Importation and Domestic Transmission of Shigella sonnei Resistant to Ciprofloxacin — United States, May 2014–February 2015
, MD1, , MPH1, , MD2, , MPH3, , MPH4, 4, , MPH5, , MPH2, , MPH2,1, 1, , MD6 (Author affiliations at end of text)
In December 2014, PulseNet, the national molecular subtyping network for foodborne disease, detected a multistate cluster of Shigella sonnei infections with an uncommon pulsed-field gel electrophoresis (PFGE) pattern. CDC's National Antimicrobial Resistance Monitoring System (NARMS) laboratory determined that isolates from this cluster were resistant to ciprofloxacin, the antimicrobial medication recommended to treat adults with shigellosis. To understand the scope of the outbreak and to try to identify its source, CDC and state and local health departments conducted epidemiologic and laboratory investigations. During May 2014–February 2015, PulseNet identified 157 cases in 32 states and Puerto Rico; approximately half were associated with international travel. Nine of the cases identified by PulseNet, and another 86 cases without PFGE data, were part of a related outbreak of ciprofloxacin-resistant shigellosis in San Francisco, California. Of 126 total isolates with antimicrobial susceptibility information, 109 (87%) were nonsusceptible to ciprofloxacin (108 were resistant, and one had intermediate susceptibility). Travelers need to be aware of the risks of acquiring multidrug-resistant pathogens, carefully wash their hands, and adhere to food and water precautions during international travel. Clinicians should request stool cultures and antimicrobial susceptibilities when they suspect shigellosis, and counsel shigellosis patients to follow meticulous hygiene regimens while ill.
Shigella causes an estimated 500,000 cases of diarrhea in the United States annually (1) and is transmitted easily from person to person and through contaminated food and recreational water. Outbreaks of shigellosis frequently are large and protracted. Although diarrhea caused by S. sonnei typically resolves without treatment, patients with mild illness often are treated with antimicrobial medications because they can reduce the duration of symptoms and shedding of shigellae in feces (2). However, resistance to the oral antimicrobial medications ampicillin and trimethoprim/sulfamethoxazole is common among shigellae in the United States, and resistance to fluorquinolones is increasing among shigellae globally (3). Because only about 2% of shigellae isolated in the United States are resistant to fluoroquinolones (4), ciprofloxacin is the first-line treatment for adults with shigellosis and is recommended as an empiric treatment for adult international travelers with diarrhea (5).
Between May 24, 2014 and February 28, 2015, PulseNet detected 157 cases of illness caused by S. sonnei with closely related pulsed-field gel electrophoresis (PFGE) patterns in 32 U.S. states and Puerto Rico. Most cases were reported in Massachusetts (45 cases), California (25) and Pennsylvania (18). In addition, public health officials in the San Francisco Department of Public Health (SFDPH) identified an outbreak of 95 cases of ciprofloxacin-resistant shigellosis, nine of which were tested using PFGE and have been included in the PulseNet cluster, for a total of 243 cases (Figure). The San Francisco outbreak cases are included in the antimicrobial susceptibility summary but are excluded from other analyses.
State and federal public health officials reported ciprofloxacin nonsusceptibility in 109 (87%) of 126 isolates tested (108 isolates were resistant and 1 had intermediate susceptibility). Of the 126 isolates, NARMS tested 19. All were resistant to nalidixic acid, and six (32%) were resistant to ciprofloxacin; isolates also exhibited resistance to ampicillin (5%), streptomycin (84%), sulfisoxazole (84%), tetracycline (87%), and trimethoprim/sulfamethoxazole (84%). One isolate displayed an azithromycin minimum inhibitory concentration of >256 µg/ml and harbored macrolide resistance genes mphA and ermB.
Median age of the patients was 34 years (interquartile range = 20–51 years). Among the patients, 48% (74 of 153) were female. Among 41 patients with such information, median duration of illness was 7 days (interquartile range = 6–12 days). Nineteen (22%) of 88 patients with such information were hospitalized. Treatment information was not available for most patients.
Forty (53%) of 75 patients with such information had traveled internationally during their incubation period; destinations included Hispaniola (the Dominican Republic, 22 cases, and Haiti, four); India (eight); Morocco (three); and other destinations in Asia and Europe. No common airline or airport exposures were identified. Most travelers to the Dominican Republic stayed at resorts in Punta Cana; however, no common hotel, resort, restaurant, or event was reported. NARMS detected ciprofloxacin resistance in isolates obtained from travelers to the Dominican Republic (one of five isolates tested) and India (one of one isolate tested), and among nontravelers (four of seven isolates tested).
