For Clinicians
Conjunctivitis can result from many causes, including viruses, bacteria, allergens, contact lens use, chemicals, fungi, and certain diseases.
Schools should allow infected children to remain in school once any indicated therapy is implemented, except when viral or bacterial conjunctivitis is accompanied by systemic signs of illness. However, infected students should refrain from attending school if their behavior is such that they cannot avoid close contact with other students.
Viral Conjunctivitis
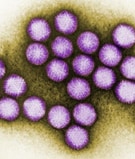
Colorized transmission electron micrograph of adenovirus.
(CDC Public Health Image Library)
The following viruses can cause viral conjunctivitis, with adenoviruses being one of the most common causes:
- Adenoviruses
- Rubella virus
- Rubeola (measles) virus
- Herpesviruses, including
- Herpes simplex virus
- Varicella-zoster virus, which also causes chickenpox and shingles
- Epstein-Barr virus, which also causes infectious mononucleosis (mono)
- Picornaviruses, such as coxsackievirus A24 and enterovirus 70 (which has caused outbreaks in other countries)
Viral conjunctivitis is highly contagious. Most viruses that cause conjunctivitis spread through hand-to-eye contact by hands or objects that are contaminated with the infectious virus. Having contact with infectious tears, eye discharge, fecal matter, or respiratory discharges can contaminate hands. Viral conjunctivitis can also spread by large respiratory tract droplets. As viral conjunctivitis can be highly contagious, infected individuals should be counseled to prevent transmission e.g., washing hands frequently, using separate towels, and avoiding close contact with others during the period of contagion.
Most cases of acute, infectious conjunctivitis in adults are viral and self-limited; these cases do not require antimicrobial treatment. Antiviral medication may be used to treat more serious forms of conjunctivitis, such as conjunctivitis caused by herpes simplex virus or varicella-zoster virus.
Depending on the cause of viral conjunctivitis, some patients may have additional symptoms or conditions, such as the following:
- Common cold, flu, or other respiratory infection
- Pharyngoconjunctivial fever – a syndrome that can produce conjunctivitis as well as a fever and sore throat, and is most commonly caused by infection with adenovirus serotypes 3, 4, and 7
- Epidemic keratoconjunctivitis – a more severe type of conjunctivitis, commonly caused by infection with adenovirus serotypes 8, 19, and 37
- Acute hemorrhagic conjunctivitis – a type of conjunctivitis that is often associated with large epidemics worldwide, especially in the tropical and subtropical regions. The viruses most commonly associated with it include enterovirus 70, coxsackievirus A24, and adenoviruses.
- Herpetic keratoconjunctivitis – a type of conjunctivitis associated with herpes simplex virus and blister-like lesions on the skin; it may affect only one eye
- Rubella and rubeola (measles) – conjunctivitis can occur with these viral rash illnesses which are usually accompanied by rash, fever, and cough
Bacterial Conjunctivitis

This illustration shows Streptococcus pneumoniae, one common cause of bacterial conjunctivitis.
Many species of bacteria can cause bacterial conjunctivitis including
- Haemophilus influenzae
- Streptococcus pneumoniae
- Moraxella catarrhalis
- Chlamydia trachomatis
- Staphylococcus aureus
- Moraxella lacunata
- Neisseria gonorrhea
- Neisseria meningitides
Bacterial conjunctivitis can spread from person to person in many ways. These include from hand-to-eye contact, via eye contact with contaminated objects, through sexual encounters with eye to genital contact, or vertically from mother to baby. Bacteria can also spread by large respiratory tract droplets. Alternatively, changes in the usual bacteria that live on the conjunctiva can also cause conjunctivitis.
Signs and symptoms of bacterial conjunctivitis overlap with other causes of conjunctivitis, including viral and allergic conjunctivitis, which can make diagnosis difficult. Typical signs and symptoms include:
- Red eye
- Purulent discharge that causes eyelids to be matted together
- Chemosis
- Decreased vision
- Eyelid swelling and pain
Contact lens wearers with bacterial conjunctivitis are at higher risk of bacterial keratitis. They should be asked to remove their contact lenses, treated with topical antibiotics, and promptly evaluated by an ophthalmologist.
