Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Quitting Smoking Among Adults --- United States, 2001--2010
Quitting smoking is beneficial to health at any age, and cigarette smokers who quit before age 35 years have mortality rates similar to those who never smoked (1,2). From 1965 to 2010, the prevalence of cigarette smoking among adults in the United States decreased from 42.4% to 19.3%, in part because of an increase in the number who quit smoking (3). Since 2002, the number of former U.S. smokers has exceeded the number of current smokers (4). Mass media campaigns, increases in the prices of tobacco products, and smoke-free policies have been shown to increase smoking cessation (5,6). In addition, brief cessation advice by health-care providers; individual, group, and telephone counseling; and cessation medications are effective cessation treatments (5). To determine the prevalence of 1) current interest in quitting smoking, 2) successful recent smoking cessation, 3) recent use of cessation treatments, and 4) trends in quit attempts over a 10-year period, CDC analyzed data from the 2001--2010 National Health Interview Surveys (NHIS). This report summarizes the results of that analysis, which found that, in 2010, 68.8% of adult smokers wanted to stop smoking, 52.4% had made a quit attempt in the past year, 6.2% had recently quit, 48.3% had been advised by a health professional to quit, and 31.7% had used counseling and/or medications when they tried to quit. The prevalence of quit attempts increased during 2001--2010 among smokers aged 25--64 years, but not among other age groups. Health-care providers should identify smokers and offer them brief cessation advice at each visit; counseling and medication should be offered to patients willing to make a quit attempt.
The 2010 NHIS, which used household-based sampling, interviewed 27,157 persons aged ≥18 years from the noninstitutionalized, U.S. civilian population; 190 persons were excluded from the analysis for this report because of unknown smoking status. The overall response rate for the 2010 NHIS adult core questionnaire, which included questions on cigarette smoking and cessation, was 60.8%; response rates for the 2001--2009 NHIS survey years have been reported previously.* To determine smoking status, respondents were asked, "Have you smoked at least 100 cigarettes in your entire life?" Those who answered "yes" were asked, "Do you now smoke cigarettes every day, some days, or not at all?" Current smokers were those who had smoked at least 100 cigarettes during their lifetime and, at the time of the interview, reported smoking every day or some days. Former smokers were those who reported smoking at least 100 cigarettes during their lifetime but currently did not smoke. Definitions for attempts to quit smoking and recent smoking cessation were consistent with Healthy People 2020 objectives.† Those attempting to quit included 1) current smokers who reported stopping smoking for >1 day during the 12 months before the interview because they were trying to quit smoking and 2) former smokers who had quit in the past year. Persons with recent smoking cessation included former smokers who quit in the past year and who had not smoked for ≥6 months before the interview; the denominator used for prevalences was current smokers who smoked for at least 2 years and former smokers who quit in the past year.
In 2010, NHIS respondents also were administered a supplemental questionnaire that focused on cancer and its risk factors and contained questions on interest in quitting smoking, receipt of a health professional's advice to quit, and use of cessation counseling and medication. Interest among current smokers in quitting smoking was determined by a "yes" response to the question, "Would you like to completely stop smoking cigarettes?" Current smokers and those who had quit in the past year were asked whether they had received medical advice to quit smoking (or quit using other tobacco products) if they had seen a health professional in the past year. Separate questions were asked to assess use of cessation counseling (i.e., one-on-one counseling; a stop smoking clinic, class, or support group; or a telephone help line or quitline) and cessation medications (i.e., nicotine patch, nicotine gum or lozenge, nicotine-containing nasal spray or inhaler, varenicline [U.S. trade name Chantix] or bupropion [including trade names Zyban and Wellbutrin]). Responses to these questions were used to assess treatments used in the past 12 months by current smokers who had tried to quit in the past year and treatments used when they stopped smoking by former smokers who had quit in the past 2 years. All data were adjusted for nonresponse and weighted to provide national estimates; 95% confidence intervals were calculated using statistical analysis software to account for the survey's multistage probability sample design. Logistic regression was used to analyze temporal changes in quit attempts by age group during 2001--2010. These 10-year linear trend analyses were constructed using 2001 prevalences as the baseline, adjusted for sex and race/ethnicity. The Wald test was used to determine statistical significance (defined as p<0.05). Data also were tested for quadratic trends, which indicated a statistically significant but nonlinear trend in the data over time.
