Injuries from Methamphetamine-Related Chemical Incidents — Five States, 2001–2012
, MD, PhD1; , MS1; , MS1, , PhD2
Methamphetamine (meth), a highly addictive drug, can be illegally manufactured using easily acquired chemicals; meth production can cause fires, explosions, injuries, and environmental contamination (1). To analyze injury incidence and trends, data on 1,325 meth-related chemical incidents reported to the Agency for Toxic Substances and Disease Registry's (ATSDR) Hazardous Substances Emergency Events Surveillance (HSEES) system and National Toxic Substance Incidents Program (NTSIP) by the five participating states (Louisiana, Oregon, Utah, New York, and Wisconsin) with complete information during 2001–2012 were examined. The findings suggested that meth-related chemical incidents increased with the drug's popularity (2001–2004), declined with legislation limiting access to precursor chemicals (2005–2007), and increased again as drug makers circumvented precursor restrictions (2008–2012). Seven percent of meth-related chemical incidents resulted in injuries to 162 persons, mostly members of the general public (97 persons, including 26 children) and law enforcement officials (42). Recent trends suggest a need for efforts to protect the general public, particularly children and law enforcement officials. Because individual state legislative actions can result in increased illegal meth production in neighboring states, a regional approach to prevention is recommended.
ATSDR supports state health departments to collect and analyze data about the public health impact of acute toxic substance releases. Data were analyzed from five states that collected information on meth-related chemical incidents for ATSDR's HSEES system during 2001–2009 and for NTSIP (the successor to HSEES), during 2010–2012. All chemical incidents possibly related to meth production, including ammonia releases associated with thefts for presumed meth production, were reviewed and confirmed. Injured persons were classified as responders (firefighters, law enforcement officials, or unspecified responders), employees, and members of the public, who could include meth producers (i.e., "cooks") or other household residents, including children. Joinpoint analysis was used to examine trends in meth-related chemical incidents.* Data on injured persons including their age group, injury severity, injury type, and population category were tabulated and analyzed by time interval.
During 2001–2012, a total of 1,325 meth-related chemical incidents were reported in the five states. Among all chemical incidents, the percentage that were classified as meth-related, by year, were plotted, and joinpoint analysis verified three trend periods: 2001–2004, 2005–2007, and 2008–2012. This percentage increased each year from 2001 through 2004, then decreased each year through 2007, and increased again through 2012 (Figure).
In 87 (7%) of the meth-related chemical incidents, 162 persons were injured, including at least 26 (16%) children (Table 1). Among those injured, 136 (84%) were treated at a hospital, including 19 (73%) children; 36 (22%) injured persons, including 19 (73%) children, required hospital admission. The percentage of injured persons who went to a hospital increased over time, from 75% (2001–2004), to 86% (2005–2007), to 90% (2008–2012). Two adults died: one, who might have been a meth cook, was found dead in a meth laboratory; the second was a law enforcement official.
The percentage of meth-related chemical incidents with injured persons increased from <5% during 2001–2004 and 2005–2007 to 10% during 2008–2012 (Table 1). The most commonly reported injuries were respiratory irritation (44%), chemical and thermal burns (27%), and eye irritation (22%) (Table 1). Chemical and thermal burns significantly increased, from 7% during 2005–2007 to 44% during 2008–2012 (p<0.001), temporally associated with new, hazardous production methods. During the same time, skin irritation injuries decreased from 20% to 2% (p = 0.004), eye symptoms decreased from 18% to 11%, and respiratory symptoms decreased from 57% to 31% (p>0.05).
Most injuries were to members of the general public (97) and law enforcement officials (42), followed by employees working in areas where meth contamination occurs, including hotels and motels, abandoned buildings, and treatment centers (14); and firefighters (7) (Table 1). The most commonly reported injuries among the general public were burns (43%) and respiratory irritation (37%); among injured law enforcement officials, respiratory irritation (64%), and eye irritation (38%) were most frequently reported (Table 2). Only two injured law enforcement officials used personal protective equipment (PPE). All seven injured firefighters used protective clothing with respiratory protection; one had respiratory irritation, but more symptoms consistent with inadequate skin protection (skin irritation) and wearing heavy, hot gear (headache and gastrointestinal) were observed. Among the 14 injured employees, nine reported headache, seven respiratory irritation, and seven eye irritation.
Discussion
In September 2006, federal legislation restricting the retail sale of the common meth precursor drugs ephedrine and pseudoephedrine was enacted (2). Many states independently implemented this act in 2005, and the number of meth-related chemical incidents in the HSEES database subsequently declined. However, this trend was reversed in 2008 when meth cooks learned to circumvent the laws and obtain the restricted precursor drugs by purchasing permitted quantities from multiple locations, often using false identification and the assistance of other persons (3). Also around 2008, the "shake-and-bake" meth-making method became popular (4). This method involves shaking smaller amounts of precursor chemicals in a 2-L plastic bottle, which frequently bursts, causing burns and environmental contamination (3,4). Burn injuries increased during this time, particularly to members of the public, who might have been meth cooks or household residents.