Travel information was available for 23 of 37 children; 10 (43%) had recently traveled abroad. None of the five children who were enrolled in group child care settings had traveled internationally. One pediatric case occurred as part of a child care–associated outbreak of five culture-confirmed and 11 suspected cases of shigellosis. None of the other four isolates from this cluster were tested using PFGE; however, a single isolate was tested and found to be resistant to ciprofloxacin.
Twelve patients self-identified as men who have sex with men (MSM). Eleven (79%) of 14 men without recent international travel were MSM, compared with one of six men with recent international travel (Fisher's exact p = 0.02).
SFDPH identified 95 ciprofloxacin-resistant S. sonnei infections in residents of or travelers to San Francisco during November 1, 2014–January 15, 2015. Nine isolates underwent PFGE and yielded patterns that were indistinguishable from or closely related to others in the PulseNet cluster. Sixty-seven patients (53% of those with such information) were hospitalized. Seventy-four cases (47% of those with such information) occurred among persons who were homeless or living in single-room occupancy hotels. Although the investigation is ongoing, no point source or common exposures such as shelters, soup kitchens, or restaurants have been identified. No patients reported international travel.
Discussion
International travelers are at elevated risk for colonization with multidrug-resistant Enterobacteriaceae (6). This investigation suggests that ciprofloxacin-resistant S. sonnei is being repeatedly introduced into the United States by travelers from various countries and can lead to large outbreaks domestically. The result has been a greater proportion of Shigella infections in the United States that are resistant to ciprofloxacin than in the past (National Antimicrobial Resistance Monitoring System; Division of Foodborne, Waterborne and Environmental Diseases; National Center for Emerging and Zoonotic Infectious Diseases, CDC, unpublished data, 2015). Travelers should be encouraged to 1) observe food, water, and hand-hygiene precautions while traveling; 2) use over-the-counter medications like bismuth subsalicylate (e.g., Pepto-Bismol) or loperamide (e.g., Immodium) if they wish to treat mild or moderate travelers' diarrhea; 3) reserve antimicrobial medications for severe cases of travelers' diarrhea; 4) seek health care if they are experiencing diarrhea upon return to the United States or develop diarrhea shortly thereafter; and 5) remain vigilant regarding hygiene practices while ill. Additional studies are needed to clarify the roles of antimicrobial medications, antidiarrheal medications, and other factors in acquiring multidrug-resistant enteric pathogens during international travel.
Although this Shigella strain is strongly associated with international travel, it is now circulating domestically. If introduced to populations of homeless persons, MSM, or children in child care settings, Shigella can spread rapidly and cause large, protracted outbreaks, as has occurred in the homeless population in San Francisco.
Hygiene promotion and increased access to hygiene and sanitation infrastructure among vulnerable populations such as the homeless might help prevent transmission. MSM can reduce their risk for acquiring this and other Shigella strains by washing their hands meticulously and by preventing fecal-oral exposures during sex (7). Health care providers should culture the stool specimens of patients with symptoms consistent with shigellosis, reculture the stool of patients who fail to improve after antimicrobial therapy, and test bacterial pathogens for antimicrobial susceptibility. Reserving antimicrobial treatment for immunocompromised patients and patients with severe shigellosis and using antimicrobial susceptibility data strategically to guide therapy might help preserve the utility of such medications. Clinical guidelines for the testing and interpretation of azithromycin susceptibility among Shigella spp. are needed to improve detection and management of cases of azithromycin-nonsusceptible shigellosis.
Acknowledgments
Julian Grass, MPH, Davina Campbell, MS, Division of Foodborne, Waterborne and Environmental Diseases, National Center for Emerging, Zoonotic, and Infectious Diseases, CDC.
1Division of Foodborne, Waterborne and Environmental Diseases, National Center for Emerging, Zoonotic, and Infectious Diseases, CDC; 2San Francisco Department of Public Health; 3Philadelphia Department of Public Health Division of Disease Control; 4Massachusetts Department of Public Health; 5California Emerging Infections Program; 6California Department of Public Health (Corresponding author: Anna Bowen, abowen@cdc.gov, 404-639-4636)
References
- Scallan E, Hoekstra RM, Angulo FJ, et al. Foodborne illness acquired in the United States—major pathogens. Emerg Infect Dis 2011;17:7–15.
- Christopher PR, David KV, John SM, Sankarapandian V. Antibiotic therapy for Shigella dysentery. Cochrane Database Syst Rev 2009;(4):CD006784.
- Gu B, Cao Y, Pan S, et al. Comparison of the prevalence and changing resistance to nalidixic acid and ciprofloxacin of Shigella between Europe-America and Asia-Africa from 1998 to 2009. Int J Antimicrob Agents 2012;40:9–17.