Overall, 68.8% of current smokers indicated they wanted to stop smoking completely (Table 1). Interest in quitting smoking was lower among those aged ≥65 years (53.8%) than among those aged <65 years (70.2%). By race/ethnicity, interest in quitting was highest among non-Hispanic black smokers (75.6%), followed by non-Hispanic whites (69.1%), persons of other race/ethnicities (62.5%), and Hispanics (61.0%). A lower proportion of those with education ending at high school graduation reported an interest in quitting (65.9%) than those with some college (73.4%). In addition, those with Medicare (60.7%) or a military health plan (55.3%) were less likely to say they were interested in quitting than those with private insurance (70.4%) or Medicaid (71.2%).
Among current and former smokers, 52.4% had made a quit attempt for >1 day in the year before the interview (Table 1). Quit attempts decreased with increasing age; 62.4% of those aged 18--24 years reported a quit attempt, compared with 43.5% of those aged ≥65 years. Among smokers aged 45--64 years, a significant linear increase in quit attempts was observed from 2001 to 2010 (p<0.05 for linear trend) (Figure). During that period, the prevalence of quit attempts remained stable among smokers aged 18--24 years and ≥65 years. A quadratic relationship was observed for quit attempts among those aged 25--44 years, with the peak prevalence of attempts observed in 2010 (56.9%) (p<0.05 for quadratic trend). Quit attempts were more prevalent among non-Hispanic blacks (59.1%) than non-Hispanic whites (50.7%) (Table 1). Persons with ≤12 years of education (no high school diploma) (46.2%) or those with a high school diploma (46.9%) were less likely to make a quit attempt than those with some college (55.9%) or an undergraduate degree (56.0%).
The overall prevalence of recent cessation was 6.2% (Table 1). Cessation was more likely among non-Hispanic whites (6.0%) than among non-Hispanic blacks (3.3%). Cessation increased with level of education; 3.2% of those with ≤12 years of education quit smoking, compared with 11.4% of those with an undergraduate degree and 8.1% of those with an associate degree. Those with private health plans (7.8%) were more likely to have quit smoking than those with Medicaid (4.6%) or no health plan (3.6%).
Less than half of smokers (48.3%) who saw a health professional in the past year reported receiving advice to quit (Table 2). Among those who had visited a health-care provider, women (51.7%) and persons aged ≥65 years (57.1%) were more likely to have received cessation advice. Hispanic smokers were less likely (34.7%) to have received advice to quit than other racial/ethnic populations. Those without a health plan (35.3%) were least likely to have received cessation advice, whereas Medicare enrollees (59.0.%) were the most likely to receive advice.
Overall, among current smokers who tried to quit in the past year and former smokers who successfully quit in the past 2 years, use of counseling and/or cessation medications was 31.7% (Table 2); 4.3% had used both. Among those who had used counseling and/or cessation medications, 30.0% had used medications (nicotine patch: 14.6%, varenicline: 11.2%, nicotine gum or lozenge: 8.9%, bupropion: 3.2%, and nicotine spray/inhaler: 1.0%), and 5.9% had used counseling (telephone quitline: 3.1%, one-on-one counseling: 2.6%, and stop smoking clinic, class, or support group: 2.4%). Use of counseling and/or medication was higher among women (35.1%) than men (28.8%) and tended to increase with age (18--24 years: 15.8%, 25--44 years: 29.4%, 45--64 years: 42.3%, and ≥65 years: 35.9%). Non-Hispanic whites (36.1%) were more likely to use counseling and/or medications than non-Hispanic blacks (21.6%) or Hispanics (15.9%). Persons without a health plan (21.5%) were less likely to use counseling and/or medications than those with a health plan (35.6%).
