Division of Cancer Prevention and Control At A Glance

CDC’s Division of Cancer Prevention and Control is a leader in efforts to prevent and find cancers early and to improve the health of cancer survivors. The division works with states and other federal agencies to collect a census of cancer cases to provide United States Cancer Statistics each year. Many DCPC programs and activities work with national organizations and state and local health agencies to help Americans lower their cancer risk by increasing the use of effective cancer prevention strategies and screening tests.
What We Do

With an appropriated FY 2021 budget of about $355 million, DCPC works to reduce cancer risk factors and promote cancer screenings to help every person have an equal opportunity to achieve the best health possible. To meet this goal, DCPC works to:
- Find out how many Americans have cancer and provide this information online through the US Cancer Statistics Data Visualizations Tool.
- Study interventions to find out what works best to prevent cancer or catch it early.
- Fund and guide states, tribes, and territories to use interventions that work.
- Share information to help all Americans understand the risk factors for cancer and how to reduce them.
Why We Do It
Cancer is the nation’s second leading cause of death, but more than half of cancer deaths could be prevented through healthy choices, screening, and vaccinations.
In the United States:

1.7 MILLION
people diagnosed with cancer each year.

600,000 DEATHS
from cancer each year.
1 IN 3 PEOPLE
will have cancer in their lifetime.

$185 BILLION
in annual cancer care costs.
How We Do It
Collect Data on Cancer Cases and Treatment
To help Americans prevent cancer and catch it early, we need to know what cancers are being diagnosed, among which groups of people, and where. DCPC runs the National Program of Cancer Registries (NPCR) and coordinates with other federal agencies to collect data for notifiable cancer cases in the United States. Through the NPCR, CDC funds 46 states, the District of Columbia, Puerto Rico, the US Pacific Island Jurisdictions, and the US Virgin Islands to collect cancer registry data.
These data can be used to answer questions such as:
- Are more or fewer people getting colon cancer this year compared to last year?
- Are there geographic areas where women are finding out they have breast cancer at a late stage, when it’s harder to treat?
- What groups of people are most likely to get skin cancer?
Data are shared with groups working to prevent cancer, like state comprehensive cancer control coalitions. The coalitions work to fix any identified problems—for example, some people might not be getting the cancer screening tests they need—and then track changes in the cancer registry data to find out if their solutions are working.
Examples of Our Impact
- South Carolina’s breast and cervical cancer early detection program uses cancer registry data to screen more people for cancer.
- Kentucky uses their data to investigate why children in the state have higher cancer rates than children in the United States as a whole.
- Delaware is closing the gap in prostate cancer deaths among African American men.
Help People Understand Their Risk of Cancer and the Importance of Screening

In 2015, CDC launched the Bring Your Brave campaign to educate women younger than age 45 about breast cancer. The campaign shares real stories about prevention, risk, family history, and cancer survivors to inspire young women to learn their risk of breast cancer and talk with their doctor about how to reduce it.
CDC’s Inside Knowledge About Gynecologic Cancer campaign raises awareness among women and medical professionals about the five main types of gynecologic cancer: cervical, ovarian, uterine, vaginal, and vulvar. These cancers are often discussed as a group, but each is unique and has different signs, symptoms, risk factors, and prevention strategies.
In 1999, CDC launched the Screen for Life: National Colorectal Cancer Action Campaign to raise awareness of and increase screening for colorectal cancer. This ongoing campaign is based on extensive research that found that men and women aged 45 or older are at highest risk of getting colorectal cancer.
Examples of Our Impact
- The Bring Your Brave campaign has been seen or heard nearly 160 million times across social media, blogs, digital display ads, and earned media.
- The Inside Knowledge campaign’s public service announcements (PSAs) have been seen or heard 5.7 billion times, for a donated ad value of nearly $235 million. When combined with paid media across search engines, social media, digital display, and paid digital advertising, Inside Knowledge has generated 8 billion impressions overall.
- CDC’s Screen for Life PSAs have been seen or heard nearly 21 billion times, for a total donated ad value of over $300 million.
Promote Colorectal Cancer Screening for US Adults

Of cancers affecting both men and women, colorectal cancer is the second leading cancer killer in the United States, but it doesn’t have to be. Screening can find precancerous polyps—abnormal growths in the colon or rectum—so they can be removed before turning into cancer. Screening also helps find colorectal cancer at an early stage, when treatment often leads to a cure.
The US Preventive Services Task Force (USPSTF) recommends colorectal cancer screening for adults aged 45 to 75.
CDC’s Colorectal Cancer Control Program funds 20 states, 8 universities, 2 tribal organizations, and 5 other organizations to increase colorectal cancer screening rates for people aged 45 to 75. To meet this goal, the program uses strategies recommended by the Community Preventive Services Task Force, such as patient and provider reminders in health system clinics.
Examples of Our Impact
- As of March 2020, Colorectal Cancer Control Program recipients had partnered with 831 health system clinics that serve more than 1.3 million patients who are eligible for colorectal cancer screening. Among clinics recruited in the first program year, screening rates increased from a mean rate of 42.4% in 2016 to 56.4% in 2019. In contrast, national screening rates for the overall United States have consistently increased by only 1 to 2 percentage points every 2 years.
- Adults aged 50 to 75 years who reported no colorectal cancer screening decreased from 27.4% in 2012 to 21.6% in 2020, a 5.8 percentage-point reduction, representing 3,917,775 fewer people screened in 2012 than in 2020. Compared to 2012, all states showed an increase in the percentage of people screened in 2020.
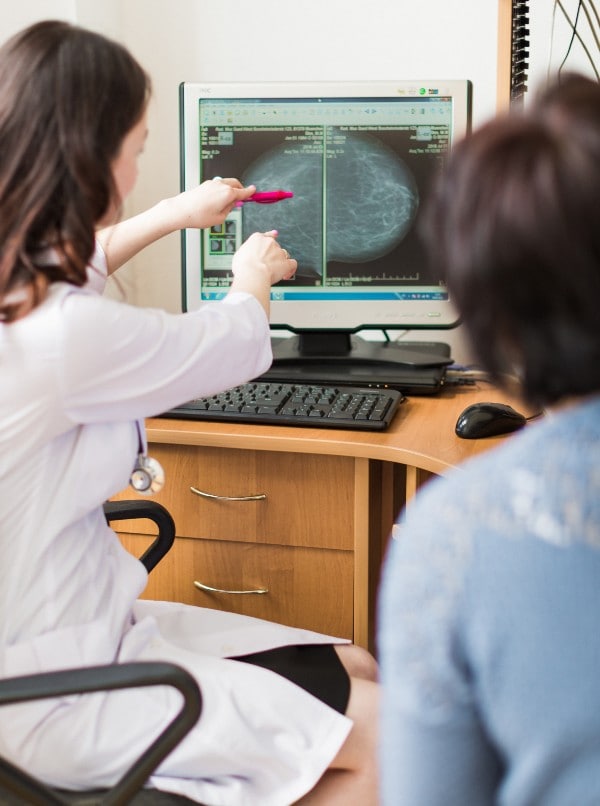
Promote Breast and Cervical Cancer Screening

