Treatment for TB Disease
There are several treatment regimens recommended in the United States for TB disease. TB treatment can take 4, 6, or 9 months depending on the regimen. TB treatment regimens include
- New4-month Rifapentine-moxifloxacin TB Treatment Regimen
- 6- or 9-month RIPE TB Treatment Regimen
- Treatment of Drug-Susceptible Tuberculosis. Clin Infect Dis, 2016
- Table 3. Doses of Antituberculosis Drugs for Adults and Children
Note: this table is an excerpt from Treatment of Drug-Susceptible Tuberculosis and cites supporting information available in the complete guidelines. - Highlights from the 2016 Treatment of Drug-Susceptible Tuberculosis Guidelines
- Table 3. Doses of Antituberculosis Drugs for Adults and Children
- Treatment of Drug-Susceptible Tuberculosis. Clin Infect Dis, 2016

Shorter regimens help patients complete treatment faster. Healthcare providers can choose the appropriate TB treatment regimen based on drug-susceptibility results, coexisting medical conditions (e.g., HIV, diabetes), and potential for drug-drug interactions. The State TB Control Offices and TB Centers of Excellence for Training, Education, and Medical Consultation can provide additional assistance and support in treating people with TB disease.
Directly observed therapy (DOT) helps patients complete treatment. CDC recommends video DOT (vDOT) as an equivalent alternative to in-person DOT for patients on treatment for TB.
The State TB Control Offices and TB Centers of Excellence for Training, Education, and Medical Consultation can provide additional assistance and support in treating people with TB disease.
TB treatment regimens vary in the duration of the regimen, the types of anti-TB drugs prescribed, and the dose and frequency of the drugs. The regimens described on this webpage are for the treatment of drug-susceptible pulmonary TB disease. For information about the treatment of drug-resistant TB, visit the Drug-Resistant TB webpage.
NewThe 4-month TB treatment regimen consists of
- high-dose daily rifapentine (RPT) with
- moxifloxacin (MOX),
- isoniazid (INH), and
- pyrazinamide (PZA).
The 4-month rifapentine-moxifloxacin regimen has an intensive phase of 2 months, followed by a continuation phase of 2 months and 1 week (total 17 weeks for treatment).
| Intensive Phase | Continuation Phase | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Drugs | Durationa | Frequencyb | Drugs | Durationc | Frequencyb | Total Doses | Commentsd,e | Regimen Effectiveness | ||
| RPT MOX INH PZA | 8 weeks | 7 days/week for 56 doses | RPT MOX INH
|
9 weeks | 7 days/week for 63 doses | 119 | Recommended for people ages 12 and older with body weight at or above 40 kg, with pulmonary TB caused by organisms that are not known or suspected to be drug-resistant, and who have no contraindications to this regimen. | The 4-month rifapentine-moxifloxacin TB treatment regimen is as effective as (noninferior to) the standard daily 6-month regimen in curing drug-susceptible TB disease. | ||
Abbreviations: RPT= rifapentine; MOX= Moxifloxacin; INH = isoniazid; PZA = pyrazinamide
aMust be administered completely within 70 days from treatment initiation. If this target is not met, the patient should be considered to have interrupted therapy and should be managed as described in TB treatment guidelines.
bAt least 5 of 7 weekly doses should be administered under direct observation. Directly observed therapy means that a healthcare worker watches the TB patient swallow each dose of the prescribed drugs. The healthcare worker should ask the patient how he or she is feeling, check the medications before they are taken, ask the patient if he or she is experiencing any side effects, and answer any questions the patient may have. Where local policies, allow, eDOT has been shown to be an acceptable alternative to traditional DOT. Contact your state or local TB control office for more information about eDOT policies and procedures.
cMust be administered within 84 days from intensive phase completion. If this target is not met, the patient should be considered to have interrupted therapy and should be managed as described in TB treatment guidelines.
dPyridoxine (vitamin B6), 25–50 mg/day, should be given with isoniazid to all patients.
eDrugs are administered with food once a day, every day of the week.