Reported by
Ann Malarcher, PhD, Shanta Dube, PhD, Lauren Shaw, MS, Stephen Babb, MPH, Rachel Kaufmann, PhD, Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. Corresponding contributor: Ann Malarcher, amalarcher@cdc.gov, 770-488-8006.
Editorial Note
The findings in this report indicate that, in 2010, 68.8% of current cigarette smokers said they would like to completely stop smoking, and 52.4% had tried to quit smoking in the past year. However, 68.3% of the smokers who tried to quit did so without using evidence-based cessation counseling or medications, and only 48.3% of those who had visited a health-care provider in the past year reported receiving advice to quit smoking. Little overall change has been observed in these measures in the past decade (7,8). However, the prevalence of quit attempts did increase from 2001 to 2010 among those aged 25--64 years. The prevalence of receiving advice from a health professional to quit was lower in 2010 than in 2005, which might have resulted from a change in the NHIS cancer control supplement questionnaire (i.e., a preceding question about whether a health professional asked the participant about tobacco use was removed) (8). Advice from a health professional increases quit attempts and increases use of effective medications which can nearly double to triple rates of successful cessation (5).
Cigarette smoking and exposure to secondhand smoke result in approximately 443,000 premature deaths and $193 billion in health-care costs and productivity losses in the United States each year (9). Most smokers establish a regular pattern of smoking and find quitting difficult because they are addicted to nicotine (10). Tobacco dependence is a chronic condition, with many smokers making repeated quit attempts before they achieve long-term success (5). Health-care providers can draw on a number of evidence-based treatment options to assist smokers in quitting. The 2008 update to the Public Health Service Clinical Practice Guideline on Treating Tobacco Use and Dependence concludes that counseling and medication are each effective alone in increasing the prevalence of smoking cessation and are even more effective when used together (5). Individual, group, and telephone counseling are effective in helping smokers quit, and the seven Food and Drug Administration (FDA)--approved first-line cessation medications reliably increase long-term smoking abstinence rates (5). This analysis found that use of medications for cessation was approximately five times more common than use of counseling, which might be influenced, in part, by the widespread availability of over-the-counter cessation medications (e.g., nicotine patch, gum, and lozenge).
The findings in this analysis also observed that, whereas non-Hispanic blacks had higher prevalences of interest in quitting and past-year quit attempts than non-Hispanic whites, they had a lower prevalence of recent smoking cessation. Possible contributors to this disparity include non-Hispanic blacks' lower utilization of evidence-based cessation treatments and their high rates of menthol cigarette use (76.7%, compared with 23.6% for non-Hispanic whites [CDC, unpublished data, 2010]). The Tobacco Product Scientific Advisory Committee to FDA§ recently concluded that it is more likely than not that the availability of menthol cigarettes results in lower likelihood of smoking cessation success among blacks, compared with smoking nonmenthol cigarettes.
To help smokers and other tobacco users quit, all states now have a cessation quitline that can be accessed through a national toll-free number (1-800-QUIT NOW). Quitlines also can be a referral source for health-care providers who might not have the time or staff to provide all of the steps in the recommended "5A" cessation counseling model: ask about tobacco use, advise to quit, assess willingness to make a quit attempt, assist in quit attempt, and arrange follow-up (5). Quitlines are an effective cessation tool with diverse populations (5). Reports have shown that certain minority populations attempt to quit as often as or more often than white smokers, but use counseling and medications less often and have lower success rates (5). E-health, Internet, and text-messaging cessation interventions could offer additional potential channels for delivering cessation assistance, considering their accessibility, potential reach, and low cost (5,6). Although more research is needed to establish the effectiveness of these strategies, they likely would appeal especially to young adults, who in this report were the most likely of all age groups to make quit attempts but the least likely to use cessation counseling and medications.
