FIGURE. Rate of reported foodborne disease outbreaks per 100,000 standard population* and number of outbreaks,† by state and major etiology group§ --- United States, 2007
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Surveillance for Foodborne Disease Outbreaks --- United States, 2007
Foodborne agents cause an estimated 76 million illnesses annually in the United States (1). Outbreak surveillance provides insights into the causes of foodborne illness, types of implicated foods, and settings of foodborne infections that can be used in food safety strategies to prevent and control foodborne disease. CDC collects data on foodborne disease outbreaks submitted from all states and territories. This report summarizes epidemiologic data for the 1,097 reported outbreaks occurring during 2007 (the most recent finalized data), which resulted in 21,244 cases of foodborne illness and 18 deaths. Among the 497 foodborne outbreaks with a laboratory-confirmed single etiologic agent reported, norovirus was the most common cause, followed by Salmonella. Among the 18 reported deaths, 11 were attributed to bacterial etiologies (five Salmonella, three Listeria monocytogenes, two Escherichia coli O157:H7, and one Clostridium botulinum), two to viral etiologies (norovirus), and one to a chemical (mushroom toxin). Four deaths occurred in outbreaks with unknown etiologies. Among the 235 outbreaks attributed to a single food commodity, poultry (17%), beef (16%), and leafy vegetables (14%) were most often the cause of illness. Public health, regulatory, and agricultural professionals can use this information when creating targeted control strategies and to support efforts to promote safe food preparation practices among food employees and the public.
A foodborne disease outbreak is defined as the occurrence of two or more similar illnesses resulting from ingestion of a common food. State, local, and territorial health departments use a standard, Internet-based form to voluntarily submit reports of foodborne outbreaks to the Foodborne Disease Outbreak Surveillance System, and a toolkit for investigation and reporting of outbreaks is used to guide reporting officials.*
This report includes outbreaks occurring in 2007 and reported to CDC by May 3, 2010. Population-based rates of reported outbreaks were calculated for each state using U.S. Census estimates of the 2007 state populations.† Reported outbreak data include the number of illnesses, hospitalizations, and deaths associated with each outbreak; the etiologic agent, either confirmed or suspected§; and the implicated food vehicle. CDC classifies implicated foods into the following 17 food commodities: finfish, crustaceans, mollusks, dairy, eggs, beef, game, pork, poultry, grains-beans, oils-sugars, fruits-nuts, fungi, leafy vegetables, root vegetables, sprouts, and vegetables from a vine or stalk (2). Outbreaks in which the reported food vehicle contained ingredients from only one commodity were assigned to that commodity; those in which the reported food vehicle contained ingredients from more than one commodity, could not be grouped in one of the 17 commodities (e.g., coffee, alcohol), or contained insufficient information for commodity assignment were not attributed to any commodity.
Public health officials from 48 states, Puerto Rico, and the District of Columbia reported 1,097 foodborne disease outbreaks; multistate outbreaks involving two additional states (Montana and Nevada) were reported indirectly (Figure). The number of foodborne disease outbreaks (1,097) reported to CDC in 2007 was 8% lower than the annual average (1,193) reported for 2002--2006, and the number of outbreak-related illnesses (21,244 versus 25,079) was 15% lower. The number of outbreaks reported by each state or territory during 2007 varied from 0 to 149 (median: 0.30 outbreaks per 100,000 population; range: 0.03--1.90). A confirmed or suspected single etiologic agent was identified in 698 (64%) outbreaks (497 confirmed, 201 suspected), resulting in 15,477 (73%) illnesses (Table 1). Among the 363 outbreaks with an unknown etiology (5,122 illnesses), 257 outbreaks (71%) with 3,904 illnesses (76%) also had an unknown food vehicle. Outbreaks in which few persons became ill were more likely to have an unknown etiology. Among the 146 outbreaks in which no more than two persons became ill, 51% had no confirmed or suspected etiology. In contrast, no confirmed or suspected etiology was identified for 40% of 346 outbreaks involving three to seven illnesses, 30% of the 89 outbreaks involving eight or nine illnesses, and 24% of the 519 outbreaks involving 10 or more illnesses. The most common reasons reported for not identifying an etiology or food vehicle were 1) delayed reporting of illnesses to the health department, 2) too many food items were consumed by ill persons to identify a single food as the contaminated vehicle, and 3) human or food sample test results were unavailable, either because samples could not be obtained or because tests were negative for the pathogens evaluated.