CDC developed a checklist resource for healthcare providers and TB programs to ensure the correct timing of testing and monitoring for patients through the 4-month rifapentine-moxifloxacin regimen.
The 6- to 9-month RIPE TB treatment regimens consist of
- Rifampin (RIF),
- Isoniazid (INH),
- Pyrazinamide (PZA), and
- Ethambutol (EMB)
RIPE regimens for treating TB disease have an intensive phase of 2 months, followed by a continuation phase of either 4 or 7 months (total of 6 to 9 months for treatment).
| Intensive Phase | Continuation Phase | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Drugsa | Duration | Frequencyb | Drugs | Duration | Frequencyb,c | Total Doses | Commentsc,d,e,f | Regimen Effectiveness | ||
| INH RIF PZA EMB |
8 weeks | 7 days/week for 56 doses | 5 days/week for 40 doses | INH RIF |
18 weeks | 7 days/week for 126 doses | 5 days/week for 90 doses | 182 to 130 | This is the preferred regimen for patients with newly diagnosed pulmonary TB. |  |
| INH RIF PZA EMB |
8 weeks | 7 days/week for 56 doses | 5 days/week for 40 doses | INH RIF |
18 weeks | 3 times weekly for 54 doses | 110 to 94 | Preferred alternative regimen in situations in which more frequent DOT during continuation phase is difficult to achieve. | ||
| INH RIF PZA EMB |
8 weeks | 3 times weekly for 24 doses | INH RIF |
18 weeks | 3 times weekly for 54 doses | 78 | Use regimen with caution in patients with HIV and/or cavitary disease. Missed doses can lead to treatment failure, relapse, and acquired drug resistance. | |||
| INH RIF PZA EMB |
8 weeks | 7 days/week for 14 doses then twice weekly for 12 dosesg | INH RIF |
18 weeks | 2 times weekly for 36 doses | 62 | Do not use twice-weekly regimens in HIV-infected patients or patients with smear positive and/or cavitary disease. If doses are missed then therapy is equivalent to once weekly, which is inferior. | |||
Abbreviations: INH = isoniazid; RIF = rifampin; PZA = pyrazinamide; EMB = ethambutol; HIV = human immunodeficiency virus
aOther combinations may be appropriate in certain circumstances; additional details are provided in the Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America Clinical Practice Guidelines: Treatment of Drug-Susceptible Tuberculosis.
bWhen directly observed therapy (DOT) is used, drugs may be given 5 days per week and the necessary number of doses adjusted accordingly. Although there are no studies that compare 5 with 7 daily doses, extensive experience indicates this would be an effective practice. DOT should be used when drugs are administered less than 7 days per week.
cBased on expert opinion, patients with cavitation on initial chest radiograph and positive cultures at completion of 2 months of therapy should receive a 7-month (31-week) continuation phase.
dPyridoxine (vitamin B6), 25–50 mg/day, is given with INH to all persons at risk of neuropathy (e.g., pregnant women; breastfeeding infants; persons with HIV; patients with diabetes, alcoholism, malnutrition, or chronic renal failure; or patients with advanced age). For patients with peripheral neuropathy, experts recommend increasing pyridoxine dose to 100 mg/day.
eThe recommended time frame for regimen, in tuberculosis control programs in the United States and in several European countries, is to administer all of the specified number of doses for the intensive phase within 3 months and those for the 4-month continuation phase within 6 months, so that the 6-month regimen is completed within 9 months.
fIn general, TB drugs are administered together, at one dosing so as to achieve maximal peak serum concentrations and to facilitate DOT. Bioavailability of all of the drugs (except for RPT) is greatest when taken on an empty stomach.
gAlternatively, some U.S. TB control programs have administered intensive-phase regimens 5 days per week for 15 doses (3 weeks), then twice weekly for 12 doses.
Note: Use of once-weekly therapy with INH 900 mg and rifapentine 600 mg in the continuation phase is not generally recommended. In uncommon situations where more than once-weekly DOT is difficult to achieve, once-weekly continuation phase therapy with INH 900 mg plus rifapentine 600 mg may be considered for use only in persons without HIV and without cavitation on chest radiography.
