedness and mutual support lay the foundation for effective emergency response.
- Empowering communities through shared responsibility and accessible resources
- Inspire your family & community with healthy habits like handwashing and vaccinations.