Among the 497 outbreaks (12,767 illnesses) with a confirmed single etiologic agent, bacteria caused 259 (52%) outbreaks with 6,441 (50%) illnesses, viruses caused 199 (40%) outbreaks with 6,120 (48%) illnesses, chemical agents caused 34 (7%) outbreaks with 141 (1%) illnesses, and parasites caused five (1%) outbreaks with 65 (1%) illnesses. Norovirus was the most common cause of illness, accounting for 193 (39%) of the confirmed single-etiology outbreaks and 97% of those caused by viruses. Salmonella was the second most common, causing 136 (27%) confirmed single-etiology outbreaks and 53% of those attributed to bacteria. Among Salmonella serotypes identified, Enteritidis was the most common, causing 28 confirmed single-etiology outbreaks with 555 illnesses. Shiga toxin-producing E. coli (STEC) caused 40 of the confirmed single-etiology outbreaks (15% of those attributed to bacteria), of which 39 were caused by serogroup O157.
Among the 18 multistate foodborne disease outbreaks (i.e., outbreaks in which exposure to the etiologic agent or agents occurred in more than one state), 10 were attributed to Salmonella, six to E. coli O157:H7, one to C. botulinum, and one to norovirus. Foods associated with multistate Salmonella outbreaks included commercially-processed frozen pot pies (401 illnesses, three deaths), commercially-processed vegetable snacks (87 illnesses), eggs (81 illnesses), spinach/lettuce (76 illnesses), beefsteak tomatoes (65 illnesses), raw tuna (44 illnesses), ground beef (43 illnesses), cheese (20 illnesses), alfalfa sprouts (15 illnesses), and raw fresh basil (11 illnesses). Of the six multistate outbreaks of E. coli O157:H7 infection, the vehicle for five was ground beef (117 illnesses) and the vehicle for one was commercially-processed frozen pepperoni pizzas (27 illnesses). The vehicle for the C. botulinum toxin outbreak (eight illnesses) was commercially canned hotdog chili sauce. The one multistate outbreak caused by norovirus was associated with raw oysters (40 illnesses).
A food vehicle was identified in 470 (43%) outbreaks associated with 9,818 illnesses, of which 235 (50%) with 4,119 (42%) illnesses were linked to a food vehicle with ingredients limited to only one of the 17 commodities (Table 2). The commodities most commonly implicated in outbreaks were finfish (41 outbreaks), poultry (40 outbreaks), and beef (33 outbreaks); the commodities associated with the most illnesses were poultry (691 illnesses), beef (667 illnesses), and leafy vegetables (590 illnesses). The pathogen-commodity pairs responsible for the most outbreak-related illnesses were norovirus in leafy vegetables (315 illnesses), E. coli O157:H7 in beef (298 illnesses), and Clostridium perfringens in poultry (281 illnesses).¶
Two of the three largest reported outbreaks in 2007 were caused by Salmonella. The vehicles were hummus (802 illnesses) and commercially-processed frozen pot pies (401 illnesses and three deaths). The second largest outbreak was caused by norovirus at a conference hotel (526 illnesses); several shared food items were the suspected vehicles. The largest outbreaks assigned to a single food commodity were caused be a chicken dish contaminated with C. perfringens (132 illnesses), leafy vegetable salad contaminated with norovirus (128 illnesses), chili beans contaminated with C. perfringens (125 illnesses), and beef contaminated with E. coli O157:H7 (124 illnesses).
Reported by
A Boore, PhD, KM Herman, MSPH, AS Perez, MPH, CC Chen, MPH, DJ Cole, DVM, PhD, BE Mahon, MD, PM Griffin, MD, IT Williams, PhD, Enteric Diseases Epidemiology Br, Div of Foodborne, Waterborne, and Environmental Diseases, National Center for Emerging and Zoonotic Infectious Diseases; AJ Hall, DVM, Epidemiology Br, Div of Viral Diseases, National Center for Immunization and Respiratory Diseases, CDC.