Healthcare providers can choose the appropriate TB treatment regimen based on drug-susceptibility results, coexisting medical conditions (e.g., HIV, diabetes), and potential for drug-drug interactions. The State TB Control Offices and TB Centers of Excellence for Training, Education, and Medical Consultation can provide additional assistance and support for treating people with TB disease.
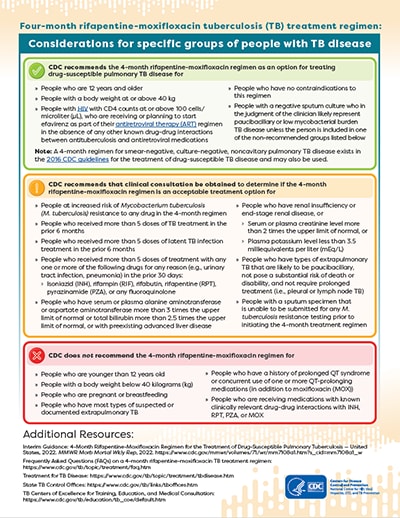
When using the 4-month rifapentine-moxifloxacin regimen as an option to treat people with drug-susceptible pulmonary TB disease, healthcare providers can consider the following information:
CDC recommends the 4-month rifapentine-moxifloxacin regimen as an option for treating pulmonary TB disease caused by organisms that are not known or suspected to be drug-resistant for
- People who are 12 years and older
- People with a body weight at or above 40 kg
- People with HIV with CD4 counts at or above 100 cells/microliter (μL), who are receiving or planning to start efavirenz as part of their antiretroviral therapy (ART) regimen in the absence of any other known drug-drug interactions between antituberculosis and antiretroviral medications
- People who have no contraindications to this regimen
- People with a negative sputum culture who in the judgment of the clinician likely represent paucibacillary or low mycobacterial burden TB disease unless the person is included in one of the non-recommended groups listed below
Note: A 4-month regimen for smear-negative, culture-negative, noncavitary pulmonary TB disease exists in the 2016 Treatment of Drug-Susceptible Tuberculosis Guidelines for the treatment of drug-susceptible TB disease and may also be used.
CDC recommends that clinical consultation be obtained to determine if the 4-month rifapentine-moxifloxacin regimen is an acceptable treatment option for
- People at increased risk of Mycobacterium tuberculosis (M. tuberculosis) resistance to any drug in the 4-month regimen
- People who received more than 5 doses of TB treatment in the prior 6 months
- People who received more than 5 doses of latent TB infection treatment in the prior 6 months
- People who received more than 5 doses of treatment with any one or more of the following drugs for any reason (e.g., urinary tract infection, pneumonia) in the prior 30 days:
- Isoniazid (INH), rifampin (RIF), rifabutin, rifapentine (RPT), pyrazinamide (PZA), or any fluoroquinolone
- People who have serum or plasma alanine aminotransferase or aspartate aminotransferase more than 3 times the upper limit of normal or total bilirubin more than 2.5 times the upper limit of normal, or with preexisting advanced liver disease
- People who have renal insufficiency or end-stage renal disease, or
- Serum or plasma creatinine level more than 2 times the upper limit of normal, or
- Plasma potassium level less than 3.5 milliequivalents per liter (mEq/L)
- People who have types of extrapulmonary TB that are likely to be paucibacillary, not pose a substantial risk of death or disability, and not require prolonged treatment (i.e., pleural or lymph node TB)
- People with a sputum specimen that is unable to be submitted for any M. tuberculosis resistance testing prior to initiating the 4-month treatment regimen

CDC does not recommend the 4-month rifapentine-moxifloxacin regimen for
- People who are younger than 12 years old
- People with a body weight below 40 kilograms (kg)
- People who are pregnant or breastfeeding
- People who have most types of suspected or documented extrapulmonary TB
- People who have a history of prolonged QT syndrome or concurrent use of one or more QT-prolonging medications (in addition to moxifloxacin (MOX))
- People who are receiving medications with known clinically relevant drug-drug interactions with INH, RPT, PZA, or MOX
- People with a baseline M. tuberculosis isolate known or suspected to be resistant to RIF, INH, PZA, or any fluoroquinolone
For additional questions and answers about the 4-month rifapentine-moxifloxacin regimen, visit the Frequently Asked Questions (FAQs) webpage.