- CDC. National Antimicrobial Resistance Monitoring System: enteric bacteria human isolates final report 2012. Atlanta, GA: US Department of Health and Human Sevices, CDC; 2014. Available at http://www.cdc.gov/narms/pdf/2012-annual-report-narms-508c.pdf.
- CDC. Health information for international travel 2014. New York, NY: Oxford University Press; 2014. Available at http://wwwnc.cdc.gov/travel/page/2014-yellow-book-about.
- Kantele A, Lääveri T, Mero S, et al. Antimicrobials increase travelers' risk of colonization by extended-spectrum beta-lactamase–producing Enterobacteriaceae. Clin Infect Dis 2015;60:837–46.
- Panel on Opportunistic Infections in HIV-Infected Adults and Adolescents. Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Atlanta, GA: US Department of Health and Human Services. Available at http://aidsinfo.nih.gov/contentfiles/lvguidelines/adult_oi.pdf.
What is already known on this topic?
Approximately 500,000 cases of shigellosis occur in the United States annually. High rates of resistance to oral antimicrobial medications complicate management of patients with shigellosis; however, ciprofloxacin has remained the recommended antimicrobial treatment for adults who acquire shigellosis within the United States or while traveling internationally.
What is added by this report?
During May 2014–February 2015, a cluster of 243 cases of shigellosis in 32 states and Puerto Rico was identified; 109 (87%) of 126 isolates tested were nonsusceptible to ciprofloxacin. Ninety-five cases were part of an outbreak of ciprofloxacin-resistant shigellosis associated with the homeless population in San Francisco, California; approximately half of the remaining cases were associated with international travel. Ciprofloxacin-resistant Shigella sonnei is being repeatedly introduced into the United States via travelers from various countries and is circulating domestically at rates that are higher than in the past.
What are the implications for public health practice?
International travelers should be aware of the risks for acquiring multidrug-resistant pathogens, wash their hands meticulously, adhere to food and water precautions, and try to reserve antimicrobial medications for severe cases of travelers' diarrhea. Clinicians should request stool specimen cultures and antimicrobial susceptibilities when they suspect shigellosis, carefully consider whether antibiotic treatment is necessary, and counsel shigellosis patients to follow meticulous hygiene regimens while ill. Hygiene promotion and increased access to hygiene and sanitation infrastructure might help prevent transmission among vulnerable populations.
FIGURE. Shigella sonnei infections (n = 239*) suspected resistant to ciprofloxacin, by isolation date and patient international travel history — United States, May 2014–February 2015
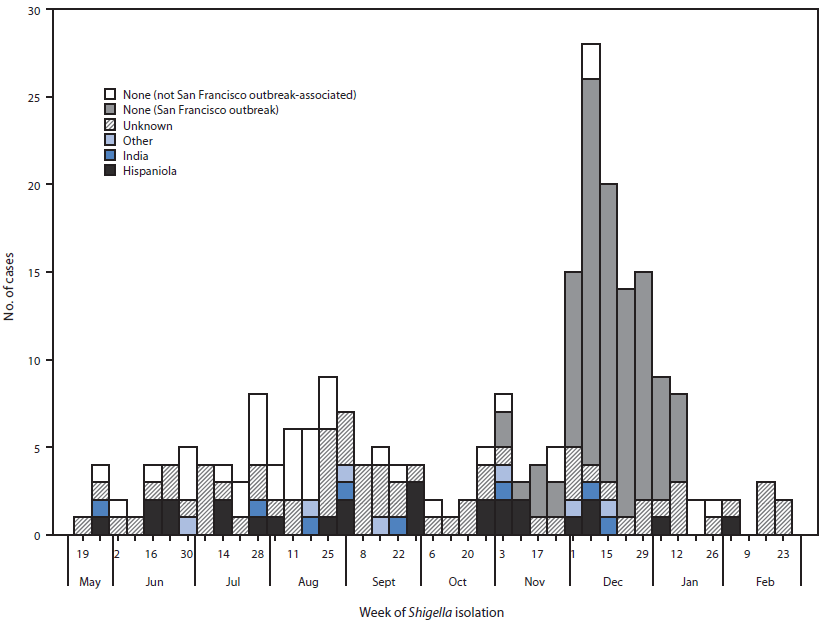
* Isolation date was not available for four isolates.
Alternate Text: The figure above is a histogram showing Shigella sonnei infections (n = 239) suspected resistant to ciprofloxacin, by isolation date and patient international travel history in the United States during May 2014-February 2015.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