Editorial Note
Many factors in detection and reporting likely contribute to variation in the annual rate of outbreaks reported by states. However, the emergence of two new norovirus strains in 2006 likely resulted in a relative increase in norovirus outbreaks in 2006 and early 2007 (3,4). Subsequently, increased population immunity to these new strains might have contributed to the relative decrease in norovirus outbreaks in 2007. This pattern of emergence of new norovirus strains corresponding with a spike in norovirus outbreaks appears to occur worldwide approximately every 2--3 years (5). The overall decrease in reported outbreaks in 2007 largely resulted from a reduction in the proportion caused by norovirus. The number of outbreaks caused by bacterial agents in 2007 was similar to the 2002--2006 average.
Despite the decrease in 2007, norovirus was still the leading cause of reported outbreaks and outbreak-related illnesses. Norovirus contamination can occur before the point of food preparation and service, as indicated by recent multistate and international norovirus outbreaks associated with oysters, raspberries, and delicatessen meat (6--8). The large number of norovirus foodborne outbreaks indicates a need for continued attention to preventing food contamination by food employees who come into contact with ready-to-eat foods. Norovirus outbreaks are thought to largely result from contamination of food via the unwashed or improperly washed hands of food workers shedding norovirus in their stools. Enhanced food safety training for food employees that work with ready-to eat foods, and the presence of a certified food protection manager in food service and retail establishments, as recommended by the Food and Drug Administration's (FDA) Food Code,** might help to reduce the number of outbreaks and outbreak-related illnesses resulting from contamination in food service establishments, if adopted by all states and territories. To date, 49 of 50 states and three of six U.S. territories have adopted codes patterned after versions of the FDA Food Code (9), but the specific components of individual state regulations vary.
The findings in this report are subject to at least four limitations. First, only a small proportion of all foodborne illnesses reported each year are identified as associated with outbreaks. For example, in FoodNet sites during 2007, only 5.4% of Salmonella illnesses reported to CDC were part of a recognized outbreak (10). Some illnesses reported as sporadic likely are not recognized as being part of a reported outbreak or are part of undetected outbreaks. All outbreak-associated illnesses might not be identified during an investigation, and smaller outbreaks might not come to the attention of public health authorities. Second, because of competing priorities in health departments, not all recognized clusters of illness are investigated or reported to CDC. Third, many reported outbreaks had an unknown etiology, an unknown food vehicle, or both, and conclusions drawn from outbreaks with a confirmed or suspected etiology or food vehicle might not apply to outbreaks of unknown etiology or food source. Finally, CDC's outbreak surveillance database is dynamic; reporting agencies can submit new reports and can change or delete previous reports at any time as new information becomes available. Therefore, the results of this analysis represent data available at a single point in time and might differ from those published earlier or subsequently.
Although most foodborne illnesses are sporadic, investigations of those that occur as part of recognized outbreaks provide insights into the agents, food vehicles, and food handling practices that lead to foodborne illness. Unlike laboratory-based surveillance systems, in which the sources of illnesses are rarely reported, the investigation and reporting of outbreaks provides important epidemiologic information that can be used to inform food safety policy. For example, recognition of E. coli O157:H7 infections caused by contaminated ground beef in the early 1990s led to regulatory and industry interventions that contributed to a decline in E. coli O157:H7 contamination of ground beef. Determining the etiologic agent and the food vehicle for small outbreaks is inherently more difficult because fewer affected persons are available to provide clinical specimens and food histories. However, even when no etiology or food vehicle is confirmed as the cause of foodborne illnesses, the investigative process provides health departments the opportunity to detect and remedy problems with food storage, preparation, and service that might prevent future outbreaks. Further information on foodborne disease outbreaks, including the Foodborne Outbreak Online Database (FOOD), is available at http://www.cdc.gov/foodborneoutbreaks.
Acknowledgments
The findings in this report are based, in part, on contributions by state, territorial, tribal, and local health departments.
References
- Mead PS, Slutsker L, Dietz V, et al. Food-related illness and death in the United States. Emerg Inf Dis 1999;5:607--25.