Regular mammograms can lower the risk of dying of breast cancer. The USPSTF recommends that women aged 50 to 74 who are at average risk should have a screening mammogram every 2 years. Average risk means women without symptoms who do not have a preexisting breast cancer, high-risk breast lesion, a known genetic mutation, or a history of chest radiation at a young age.
For cervical cancer, two screening tests can help prevent the disease or find it early. The Pap test can find abnormal cells in the cervix that may turn into cancer. The human papillomavirus (HPV) test identifies the virus that can cause these abnormal cell changes. The Pap test is recommended for women aged 21 to 65. The HPV test, either with the Pap test or alone, can be used to screen for cervical cancer in women aged 30 to 65.
CDC’s National Breast and Cervical Cancer Early Detection Program (NBCCEDP) funds all 50 states, the District of Columbia, Puerto Rico, 5 US-Affiliated Pacific Islands, and 13 tribes or tribal organizations to provide breast and cervical cancer screening and diagnostic services to women with low incomes and little or no health insurance. These services include mammograms, breast MRIs, Pap tests, and HPV tests; follow-up testing if results are abnormal; and referrals to treatment if needed.
Women who are diagnosed with cancer through the NBCCEDP may qualify for treatment through Medicaid.
Examples of Our Impact
Since 1991, NBCCEDP-funded programs have:
- Served more than 6.0 million women.
- Provided more than 15.6 million breast and cervical cancer screening exams.
- Diagnosed 74,891 invasive breast cancers and 23,707 premalignant breast lesions.
- Diagnosed 5,066 invasive cervical cancers and 232,428 premalignant cervical lesions, of which 39% were high grade (more likely to progress to cancer).
Fund States to Prevent and Control Cancer

Comprehensive cancer control involves state and local health departments, organizations, researchers, health care providers, cancer survivors, and their families coming together to find ways to reduce cancer and improve the lives of cancer survivors in their communities. CDC’s National Comprehensive Cancer Control Program funds all 50 states, the District of Columbia, 7 US territories and freely associated states, and 8 tribes or tribal organizations to:
- Build groups of partners that share resources and expertise to fight cancer.
- Use data from cancer registries, behavioral risk factor surveys, and other sources to learn more about the cancers and risk factors that affect their communities most.
- Develop and use strategic plans to address these cancers and risk factors.
- Support lifestyle changes to prevent cancer.
- Improve access to screening and treatment.
- Reduce cancer risk factors and improve cancer outcomes for groups affected by health disparities.
- Respond to the physical, financial, and emotional needs of cancer survivors and their families.
Examples of Our Impact
- The Iowa Comprehensive Cancer Control Program (ICCCP) worked with partners to increase colorectal cancer screening in Federally Qualified Health Centers (FQHCs). This collaboration has achieved an 17.5% increase in the colorectal cancer screening rate within participating FQHCs. Six of the FQHCs have updated their data systems to increase colorectal cancer screening connections. This work with FQHCs has reached 22,825 Iowans (aged 50–75). These efforts were done before the recommended change in age eligibility to start screening at age 45.
- Radon, a naturally occurring gas, is the second leading cause of lung cancer death in the United States. The NC Comprehensive Cancer Control Program worked with the state’s radon control program to increase awareness of the harmful effects of high radon levels in homes. They created a Radon in Real Estate continuing education course to help real estate agents educate home buyers about the benefits of testing for radon. The Radon in Real Estate course was first offered in 2021, and 387 real estate agents have taken it to date.
Health Equity Highlight: National Breast and Cervical Cancer Early Detection Program (NBCCEDP)
The Challenge
Despite the availability of screening tests, deaths from breast and cervical cancer occur more often among women who are uninsured or underinsured.
CDC’s Approach
NBCCEDP helps women with low incomes and little or no health insurance get timely breast and cervical cancer screening, diagnostic, and treatment services. The program also offers patient navigation to help women overcome barriers to getting quality care.
Over its 30-year history, NBCCEDP has reached nearly 6.0 million women across the United States. The screenings offered through this program have found more than 74,891 breast cancers and 5,066 cervical cancers that might not have been found.