Types of bacterial conjunctivitis include:
Acute bacterial conjunctivitis
- Is the most common form of bacterial conjunctivitis
- In children is often caused by Haemophilus influenzae, Streptococcus pneumoniae, or Moraxella catarrhalis
- Is typically self-limited within 1–2 weeks, but topical antibiotic therapy may reduce the duration of disease
Hyperacute bacterial conjunctivitis
- Is a very rare and severe type of conjunctivitis with rapid onset and progression, as well as severe symptoms, including massive exudate, severe chemosis, eyelid swelling, marked hyperemia, pain, and decreased vision
- Caused by Neisseria gonorrhoeae or Neisseria meningitidis
- Requires both parenteral and topical antibiotic therapy
- Can progress to corneal infiltrates, melting and perforation and vision loss if not treated promptly by an ophthalmologist
Chronic bacterial conjunctivitis
- Defined as symptoms lasting for at least 4 weeks
- Common causes include by Staphylococcus aureus or Moraxella lacunata
- Often occurs with blepharitis (inflammation of the eyelid), which can cause flaky debris and warmth along the lid
- People with this condition should see an ophthalmologist
Chlamydial conjunctivitis
- In neonates
- Infection usually is acquired during delivery of infants born to mothers with Chlamydia trachomatis
- It is called chlamydial ophthalmia neonatorum in the first 4 weeks of life
- Usually symptoms develop 5 to 14 days after birth; symptoms can develop earlier if the amniotic sac is ruptured during delivery Concurrent chlamydial infection elsewhere in their bodies (e.g., lungs, nasopharynx) is common
- Approximately 50% of infants who develop pneumonia have a history of chlamydial conjunctivitis
- Presenting symptoms include watery, mucopurulent, or bloody discharge, marked swelling with red, thickened, and friable conjunctivae, and a pseudomembrane may form
- Among sexually active people
- Acute disease is commonly unilateral with hyperemia and purulent discharge and caused by Chlamydia trachomatis subtypes D through K
- Many patients will have a mild prolonged course
- Presenting with chlamydial conjunctivitis will have an associated genital infection
- Trachoma
- The leading global cause of preventable blindness
- A chronic follicular conjunctivitis caused by Chlamydia trachomatis subtypes A through C
- Causes scarring of the inner eyelid which can cause the eyelashes to turn in and scratch the cornea (trichiasis), leading to permanent damage
- Transmitted from person to person through contact with discharge from the eyes or nose of an infected person, through shared items, or by flies spreading ocular secretions
- Repeat infections occur in children younger than 10 years of age
- Common in developing countries where access to water and sanitation may be poor
- Is targeted for elimination by the World Health Organization through an innovative, multi-faceted public health strategy known as S.A.F.E. (Surgery to correct the advanced, blinding stage of the disease (trichiasis), Antibiotics to treat active infection, Facial cleanliness and, Environmental improvements in the areas of water and sanitation to reduce disease transmission)
Learn more about trachoma and other hygiene-related diseases.
Gonococcal conjunctivitis
- In neonates
- Infection usually is acquired during delivery of infants born to mothers with Neisseria gonorrhoeae
- It is called gonococcal ophthalmia neonatorum in the first 4 weeks of life
- It usually presents in the first 2 days of life and can be associated with bacteremia and meningitis
- Prompt treatment is recommended as there is concern for corneal perforation, scarring, and blindness
- Prophylaxis with erythromycin ophthalmic ointment is currently recommended by the U.S. Preventive Services Task Force immediately after birth and is legally mandated in most states
- Among sexually active people
- Symptoms typically develop 24-48 hours following exposure to urogenital secretions containing N. gonorrhoeae
- Symptoms include red eyes, thick pus in the eyes, and swelling of the eyelids and conjunctiva
- Gonococcal conjunctivitis in adults is uncommon and treatment data are limited; an infectious disease specialist should be consulted
Scanning electron micrograph of an Ambrosia trifida plant, more commonly known as ragweed.
(CDC Public Health Image Library)
Allergic Conjunctivitis
Allergic conjunctivitis is common in people who have other signs of allergic disease, such as hay fever, asthma, and eczema. It is caused by the body’s reaction to certain substances it is allergic to, such as
- Pollen from trees, plants, grasses, and weeds
- Dust mites
- Animal dander
- Molds
- Contact lenses and lens solution
- Cosmetics