- Painter JA, Ayers T, Woodruff R, et al. Recipes for foodborne outbreaks: a scheme for categorizing and grouping implicated foods. Foodborne Pathog Dis 2009;6:1259--64.
- CDC. Norovirus activity---United States, 2006--2007. MMWR 2007;56:842--6.
- CDC. Surveillance for foodborne disease outbreaks---United States, 2006. MMWR 2009;58:609--15.
- Siebenga JJ, Vennema H, Zheng DP, et al. Norovirus illness is a global problem: emergence and spread of norovirus GII.4 variants, 2001--2007. J Infect Dis 2009;200:802--12.
- Korsager B, Hede S, Boggild H, Bottiger BE, Molbak K. Two outbreaks of norovirus infections associated with the consumption of imported frozen raspberries, Denmark, May--June 2005. Euro Surveill 2005;10:E050623.1.
- Dowell SF, Groves C, Kirkland KB, et al. A multistate outbreak of oyster-associated gastroenteritis: implications for interstate tracing of contaminated shellfish. J Infect Dis 1995;171:1497--503.
- Malek M, Barzilay E, Kramer A, et al. Outbreak of norovirus infection among river rafters associated with packaged delicatessen meat, Grand Canyon, 2005. Clin Infect Dis 2009;48:31--7.
- Food and Drug Administration. Real progress in food code adoptions. Silver Spring, MD: Food and Drug Administration; 2010. Available at http://www.fda.gov/food/foodsafety/retailfoodprotection/federalstatecooperativeprograms/ucm108156.htm#adopt. Accessed August 5, 2010.
- CDC. FoodNet 2007 surveillance report. Atlanta, GA: US Department of Health and Human Services, CDC; 2009. Available at http://www.cdc.gov/foodnet/annual/2007/2007_annual_report_508.pdf. Accessed May 5, 2010.
* The reporting form is available via the National Outbreak Reporting System at http://www.cdc.gov/outbreaknet/nors; the toolkit is available at http://www.cdc.gov/outbreaknet/references_resources.
† US Census Bureau. Population, population change and estimated components of population change: April 1, 2000 to July 1, 2008. Available at http://www.census.gov/popest/datasets.html.
§ Available at http://www.cdc.gov/outbreaknet/references_resources/guide_confirming_diagnosis.html.
¶ Additional data on foodborne disease outbreaks and illnesses for the 17 commodity categories can be found at http://www.cdc.gov/outbreaknet/surveillance_data.html.
** The 2009 Food Code and earlier versions are available at http://www.fda.gov/food/foodsafety/retailfoodprotection/foodcode/default.htm.
What is already known on this topic?
Surveillance for foodborne disease outbreaks can identify opportunities to prevent and control foodborne diseases, which cause millions of illnesses in the United States each year.
What is added by this report?
Among the 1,097 foodborne disease outbreaks reported in 2007, most of the single, laboratory-confirmed, agents of outbreak-associated illnesses (12,767) were norovirus (47%) and Salmonella (27%). Among outbreaks in which a pathogen and a single-commodity food vehicle were identified, most were attributed to norovirus in leafy vegetables, Escherichia coli O157 in beef, or Clostridium perfringens in poultry.
What are the implications for public health practice?
Timely investigation and reporting of foodborne outbreaks can provide public health, regulatory, and agricultural professionals with information to target control and prevention strategies as well as to promote good food-handling practices among food employees and the public.
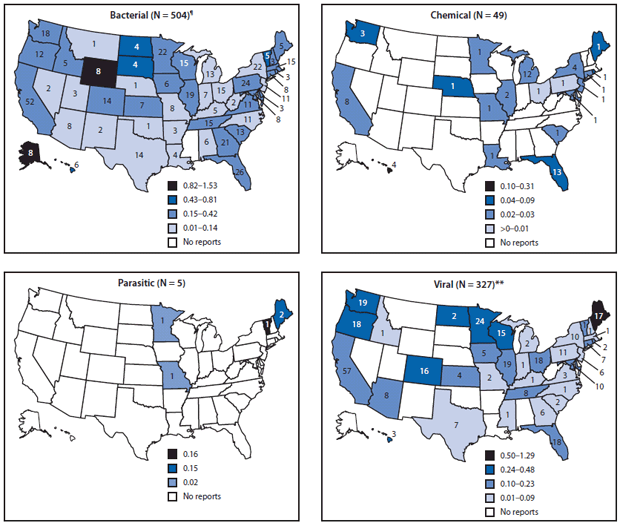
* Cutpoints for outbreak rate categories determined using Jenks Natural Breaks Optimization in ArcGIS.