The State TB Control Offices and TB Centers of Excellence for Training, Education, and Medical Consultation can provide additional assistance and support in treating people with TB disease.
The 6-month regimen for the treatment of drug-susceptible pulmonary TB can be used in most patients. It consists of four anti-TB drugs and is sometimes called the RIPE regimen because of the medications
- Rifampin
- Isoniazid
- Pyrazinamide
- Ethambutol
CDC recommends the 9-month regimen for the treatment of drug-susceptible pulmonary TB for the following groups:
- People with cavitary pulmonary TB caused by drug-susceptible organisms and whose sputum culture obtained at the time of completion of 2 months of treatment is positive
- People whose intensive phase of treatment did not include pyrazinamide
- People with HIV who are not receiving antiretroviral treatment (ART) during TB treatment
- People being treated with once weekly isoniazid (INH) and rifapentine and whose sputum culture obtained at the time of completion of the intensive phase is positive
(Note: Use of once-weekly therapy with INH 900 mg and rifapentine 600 mg in the continuation phase is not generally recommended. In uncommon situations where more than once-weekly directly observed therapy is difficult to achieve, once-weekly continuation phase therapy with INH 900 mg plus rifapentine 600 mg may be considered for use, but only in persons without HIV and without cavitation on chest radiography.)
Learn more about considerations for
The 4-month TB treatment regimen (high-dose daily rifapentine with moxifloxacin, isoniazid, and pyrazinamide) and 6-month RIPE (rifapentine, isoniazid, pyrazinamide, and ethambutol) regimen have unique considerations. The below table compares the recommended evaluation and testing considerations for the two regimens.
| Evaluation and Testing Considerations | 4-month Rifapentine-moxifloxacin Regimen | Standard 6-month RIPE Regimen |
|---|---|---|
| Rapid molecular testing | At baseline, test at least one specimen using a rapid molecular test. It is advisable to test at least one specimen using a rapid molecular test for susceptibility to
|
At baseline, test at least one specimen using a rapid molecular test. For patients with risk factors for drug-resistant disease, it is recommended to test at least one specimen using a rapid molecular test for susceptibility to
|
| Acid-fast bacilli smear microscopy and culture | At baseline and at minimum monthly intervals until 2 consecutive specimens are negative on culture, test a respiratory specimen for acid-fast bacilli smear microscopy and culture | At baseline and at minimum monthly intervals until 2 consecutive specimens are negative on culture, test a respiratory specimen for acid-fast bacilli smear microscopy and culture |
| Phenotypic drug susceptibility testing | At baseline, obtain phenotypic drug susceptibility at least for the following TB drugs
|
At baseline, obtain phenotypic drug susceptibility for the following TB drugs
|
| Additional tests | Recommended at baseline, obtain blood levels of
|
Not routinely recommended for all patients |
- State TB Control Programs
- TB Centers of Excellence for Training, Education, and Medical Consultation
For People with TB Disease
- TB – General Information (Fact sheet)
- TB Can Be Treated (Fact sheet)
- You Can Prevent TB (Fact sheet)
- Staying on track with TB medicine (Pamphlet) (PDF – 511k)
- Questions and Answers About TB
For Healthcare Providers
- Treatment Fact Sheets
- Treatment of Drug-Susceptible Tuberculosis Disease in Persons Not Infected with HIV
- Treatment of Drug-Resistant Tuberculosis
- Provisional CDC Guidance for the Use of Pretomanid as part of a Regimen [Bedaquiline, Pretomanid, and Linezolid (BPaL)] to Treat Drug-Resistant Tuberculosis Disease
- Treatment Guidelines
- Core Curriculum on Tuberculosis: What the Clinician Should Know
- Frequently Asked Questions (FAQs) on 4-month rifapentine-moxifloxacin TB treatment regimen
- Treatment Regimen Checklist for Healthcare Providers
- Considerations for Specific Groups of People