Work-related Tuberculosis

Photo by Getty Images
Spread of tuberculosis (TB) is a risk in healthcare and other congregate settings where people share the same space for extended time. Examples of congregate settings where TB spread occurs include:
- Prisons
- Jails
- Homeless shelters
- Social assistance shelters
- Emergency shelters
This disease often spreads when patients, prisoners, or shelter clients have unrecognized TB. It can also spread when people with active disease receive ineffective or incomplete treatment.
TB is a contagious and potentially life-threatening infectious disease caused by a bacteria called Mycobacterium tuberculosis. The bacteria spread from person to person through the air. People with symptoms have active TB infection and can spread the disease. The risk of developing active TB disease is greatest in the first few years after infection, but some risk remains throughout life.
People with active TB of the lungs or larynx release the bacteria into the surrounding area when they:
- Cough
- Sneeze
- Talk
- Expel droplets in the air in other ways
These droplets can dry into tiny particles called droplet nuclei. They remain suspended in air for long periods of time. Other people can breathe the infectious particles into their lungs. Becoming infected with TB typically requires an extended amount of time sharing a space with a person who has active TB. However, in rare cases the infection has been documented after short exposures to persons with active TB.
People who have been infected but do not have symptoms have latent TB infection and are not contagious. Once infected, most people’s immune systems can control the infection. However, they are not able to eliminate it without taking anti-TB drugs. Without treatment, people infected with latent TB can develop active TB and become contagious.
TB is preventable and treatable in most cases. It can usually be cured by available anti-TB drugs. Infection control practices can help reduce the spread of TB. Treatment for latent TB infection can prevent others from developing active TB. Even persons with drug-resistant strains can often recover using alternative regimens of medications.

Photo by Getty Images
Respiratory Protection
A TB infection control program should be based on the following three levels of a hierarchy of controls:
- Administrative Controls – Change the way people work
- Engineering Controls – Isolate people from the hazard
- Personal Protective Equipment (respiratory protection) – Further reduces risk of exposure
The minimum level of respiratory protection acceptable for TB is a filtering face piece respirator selected from those approved by NIOSH under Title 42 CFR, Part 84.
The following references provide useful information on establishing a respiratory protection program and choosing appropriate respirators.
Respirator Information
NIOSH Topic Page about respirators, including news, user notices, and respirator selection and maintenance and more.
Respirators: Your TB Defense
Streaming videos about respiratory protection against TB.
NIOSH-Approved Disposable Particulate Respirators (Filtering Facepieces)
A listing of NIOSH-approved disposable particulate respirators that health care workers can use to help protect themselves from diseases potentially spread through the air, such as SARS or Tuberculosis.
TB Respiratory Protection Program in Health Care Facilities – Administrator’s Guide
DHHS (NIOSH) Publication No. 99-143 (1999)
A manual designed to serve as a practical guide for those individuals responsible for initiating and running a TB respiratory protection program in health care facilities.
Protect Yourself Against Tuberculosis – A Respiratory Protection Guide for Health Care Workers
DHHS (NIOSH) Publication No. 96-102 (1995)
A booklet written to answer questions about respirator use in the health care industry. Serves as a quick reference for health care workers employed in a variety of settings and with varied educational backgrounds.

Photo by Getty Images
Training
TB training for clinicians and health care workers includes:
CDC TB 101 for Health Care Workers
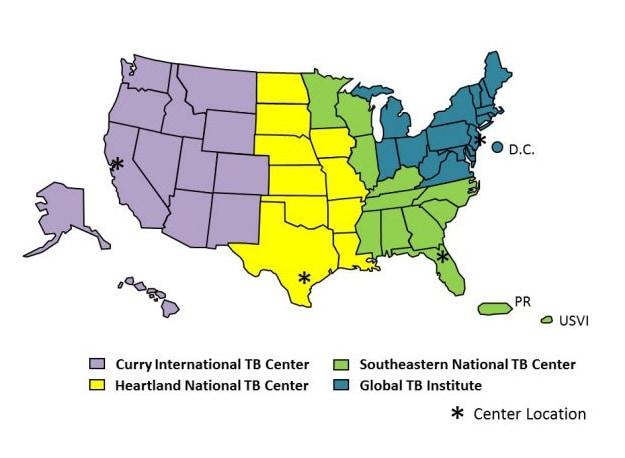
Regional Tuberculosis Training and Medical Consultation Centers (RTMCC)
Curry International Tuberculosis Center
The Curry International Tuberculosis Center is a RTMCC serving 13 states in the western United States, including Alaska, Hawaii, and U.S. Pacific Island Territories.
Global Tuberculosis Center at Rutgers, the State University of New Jersey
The New Jersey Medical School National Tuberculosis Center at the University of Medicine and Dentistry of New Jersey (UMDNJ) was established in January 1993 in response to the resurgence of Tuberculosis in the United States. It is now the Northeastern RTMCC serving 16 northeastern states and Washington, D.C.
Heartland National Tuberculosis Center
The Heartland National TB Center a RTMCC serving 10 states in the south-central United States. The vision of Heartland National TB Center is to provide excellence, expertise, and innovation in training, medical consultation, and product development to reduce the impact of tuberculosis.
Southeastern National Tuberculosis Center
The Southeastern National Tuberculosis Center (SNTC) is a RTMCC serving 11 states in the southeastern and central United States, Puerto Rico and the U.S. Virgin Islands. The SNTC supports the education and training missions of TB programs throughout our region and provides a source of expert medical consultation for healthcare providers caring for TB patients.