"Prescription-only" laws for ephedrine and pseudoephedrine were enacted in Oregon (2006) and Mississippi (2010). Since the law went into effect in Oregon, fewer meth laboratories have been seized, and Oregon has reported fewer meth-related chemical incidents. Meth-related chemical incident data are not available for Mississippi; however, since Mississippi's prescription law went into effect, fewer meth laboratories were seized in that state (3), but meth-related chemical incidents increased in neighboring Louisiana (5). To most effectively reduce meth production, a regional, rather than state-by-state approach to outreach has been proposed by the Office of National Drug Control Policy, including implementing stricter laws limiting meth precursors, using electronic monitoring systems to track precursor purchasers, and developing and maintaining a database including information about offenders (6).
Workers, including responders, should be trained and prepared to recognize the different potential hazards of their occupations, and to know control measures to prevent injury such as avoidance, proper PPE selection and proper PPE use. Law enforcement personnel might encounter dangerous meth situations while responding to other calls, in conducting public safety assignments in response to meth incidents, and during meth laboratory seizures (1). Although the number and severity of law enforcement personnel injuries was slightly reduced, which might be related to targeted outreach, this group remains at high risk and needs training to recognize these risks and use appropriate PPE and procedures to avoid exposure and injury (7). The use of PPE by firefighters appears to afford respiratory protection; however, their gear is not designed to protect their skin from chemicals and can be heavy and hot during response. If possible, they should have physical fitness qualifications and physical monitoring for PPE usage.† Other workers were injured in locations where meth laboratories or contaminated persons are often encountered; therefore, employees working as cleanup contractors, or in housekeeping, patient intake, and other high-risk occupations should be alerted to the dangers.
Children who are present during drug production face many hazards in addition to threats to their health and safety (8,9). Several states, including Georgia, have enacted laws to protect children from meth-related injuries. In 2004, Georgia's governor used ATSDR data to support passage of a law that provides for serious penalties to meth producers if a child is present or is seriously injured during meth production (8).§ As part of the president's 2010 National Drug Control Strategy, the Department of Justice established the Federal Interagency Drug Endangered Children Task Force to provide guidance to professionals to help identify, respond to, and serve children endangered by drugs.¶
With the increase in residential meth laboratories comes an increase in contaminated housing. The Drug Enforcement Agency maintains the National Clandestine Laboratory Register, which lists meth laboratories or illegal dump sites reported by law enforcement; some states maintain independent registries. These registries might help prevent inadvertent occupation of nonremediated contaminated housing. The agency's Clandestine Drug Laboratory Cleanup Program assists states with the removal and disposal of seized drug-making chemicals and equipment, and the U.S. Environmental Protection Agency provides national remediation guidelines and remediation support (9). In February 2011, state assistance was temporarily discontinued. During the unfunded period, according to an Associated Press report, local governments did not seize at least one third of known meth laboratories because they could not afford the clean-up cost, highlighting the importance of these resources for the seizure and effective clean-up of meth laboratories.**
The findings in this report are subject to at least three limitations. First, all meth-related incidents for the five states in the database might not have been captured because of the queries used. NTSIP does not include meth incidents in homes unless there is a public health action, such as evacuation. In addition, because of pending legal actions, data on meth-chemical incidents are often difficult to obtain. Second, because states rely on relationships with law enforcement agencies and on scanning media reports, the quality of meth-related chemical incident data differs among states. Finally, trends from the five states cannot be generalized to the entire United States.
Implementation of federal and individual state legislative efforts to curb meth production has sometimes resulted in unintended consequences, such as shifting the problem to other states and circumvention of laws limiting precursor availability. Public health outreach aimed at protecting the general public (including children) and law enforcement officials, the groups most often injured in meth incidents is urgently needed. Possible actions include additional legislative restrictions, continued support for the identification and remediation of contaminated housing, professional responder training, and identifying children at risk for exposure.
1Division of Toxicology and Human Health Sciences, Agency for Toxic Substances and Disease Registry; 2Division of Environmental Hazards and Health Effects, National Center for Environmental Health, CDC.
Corresponding author: Natalia Melnikova, nmelnikova@cdc.gov, 770-488-3697.
References
- Melnikova N, Welles WL, Wilburn RE, Rice N, Wu J, Stanbury M. Hazards of illicit methamphetamine production and efforts at reduction: data from the hazardous substances emergency events surveillance system. Public Health Rep 2011;126(Suppl 1):116–23.
- The combat methamphetamine epidemic act of 2005. Pub.L.No.109–177, Sec.701–56, 120 Stat.192, 256–77. March 9, 2006.