† Number of reported outbreaks in each state.
§ Analysis restricted to outbreaks attributed to a single confirmed or suspected etiology. Note that legend differs for each etiology.
¶ Includes 17 multistate outbreaks, which are assigned as an outbreak to each state involved. An outbreak in Puerto Rico is not shown.
** Includes one multistate outbreak, which is assigned as an outbreak to each state involved.
Alternate Text: The figure above shows the rate of reported foodborne disease outbreaks per 100,000 standard population and number of outbreaks, by state and major etiology group in the United States in 2007. Public health officials from 48 states, Puerto Rico, and the District of Columbia reported 1,097 foodborne disease outbreaks; multistate outbreaks involving two additional states (Montana and Nevada) were reported indirectly.
|
TABLE 2. Number of reported foodborne disease outbreaks and outbreak-associated illnesses, by etiology* and food vehicle attribution --- United States, 2007.† |
||||||||
|---|---|---|---|---|---|---|---|---|
|
Etiology |
Outbreaks (illnesses) |
Total outbreaks (illnesses) |
||||||
|
Attributed to a single commodity§ |
Attributed to food containing at least two commodities |
Attributed to unknown commodity |
||||||
|
Bacterial |
|
|||||||
|
Salmonella¶ |
32 |
(816) |
39 |
(1,939) |
71 |
(760) |
142 |
(3,515) |
|
Clostridium perfringens |
21 |
(652) |
18 |
(535) |
6 |
(419) |
45 |
(1,606) |
|
Staphylococcus enterotoxin** |
7 |
(186) |
7 |
(59) |
7 |
(41) |
21 |
(286) |
|
Escherichia coli, Shiga toxin-producing (STEC)†† |
18 |
(341) |
3 |
(30) |
21 |
(232) |
42 |
(603) |
|
Campylobacter§§ |
15 |
(252) |
1 |
(48) |
11 |
(72) |
27 |
(372) |
|
Bacillus cereus |
4 |
(51) |
9 |
(75) |
6 |
(38) |
19 |
(164) |
|
Shigella¶¶ |
3 |
(132) |
0 |
(0) |
8 |
(223) |
11 |
(355) |
|
Vibrio parahaemolyticus |
1 |
(5) |
0 |
(0) |
0 |
(0) |
1 |
(5) |
|
Listeria*** |
1 |
(5) |
0 |
(0) |
0 |
(0) |
1 |
(5) |
|
Clostridium botulinum |
1 |
(4) |
2 |
(10) |
1 |
(2) |
4 |
(16) |
|
Brucella spp |
1 |
(3) |
0 |
(0) |
0 |
(0) |
1 |
(3) |
|
Escherichia coli, enterotoxigenic |
0 |
(0) |
1 |
(76) |
1 |
(66) |
2 |
(142) |
|
Yersinia enterocolitica |
0 |
(0) |
0 |
(0) |
0 |
(0) |
0 |
(0) |
|
Other bacterial |
1 |
(32) |
1 |
(3) |
2 |
(8) |
4 |
(43) |
|
Total |
105 |
(2,479) |
81 |
(2,775) |
134 |
(1,861) |
320 |
(7,115) |
|
Chemical |
||||||||
|
Scombroid toxin/Histamine |
19 |
(72) |
1 |
(2) |
0 |
(0) |
20 |
(74) |
|
Ciguatoxin |
13 |
(81) |
1 |
(3) |
0 |
(0) |
14 |
(84) |
|
Mycotoxins |
3 |
(10) |
0 |
(0) |
0 |
(0) |
3 |
(10) |
|
Neurotoxic shellfish poison |
1 |
(3) |
0 |
(0) |
0 |
(0) |
1 |
(3) |
|
Puffer fish tetrodotoxin |
0 |
(0) |
1 |
(2) |
0 |
(0) |
1 |
(2) |
|
Heavy metals |
0 |
(0) |
0 |
(0) |
1 |
(3) |
1 |