Evidence-based cessation treatments, reducing client out-of-pocket costs for cessation treatments, and implementing provider-reminder systems to prompt health-care providers to deliver evidence-based treatments are effective in increasing cessation (5,6). Tobacco dependence treatments have been found to be both clinically effective and highly cost-effective (5). Health-care administrators and health plans can support these clinical interventions and increase successful cessation by providing comprehensive coverage for cessation treatments with no deductibles or copayments, integrating smoker identification and treatment measures into quality assurance and improvement efforts, and implementing tobacco-free campus policies in health-care settings and workplaces (5,6).
The findings in this report are subject to at least six limitations. First, questionnaires were administered only in English and Spanish, which might have decreased response rates for populations unable to respond to the survey because of language barriers. Second, small sample sizes for certain populations resulted in less precise estimates. Third, institutionalized populations and persons in the military were not included in the survey, and data on those with military health coverage only reflects dependents of persons on active duty, retirees, those with Veteran's Administration coverage and their dependents with CHAMPVA, which reduces the generalizability of the results to the U.S. population. Fourth, the 2010 NHIS response rate was 60.8%, and lower response rates increase the potential for bias. Fifth, questions regarding counseling only assessed use of each type of counseling and did not assess the content or quality of the counseling (i.e., number and length of sessions, use of problem solving, skills training, and social support). Therefore, determining whether the counseling followed the Public Health Service Clinical Practice Guideline on Treating Tobacco Use and Dependence was not possible (5). Finally, the extent of misclassification of cigarette smoking and cessation-related measures could not be determined because all smoking information was self-reported and not validated by biochemical tests or other means.
Several recent national initiatives have created unprecedented opportunities to increase the number of persons in the United States who quit smoking. The 2010 Patient Protection and Affordable Care Act will expand coverage of smoking cessation treatments substantially.¶ For example, effective October 1, 2010, the Act required state Medicaid programs to provide cessation coverage to pregnant Medicaid enrollees with no cost sharing. The legislation also bars state Medicaid programs from excluding FDA-approved cessation medications, including over-the-counter medications, from Medicaid drug coverage, effective January 1, 2014, and requires non-grandfathered private health plans to offer cessation coverage without cost sharing, effective September 23, 2010. In addition, the Joint Commission, an independent, not-for-profit organization responsible for accreditation of health-care organizations and programs in the United States, has developed new voluntary performance measures for hospitals for assessing and treating tobacco dependence in all hospitalized patients.**
Identification and treatment of tobacco use also are likely to increase among health-care providers who become "meaningful users" of certified electronic health record (EHR) technology. Under the Centers for Medicare and Medicaid Services EHR Incentive Program, participating physicians and hospitals must identify a patient's smoking status, and health-care providers also must implement clinical quality measures on tobacco use assessment and intervention. The Million Hearts initiative††of the U.S. Department of Health and Human Services will continue to support these and other efforts directed at smoking prevention and cessation in communities and health-care systems.
Acknowledgments
Kat Asman, Alissa O'Halloran, Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, CDC
References
- CDC. How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease: a report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, CDC; 2010. Available at http://www.surgeongeneral.gov/library/tobaccosmoke/report/full_report.pdf. Accessed November 7, 2011.
- Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years' observations on male British doctors. BMJ 2004;328:1519--28.
- CDC. Smoking and tobacco use: trends in current cigarette smoking among high school students and adults, United States, 1965--2010. Atlanta, GA: US Department of Health and Human Services, CDC; 2011. Available at http://www.cdc.gov/tobacco/data_statistics/tables/trends/cig_smoking/index.htm. Accessed November 7, 2011.
- CDC. Cigarette smoking among adults---United States, 2002. MMWR 2004:53:427--31.
- Fiore MC, Jaen CR, Baker TB, et al. Treating tobacco use and dependence: 2008 update. Clinical practice guideline. Rockville, MD: US Department of Health and Human Services, Public Health Service; 2008. Available at http://www.surgeongeneral.gov/tobacco/treating_tobacco_use08.pdf. Accessed November 7, 2011.