- Office of National Drug Control Policy, Executive Office of the President. Fact sheet: methamphetamine trends in the United States. July 2010. Available at http://www.whitehouse.gov/sites/default/files/ondcp/Fact_Sheets/pseudoephedrine_fact_sheet_7-16-10_0.pdf.
- Burke BA, Lewis RW 2nd, Latenser BA, et al. Methamphetamine-related burns in the cornbelt. J Burn Care Res 2008;29:574–9.
- Trachtman WC, Xiaoping N, Syed AA, Koehler AN. Considerable increase in methamphetamine events Louisiana, 2011. Louisiana Morbidity Report 2012;23:2–6. Available at http://new.dhh.louisiana.gov/assets/oph/Center-PHCH/Center-CH/infectious-epi/LMR/2011-2020/2012/marapr12.pdf.
- Office of National Drug Control Policy, Executive Office of the President. Controlling precursor chemicals. Available at http://www.whitehouse.gov/ondcp/precursor-chemicals.
- CDC. Public health consequences among first responders to emergency events associated with illicit methamphetamine laboratories—selected states, 1996–1999. MMWR Morb Mortal Wkly Rep 2000;49:1021–4.
- Horton DK, Berkowitz Z, Kaye WE. The acute health consequences to children exposed to hazardous substances used in illicit methamphetamine production, 1996 to 2001. J Child Health 2003;1:99–108.
- US Environmental Protection Agency. Voluntary guidelines for methamphetamine laboratory cleanup. Revised edition: March 2013. Available at http://www2.epa.gov/sites/production/files/documents/meth_lab_guidelines.pdf.
* Additional information available at http://surveillance.cancer.gov/joinpoint/.
† Additional information available at http://www.cdc.gov/niosh/fire/reports/face201218.html.
§ Georgia code § 16-5-73(b).
¶ Additional information available at http://www.whitehouse.gov/ondcp/dec-info.
** Available at http://news.yahoo.com/ap-exclusive-national-meth-lab-busts-2011-185113059.html.
Summary
What is already known on this topic?
Illegal methamphetamine production results in fires, explosions, spills, or air releases of hazardous chemicals (meth-chemical incidents), placing the meth producer and others nearby, including children, workers, and responders, at risk for injury or death and causing environmental contamination.
What is added by this report?
Data from five states suggest that, beginning in 2005, when state and federal legislative efforts to restrict meth precursors were enacted, meth-related chemical incidents temporarily declined in those states. However, in 2008, as meth producers learned to circumvent laws and obtain restricted precursor drugs, and introduced the hazardous "shake-and-bake" meth-making method, such incidents began to rise, as did the percentage of events with injuries, particularly burns. The general public, including many children, and law enforcement officials are most often injured. Prescription-only precursor laws have been effective in states that have implemented them, but also have had unintended consequences on neighboring states.
What are the implications for public health practice?
Additional measures should be taken to protect the public, particularly children, from meth-related chemical exposures. Law enforcement officials might need increased awareness and training. It is also important to consider regional approaches because actions in one state might result in increased meth production in a neighboring state.
FIGURE. Joinpoint analysis of percentage of chemical incidents that were methamphetamine-related — Hazardous Substances Emergency Events Surveillance System and National Toxic Substance Incidents Program, five states, 2001–2012
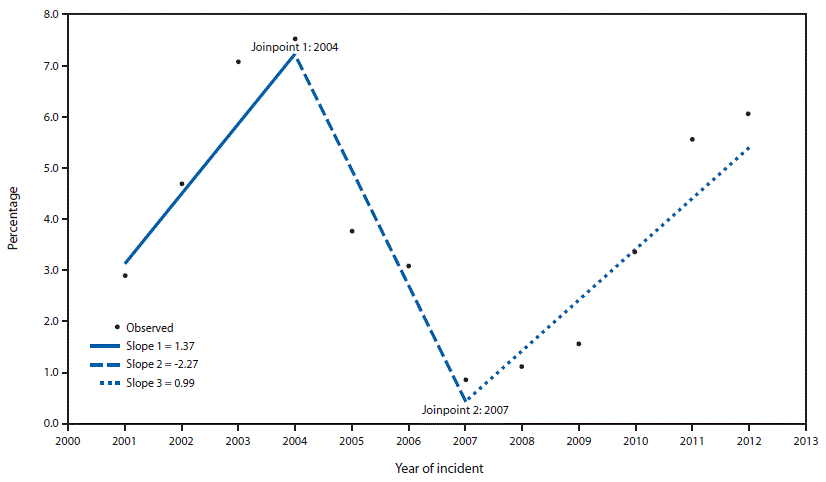
Alternate text:The figure above is a graph of a joinpoint analysis showing trends in reported chemical incidents that were methamphetamine-related in five U.S. states during 2001–2012.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