(3) |
|
Paralytic shellfish poison |
1 |
(4) |
0 |
(0) |
0 |
(0) |
1 |
(4) |
|
Other natural toxins |
2 |
(6) |
0 |
(0) |
1 |
(6) |
3 |
(12) |
|
Other chemical |
2 |
(4) |
0 |
(0) |
3 |
(14) |
5 |
(18) |
|
Total |
41 |
(180) |
3 |
(7) |
5 |
(23) |
49 |
(210) |
|
Parasitic |
||||||||
|
Cryptosporidium |
0 |
(0) |
1 |
(5) |
2 |
(9) |
3 |
(14) |
|
Cyclospora |
0 |
(0) |
0 |
(0) |
0 |
(0) |
0 |
(0) |
|
Giardia |
0 |
(0) |
1 |
(15) |
1 |
(36) |
2 |
(51) |
|
Trichinella |
0 |
(0) |
0 |
(0) |
0 |
(0) |
0 |
(0) |
|
Other parasite |
0 |
(0) |
0 |
(0) |
0 |
(0) |
0 |
(0) |
|
Total |
0 |
(0) |
2 |
(20) |
3 |
(45) |
5 |
(65) |
|
Viral |
||||||||
|
Norovirus |
39 |
(800) |
69 |
(1,819) |
209 |
(5,405) |
317 |
(8,024) |
|
Hepatitis A |
1 |
(3) |
1 |
(15) |
2 |
(10) |
4 |
(28) |
|
Rotavirus |
0 |
(0) |
0 |
(0) |
2 |
(18) |
2 |
(18) |
|
Other viral |
0 |
(0) |
0 |
(0) |
1 |
(17) |
1 |
(17) |
|
Total |
40 |
(803) |
70 |
(1,834) |
214 |
(5,450) |
324 |
(8,087) |
|
Single etiology (subtotal) |
186 |
(3,462) |
156 |
(4,636) |
356 |
(7,379) |
698 |
(15,477) |
|
Unknown etiology††† |
40 |
(531) |
66 |
(687) |
257 |
(3,904) |
363 |
(5,122) |
|
Multiple etiologies |
9 |
(126) |
13 |
(376) |
14 |
(143) |
36 |
(645) |
|
Total |
235 |
(4,119) |
235 |
(5,699) |
627 |
(11,426) |
1,097 |
(21,244) |
|
* If all reported etiologies were laboratory-confirmed, the outbreak was considered to have a "confirmed etiology." If at least one etiology was not laboratory-confirmed, but an etiology was reported based on clinical or epidemiologic features, the outbreak was considered to have a "suspected etiology." † As of May 3, 2010. § Data on foodborne disease outbreaks and illnesses for each of the 17 commodity categories is available at http://www.cdc.gov/outbreaknet/surveillance_data.html. ¶ Salmonella serotypes accounting for more than five outbreaks reported include Enteriditis (30 outbreaks), Typhimurium (20), Newport (17), and Heidelberg (nine), and Montevideo (nine). ** Staphylococcus aureus (11 confirmed outbreaks, nine suspected outbreaks) and Staphylococcus unknown (one suspected outbreak). †† STEC O157:H7 (36 confirmed outbreaks, two suspected outbreaks), STEC O157:NM(H-) (three confirmed outbreaks), and STEC O111 (one confirmed outbreak). §§ Campylobacter jejuni (14 confirmed outbreaks, three suspected outbreaks) and Campylobacter unknown (seven confirmed outbreaks, three suspected outbreaks). ¶¶ Shigella sonnei (nine confirmed outbreaks, one suspected outbreak) and Shigella unknown (one confirmed outbreak). *** Listeria monocytogenes (one confirmed outbreak). ††† An etiologic agent was not confirmed or suspected based on clinical, laboratory, or epidemiologic information. |
||||||||
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