- Community Guide Task Force on Community Preventive Services. The guide to community preventive services: what works to promote health. Part 1: changing risk behaviors and addressing environmental challenges. Tobacco [Chapter 1]. New York, NY: Oxford University Press; 2005. Available at http://www.thecommunityguide.org/tobacco/tobacco.pdf. Accessed November 7, 2011.
- Shiffman S, Brockwell SE, Pillitteri JL, Gitchell JG. Use of smoking-cessation treatments in the United States. Am J Prev Med 2008;34:102--11.
- Curry SJ, Sporer AK, Pugach O, Campbell RT, Emery S. Use of tobacco cessation treatments among young adult smokers: 2005 National Health Interview Survey. Am J Public Health 2007;97:1464--9.
- CDC. Smoking-attributable mortality, years of potential life lost, and productivity losses---United States, 2000--2004. MMWR 2008;57:1226--8.
- National Institute on Drug Abuse. Research report series: tobacco addiction. Bethesda MD: National Institutes of Health, National Institute on Drug Abuse; 2009. Available at http://drugabuse.gov/researchreports/nicotine/addictive.html. Accessed November 7, 2011.
* Additional information available at http://www.cdc.gov/nchs/nhis/quest_data_related_1997_forward.htm.
† Available at http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=41.
§ Additional information available at http://www.fda.gov/downloads/advisorycommittees/committeesmeetingmaterials/tobaccoproductsscientificadvisorycommittee/ucm269697.pdf.
¶ Additional information available at http://docs.house.gov/energycommerce/ppacacon.pdf.
** Additional information available at http://www.jointcommission.org/tobacco_and_alcohol_measures.
†† Additional information available at http://millionhearts.hhs.gov.
What is already known on this topic?
Quitting smoking is the most important behavioral change a smoker can make to improve his or her health. Cessation counseling and medications improve a smoker's chances of quitting, but these treatments remain underutilized.
What is added by this report?
In 2010, 68.8% of cigarette smokers said they would like to quit smoking, and 52.4% had recently tried to quit. However, 68.3% of the smokers who tried to quit did so without using evidence-based cessation counseling or medications, and only 48.3% of those who had visited a health-care provider in the past year received advice to quit smoking. Only 31.7% had used counseling and/or medications when they tried to quit; 30.0% had used medications, and 5.9% had used counseling.
What are the implications for public health practice?
Health-care providers should consistently and routinely identify tobacco users, advise them to quit, and provide assistance to those engaged in a quit attempt. Population-based interventions that effectively increase cessation also should be implemented, including expanding tobacco cessation quitlines and health-care coverage for cessation treatments.
FIGURE. Percentage of cigarette smokers aged ≥18 years who made a quit attempt* in the past year, by age group --- National Health Interview Survey, United States, 2001--2010
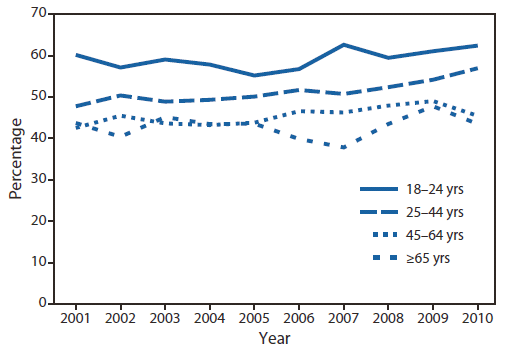
* Current smokers who reported that they stopped smoking for >1 day in the past 12 months because they were trying to quit smoking and former smokers who quit in the past year. Excludes 190 respondents whose smoking status was unknown.
Alternate Text: The figure above shows the percentage of cigarette smokers aged ≥18 years who made a quit attempt in the past year in the United States, during 2001-2010, by age group, according to the National Health Interview Survey. Among smokers aged 45-64 years, a significant linear increase in quit attempts was observed from 2001 to 2010 (p<0.05 for linear trend).
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


